Achalasia: Understanding Achalasia
Achalasia is a rare condition that affects the esophagus, causing swallowing difficulties. It is characterized by the inability of food to pass through the esophagus and into the stomach. This is due to abnormal muscle contractions. Those with achalasia often face symptoms like dysphagia, regurgitation of food, and chest pain. It’s vital to understand the causes, symptoms, and treatment options. This knowledge is key to managing the condition effectively.
This esophageal disorder can significantly impact an individual’s quality of life. It’s essential to seek medical attention if symptoms persist. Early intervention can make a big difference. Achalasia, a rare esophageal motility disorder, presents unique challenges in diagnosis and treatment. It is essential to comprehend the nature of this condition to provide effective care and management.
Definition and Overview
Achalasia is characterized by the inability of food to pass through the esophagus and into the stomach due to abnormal muscle contractions. This condition results from the degeneration of the nerve cells that control the esophageal muscles.
The esophagus is a muscular tube that carries food from the throat to the stomach. In Achalasia, the muscles and nerves of the esophagus are affected. This leads to a failure of the lower esophageal sphincter (LES) to relax, obstructing food passage.
- Difficulty swallowing both solids and liquids
- Regurgitation of food
- Chest pain
How Common is Achalasia?
Achalasia is considered a rare condition. The estimated incidence is approximately 1 in 100,000 people per year.
It affects men and women equally, typically presenting between the ages of 20 and 40. The prevalence may be higher in certain populations due to genetic factors.
The Esophagus and Its Function
To grasp achalasia, we must first understand the esophagus’s normal function and its role in swallowing. The esophagus is a muscular tube that propels food into the stomach through a process called peristalsis.
Normal Esophageal Function
The esophagus works by using muscular contractions to move food from the mouth to the stomach. This process is facilitated by the coordinated relaxation and contraction of muscles along the esophagus. It ensures that food is efficiently transported.
The lower esophageal sphincter (LES) plays a critical role in this process. It relaxes to allow food to pass into the stomach and then tightens to prevent stomach contents from flowing back into the esophagus.
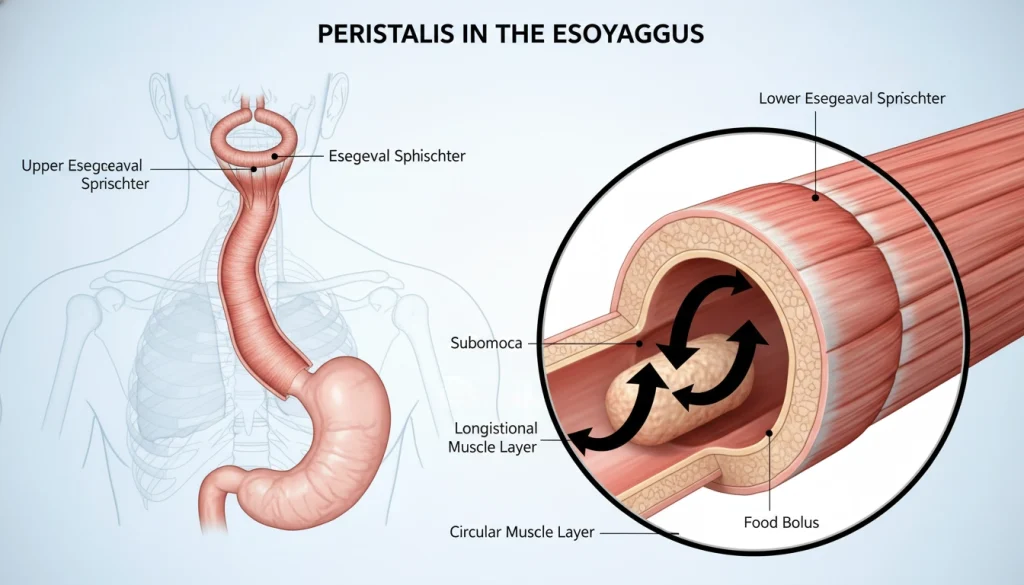
How Achalasia Affects the Esophagus
Achalasia disrupts the esophagus’s normal functioning by affecting the LES’s ability to relax. This impedes the passage of food into the stomach. The condition also often involves abnormal peristalsis, further complicating the swallowing process.
