Anesthesia in Children: Types of Anesthesia Used in Pediatric Care
Administering pediatric anesthesia demands a profound grasp of the distinct physiological traits of young patients. This knowledge is critical for tailoring care to meet their specific needs. Healthcare professionals must weigh numerous factors to guarantee anesthesia safety during medical procedures. This includes understanding the child’s age, weight, and overall health.
The process of administering children anesthesia is meticulous. It involves careful planning, precise dosing, and continuous monitoring to minimize risks. This approach ensures the child’s safety and comfort throughout the procedure. By grasping the unique requirements of pediatric patients, healthcare providers can enhance anesthesia care. This leads to better outcomes and a more positive experience for the young patients.
The Unique Physiology of Pediatric Patients
For anesthesiologists, grasping the unique physiology of pediatric patients is essential. It ensures safe and effective care. Pediatric patients show distinct physiological traits, differing from adults. This necessitates specialized knowledge for anesthesia management.
Anatomical Differences
Pediatric patients have anatomical variations that affect anesthesia care. These include differences in airway anatomy and the cardiovascular system.
Airway Anatomy Variations
Children have a larger tongue compared to their mouth size. Their larynx is higher and more forward, and their cricoid ring is narrower than adults’. These factors complicate airway management.
Cardiovascular System Particularities
The cardiovascular system in children has a higher heart rate and lower blood pressure than adults. This affects how anesthetics are administered and managed.
Metabolic Considerations
Children have a higher metabolic rate and different glucose homeostasis than adults. This impacts anesthesia management.
Higher Metabolic Rate Impact
Children’s higher metabolic rate means they consume oxygen and produce carbon dioxide faster. This influences ventilation strategies during anesthesia.
Glucose Homeostasis
Children’s glucose levels can fluctuate rapidly due to their higher metabolic rate and limited glycogen stores. This requires careful glucose monitoring.
Respiratory System Variations
- Differences in oxygen consumption
- Respiratory reserve limitations
Oxygen Consumption Differences
Children consume more oxygen relative to their body size than adults. This affects ventilation during anesthesia.
Respiratory Reserve Limitations
Pediatric patients have a smaller functional residual capacity. This makes them more susceptible to hypoxia during anesthesia induction.
Types of Anesthesia Used in Pediatric Care
Anesthesia for pediatric patients involves a variety of techniques, each tailored to their specific needs. The choice of anesthesia depends on the procedure type, the child’s age and health, and the anesthesiologist’s preference.
General Anesthesia
General anesthesia is often used for surgeries requiring the child to be completely unconscious. It can be administered through inhalational or intravenous agents.
Inhalational Agents
Inhalational agents, such as sevoflurane, are favored for pediatric anesthesia due to their safety and ease of use.
Intravenous Agents
Intravenous agents, including propofol and ketamine, offer quick induction and recovery. They are commonly used in combination with other anesthetics.
Regional Anesthesia
Regional anesthesia numbs a specific body region. It’s an effective alternative to general anesthesia for certain procedures.
Neuraxial Blocks
Neuraxial blocks, such as epidural and spinal anesthesia, are used for lower abdominal and lower limb surgeries.
Peripheral Nerve Blocks
Peripheral nerve blocks target specific nerves to provide pain relief for the affected limb or region.
Sedation Options
Sedation is used for less invasive procedures, providing a range of options from minimal to deep sedation.
Minimal Sedation
Minimal sedation involves the use of anxiolytics to relax the child without impairing their ability to respond to verbal commands.
Moderate and Deep Sedation
Moderate sedation results in a depressed level of consciousness. Deep sedation is characterized by a more profound depression, potentially requiring airway management.
Local Anesthesia Applications
Local anesthesia is used for minor procedures, providing pain relief without the need for systemic anesthetics.
Topical Anesthetics
Topical anesthetics, such as lidocaine cream, are applied directly to the skin to numb the area.
Infiltration Techniques
Infiltration techniques involve injecting local anesthetic into the tissue surrounding the surgical site.
The various types of anesthesia used in pediatric care offer a range of options for managing pain and anxiety in children. By understanding the different techniques available, healthcare providers can tailor their approach to meet the unique needs of each child.
- General anesthesia is used for major surgeries.
- Regional anesthesia provides pain relief for specific regions.
- Sedation is used for less invasive procedures.
- Local anesthesia is applied for minor procedures.