As a result, individuals with achalasia may experience difficulty swallowing, regurgitation of food, and other symptoms. These symptoms significantly impact their quality of life.
Types of Achalasia
Grasping the various forms of achalasia is key to crafting effective treatment strategies. This esophageal disorder is divided into three primary categories, based on manometric findings and esophageal contraction patterns.
Type I Achalasia
Type I achalasia is distinguished by minimal esophageal contractility. It’s often linked with significant esophageal dilation and a lack of pressurization. Patients with Type I achalasia face a more severe form of the disease, with substantial impairment of esophageal function.
Type II Achalasia
Type II achalasia is identified by widespread esophageal pressurization in at least 20% of swallows. This subtype has a better prognosis than Type I, as the esophagus retains some contractility. It’s the most prevalent form of achalasia and generally responds well to treatment.
Type III Achalasia
Type III achalasia, or spastic achalasia, is characterized by premature or spastic contractions in at least 20% of swallows. This type presents a more complex clinical scenario and may necessitate a customized treatment plan due to significant esophageal spasm.
Classification into these three types is critical for managing and treating achalasia. Accurate identification of a patient’s achalasia type is essential for choosing the most suitable therapeutic approach.
Signs and Symptoms of Achalasia
Achalasia, a rare esophageal disorder, shows through various symptoms that greatly affect one’s life quality. It’s vital to recognize these signs early for timely diagnosis and effective treatment.
Common Symptoms
The primary symptoms of Achalasia include difficulty swallowing (dysphagia) and food regurgitation. Dysphagia starts with solids and progresses to liquids, worsening over time.
Regurgitation happens when food stays in the esophagus and returns to the mouth. It can occur shortly after eating or hours later, even during sleep.
Less Common Symptoms
Less common symptoms include chest pain, which might be mistaken for heart problems, and weight loss from poor nutrition. Some may also cough or develop aspiration pneumonia from food or liquids entering the lungs.
How Symptoms Progress Over Time
Achalasia symptoms gradually worsen. Initially, symptoms may be mild, but they intensify and occur more often as the condition progresses.
Understanding how Achalasia symptoms evolve is key to managing the condition. It helps improve the life quality of those affected.
Early detection and treatment are critical in managing Achalasia. This emphasizes the need for awareness and prompt medical consultation.
Causes and Risk Factors
The exact causes of achalasia are not fully understood, but research has uncovered several possible factors. It’s essential to grasp these causes and risk factors to create effective management strategies.
Potential Causes
Achalasia likely stems from a mix of factors affecting the esophagus. The degeneration of neurons in the esophagus is a key factor. This degeneration results in the loss of peristalsis and the inability of the lower esophageal sphincter to relax.
- Neurodegenerative changes
- Autoimmune responses
- Infections
These elements can impair normal esophageal function, contributing to achalasia’s development.
Risk Factors
Several risk factors have been identified that may increase the likelihood of developing achalasia. These include:
- Age: Achalasia is more common in adults between 20 and 40 years old.
- Family history: Having a family history of achalasia may increase the risk.
- Other medical conditions: Certain conditions, such as Chagas disease, may be associated with an increased risk of achalasia.
Genetic Considerations
There is evidence suggesting a genetic component to achalasia, with some families showing a higher incidence. Yet, no specific genetic mutation has been pinpointed as the sole cause.
Research into the genetic aspects of achalasia continues. The aim is to better understand the role of genetics in its development.
Pathophysiology of Achalasia
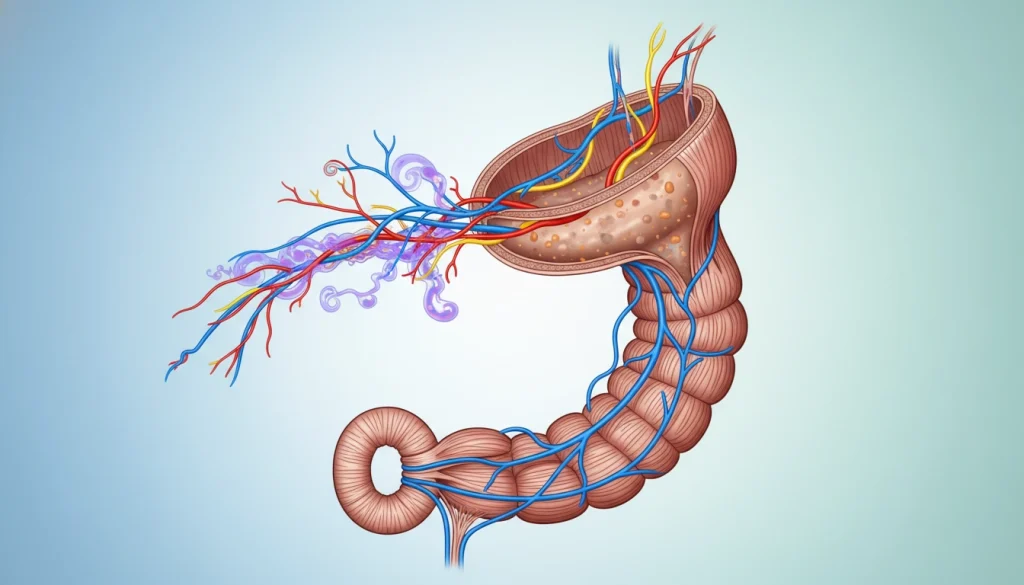
Achalasia’s pathophysiology is complex, involving both neurological and muscular changes in the esophagus. These alterations significantly affect the esophagus’s motility and function. This leads to the hallmark symptoms of achalasia.
Neurological Changes
Achalasia is mainly caused by the degeneration of inhibitory neurons in the esophageal myenteric plexus. This loss disrupts the esophagus’s normal peristaltic movement. The inhibitory neurons are vital for regulating the relaxation of the lower esophageal sphincter (LES).
The degeneration of these neurons causes the LES to fail to relax properly during swallowing. This obstruction prevents food from entering the stomach.
Muscular Changes
Achalasia also involves changes in the esophagus’s muscular layer. The smooth muscle becomes hypertrophied, and its contractility is altered. These muscular changes impair peristalsis, making swallowing even more difficult.
Diagnosing Achalasia
Achalasia diagnosis involves a detailed process, starting with initial assessments and moving to specialized tests. This thorough approach is essential to accurately diagnose the condition and exclude other possible causes of symptoms.
Initial Assessment and Physical Examination
The diagnostic journey for Achalasia begins with a detailed medical history and physical exam. Healthcare providers search for symptoms like dysphagia, regurgitation, and weight loss. They also check for signs of malnutrition or dehydration. This initial step helps identify risk factors and guides further testing.
Barium Swallow Studies
A barium swallow study uses a liquid containing barium to visualize the esophagus through X-rays. It can reveal signs of Achalasia, such as a dilated esophagus and a “bird’s beak” shape at the lower end. This test offers valuable insights into the esophagus’s anatomy and function.
Esophageal Manometry
Esophageal manometry is a critical diagnostic tool for Achalasia. It measures the pressure and coordination of esophageal muscles using a catheter inserted through the nose. Manometry can identify issues like the absence of peristalsis and impaired lower esophageal sphincter relaxation, characteristic of Achalasia.
Endoscopy
Endoscopy is a vital diagnostic tool for suspected Achalasia. A flexible tube with a camera is inserted through the mouth to examine the esophagus. This test helps to exclude other conditions that might cause similar symptoms, like esophageal strictures or tumors.
Other Diagnostic Tests
In some instances, additional tests are ordered to further evaluate the esophagus and rule out other conditions. These might include ambulatory pH monitoring for GERD or CT scans to examine the esophagus and surrounding tissues.
Differential Diagnosis
Diagnosing Achalasia requires ruling out other conditions with similar symptoms, known as differential diagnosis. This is essential because many esophageal and gastrointestinal disorders can mimic Achalasia. Accurate diagnosis is challenging due to these similarities.
Conditions That Mimic Achalasia
Several conditions can mimic Achalasia, including esophageal strictures, diffuse esophageal spasm, and gastroesophageal reflux disease (GERD). Esophageal cancer, often found at the gastroesophageal junction, can also cause symptoms like dysphagia and regurgitation, similar to Achalasia.
Chagas disease, a parasitic infection that damages the esophagus, and certain neurodegenerative diseases can also present with symptoms similar to Achalasia. A thorough diagnostic evaluation is necessary to differentiate Achalasia from these conditions.
Distinguishing Features
Achalasia is characterized by specific manometric findings, such as aperistalsis in the esophageal body and impaired LES relaxation.Barium swallow studies may reveal a dilated esophagus with a “bird’s beak” appearance, typical but not exclusive to Achalasia.
Endoscopy and other diagnostic tests help exclude other causes of dysphagia, like strictures or tumors. By combining clinical presentation, diagnostic imaging, and manometry results, healthcare providers can accurately diagnose Achalasia and distinguish it from other conditions.
Non-Surgical Treatment Options
Managing Achalasia involves several non-surgical methods, each with its own set of benefits and drawbacks. These treatments aim to ease symptoms, enhance quality of life, and sidestep surgery’s risks.
Medications
Medications are often the first choice for treating Achalasia. They include calcium channel blockers and nitrates, which relax the esophageal muscles. This makes it easier for food to move through. Though they offer relief, their effectiveness can decrease over time. They may not be right for everyone due to possible side effects.
Botulinum Toxin (Botox) Injections
Botox injections are another non-surgical option. Injected into the lower esophageal sphincter, Botox weakens the muscle, aiding food passage. It’s beneficial for those not suited for invasive procedures or as a temporary fix. Yet, the effects are not permanent, and repeated injections are often needed. There’s also a risk of developing antibodies against Botox, which can reduce its effectiveness over time.
Pneumatic Dilation
Pneumatic dilation uses a balloon to stretch the lower esophageal sphincter. It’s a more lasting solution than medications and Botox injections. The procedure involves inflating a balloon in the sphincter to widen it, improving esophageal emptying. Though effective, there’s a risk of esophageal perforation, a serious issue that requires immediate medical care.
Each non-surgical treatment has its role in managing Achalasia. The choice depends on the patient’s condition, health, and preferences. A healthcare provider can guide in selecting the most suitable treatment plan.
Surgical Treatment Options
For those with Achalasia, surgery presents a viable solution to ease symptoms. Surgical interventions are considered when other treatments fail to provide relief. The choice of procedure depends on symptom severity, patient health, and the surgeon’s expertise.
Heller Myotomy
Heller myotomy involves a longitudinal incision in the lower esophagus’s muscles, including the lower esophageal sphincter. This aims to enhance food passage into the stomach. It’s a widely used and effective treatment for Achalasia.
The procedure can be laparoscopic, which is less invasive and leads to quicker recovery. It’s often paired with partial fundoplication to manage reflux.
Peroral Endoscopic Myotomy (POEM)
POEM is a newer, minimally invasive method. It makes an incision in the esophageal mucosa to divide the muscle fibers of the lower esophageal sphincter. This is done endoscopically, avoiding external cuts.
POEM’s benefits include less invasiveness, potentially quicker recovery, and less scarring. Yet, it requires specialized skills and tools.
Esophagectomy
In severe cases, esophagectomy might be considered. This involves removing the esophagus and reconstructing it. It’s a complex procedure, usually for advanced disease or treatment failures.
Esophagectomy is a more radical option, typically for severe or refractory cases.
Comparing Surgical Approaches
Heller myotomy and POEM are effective but differ in invasiveness and skill requirements. Esophagectomy is a more radical option, usually for severe or refractory cases.
The choice among these options should be based on individual patient factors. This includes the severity of Achalasia, overall health, and personal preferences. Consultation with a healthcare provider is essential.
Complications of Achalasia
Complications from Achalasia can severely affect a patient’s quality of life. If not treated, Achalasia can cause several serious health problems.
Aspiration Pneumonia
Achalasia raises the risk of aspiration pneumonia due to food regurgitation into the lungs. This happens when food is inhaled into the lungs, potentially causing infection.
- Symptoms include coughing and difficulty breathing.
- Aspiration pneumonia can be life-threatening, mainly in older adults.
- Prompt medical attention is necessary if symptoms persist.
Esophageal Cancer Risk
Patients with long-standing Achalasia face a higher risk of esophageal cancer. The chronic dilation of the esophagus may contribute to this risk.
Regular monitoring is essential for early detection.
Malnutrition and Weight Loss
Dysphagia from Achalasia can lead to malnutrition and significant weight loss. Patients may find it hard to consume enough nutrients.
Dietary adjustments and nutritional supplements can help manage these issues.
Psychological Impact
The chronic nature of Achalasia and its effects on eating can cause psychological distress. This includes anxiety and depression.
- Support from healthcare professionals is vital.
- Patients may benefit from counseling or support groups.
Living with Achalasia
Managing achalasia requires a holistic approach, encompassing dietary changes, lifestyle adjustments, and long-term management strategies. Those with achalasia must adapt their daily routines to effectively manage symptoms and enhance their quality of life.
Dietary Modifications
Dietary adjustments are key in managing achalasia. Patients are often advised to consume smaller, more frequent meals to ease esophageal strain. Soft or liquid diets are recommended to facilitate easier swallowing. It’s also beneficial to avoid foods that can worsen symptoms, such as spicy or fatty foods.

Lifestyle Adjustments
Lifestyle adjustments are equally critical in managing achalasia. Elevating the bed’s head can help prevent food from flowing back up into the throat. Avoiding meals before bedtime and taking a walk after eating can also alleviate symptoms. Maintaining a healthy weight and wearing loose clothing can further reduce stomach pressure.
Long-term Management
Effective long-term management of achalasia involves regular check-ups with healthcare providers. These appointments are essential for monitoring the condition and adjusting treatment plans as needed. Periodic tests, such as esophageal manometry or endoscopy, may be required to assess esophageal function and detect complications early.
Support Resources
Support resources are indispensable for those living with achalasia. Joining support groups, whether online or in-person, offers emotional support and practical advice from peers. Healthcare providers can also provide guidance on managing the condition and recommend additional resources as needed.
When to See a Doctor
Understanding when to seek medical help is vital for managing Achalasia. It’s essential for those with this condition to recognize the signs that require professional attention.
Warning Signs
Several warning signs indicate the need for a doctor’s visit. These include:
- Difficulty swallowing both liquids and solids
- Regurgitation of food
- Chest pain or discomfort
- Weight loss due to difficulty eating
If you experience any of these symptoms, it’s essential to consult with your healthcare provider.
Emergency Situations
Certain situations require immediate medical attention. These emergencies include:
- Severe chest pain
- Difficulty breathing
- Severe regurgitation with risk of aspiration
If you’re experiencing any of these emergency situations, seek immediate care at an emergency room or call emergency services.
Conclusion
Achalasia is a rare esophageal disorder that makes swallowing difficult, leading to food regurgitation and chest pain. It’s essential to grasp the symptoms, causes, and treatment options to manage it effectively.
Diagnosing Achalasia involves several tests, including barium swallow studies, esophageal manometry, and endoscopy. Treatment options span from medications and botulinum toxin injections to pneumatic dilation and surgeries like Heller myotomy and peroral endoscopic myotomy (POEM).
For those with Achalasia, maintaining esophageal health is key. This includes making dietary changes, adjusting lifestyle habits, and adopting long-term management strategies. Understanding Achalasia and its treatments helps individuals manage their condition better, improving their quality of life.
Effective Achalasia management requires a holistic approach. This includes using the latest treatment options and focusing on esophageal health. Such an approach helps alleviate symptoms and prevents complications.
FAQ
Q: What is achalasia?
A: Achalasia is a rare esophageal disorder. It makes swallowing hard because the esophagus can’t push food into the stomach.
Q: What are the symptoms of achalasia?
A: Common symptoms include trouble swallowing and food coming back up. You might also feel chest pain and lose weight.
Q: How is achalasia diagnosed?
A: Doctors use tests like barium swallow studies and esophageal manometry. Endoscopy is also used to diagnose achalasia.
Q: What are the treatment options for achalasia?
A: Treatments include medications and Botox injections. Other options are pneumatic dilation, Heller myotomy, and Peroral Endoscopic Myotomy (POEM). Esophagectomy is also considered.
Q: Can achalasia be cured?
A: There’s no cure for achalasia. But, treatments can help manage symptoms and improve life quality.
Q: What are the complications of untreated achalasia?
A: Untreated achalasia can cause serious problems. These include aspiration pneumonia, esophageal cancer, malnutrition, and weight loss.
Q: How can I manage achalasia?
A: Managing achalasia involves making dietary changes and adjusting your lifestyle. It’s also important to seek support from healthcare professionals and support groups.
Q: When should I see a doctor for achalasia symptoms?
A: If you have trouble swallowing, chest pain, or food coming back up, see a doctor. These symptoms could be signs of achalasia or other serious issues.