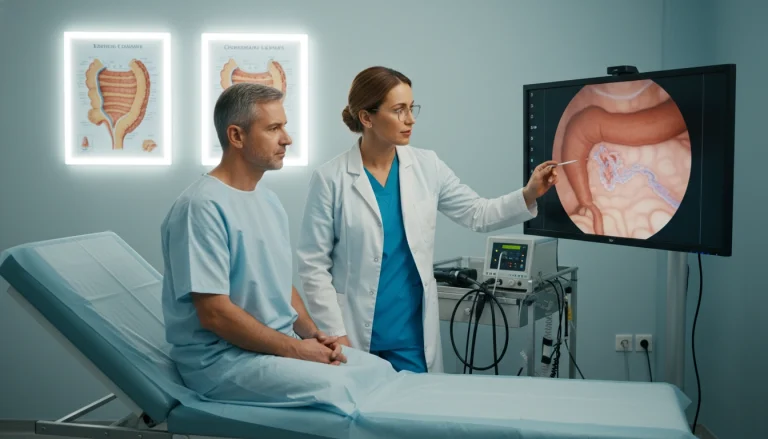
Pre-Anesthetic Assessment for Children
The pre-anesthetic assessment phase is vital in pediatric anesthesia care. It aids in planning the right anesthetic strategy. This detailed evaluation aims to spot risks and craft a customized anesthetic plan.
Medical History Evaluation
Thoroughly reviewing a child’s medical history is key. It involves looking at past anesthetic experiences and family health. This gives insights into possible anesthetic issues.
Previous Anesthetic Experiences
Knowing a child’s past with anesthesia helps predict future challenges. It guides in making necessary preparations.
Family History Significance
A family history of anesthetic problems is significant. It hints at genetic factors that might affect anesthesia.
Physical Examination Protocols
A physical exam is a core part of the pre-anesthetic check-up. It focuses on the child’s airway and heart health.
Airway Assessment
Checking the child’s airway is essential. It helps predict any intubation difficulties.
Cardiovascular Evaluation
Examining the heart is vital. It uncovers any heart issues that could affect anesthesia.
Laboratory Testing Requirements
Labs are ordered based on the child’s age and health. Tests vary by age and medical condition. This ensures a complete assessment.
Age-Specific Testing
Lab tests differ with the child’s age. Each age group has specific needs.
Condition-Specific Testing
Some medical conditions require extra or specialized tests. This ensures safe anesthesia management.
Preparing Children for Anesthesia
Preparing children for anesthesia requires a blend of age-appropriate communication, psychological preparation, and strict adherence to guidelines. This approach is key to reducing anxiety and ensuring the child’s safety and comfort during medical procedures.
Age-Appropriate Communication
It’s essential to communicate with children in a way that matches their age. Using simple language and visual aids can help explain the procedure they will undergo.
Using Play Therapy
Play therapy is a valuable tool for helping children grasp and cope with the anesthesia process.
Visual Aids and Demonstrations
Visual aids and demonstrations can significantly reduce anxiety. They provide a clear understanding of what to expect during the procedure.
Psychological Preparation
Psychological preparation is a critical aspect. Techniques like anxiety reduction and the involvement of child life specialists are vital.
Anxiety Reduction Techniques
Several methods can be used to reduce anxiety. These include relaxation techniques and distractions.
Child Life Specialist Role
Child life specialists are trained professionals. They help children navigate the medical environment.
Fasting Guidelines
Following fasting guidelines is essential for the child’s safety during anesthesia.
Clear Liquid Allowances
It’s important to understand what clear liquids are allowed and when.
Age-Based Fasting Times
Fasting times vary based on the child’s age. It’s critical to follow specific guidelines.
Parental Involvement in Anesthetic Care
Parents are key in their child’s anesthetic care, from preparation to recovery. Their involvement is invaluable. It enhances the child’s comfort and safety, and supports the medical team in delivering top-notch care.
Education and Informed Consent
Education and informed consent are essential for parental involvement. Parents need to understand the anesthetic process fully, including risks and benefits.
Risk Communication
Clear communication about risks is vital. It helps parents grasp what to expect and make informed decisions about their child’s care.
Expectation Management
Managing expectations is critical. It reduces anxiety and ensures parents are ready for the procedure and recovery.
Presence During Induction
Parents being present during induction can comfort and reassure the child.
Benefits and Considerations
While parental presence is comforting, its impact on parents must be considered. It’s important to ensure they are prepared.
Parental Preparation
Preparing parents for induction is vital. They need to know what to expect, including sights, sounds, and their child’s reactions.

Post-operative Support Role
Post-operatively, parents are critical in supporting their child’s recovery. They manage pain and monitor for complications.
Pain Management Assistance
Parents can help with pain management. They follow the medical team’s advice on medication and comfort measures.
Monitoring for Complications
Parents are also vital in monitoring for complications. They watch for unusual bleeding, respiratory issues, or signs of infection.
Anesthesia in Children: Induction Techniques
In pediatric anesthesia, the right induction technique is key to a successful procedure and the child’s comfort. The choice of method depends on the child’s age, medical history, and the surgery type.
Inhalational Induction
Inhalational induction is a common technique in pediatric anesthesia. It uses anesthetic gases to induce unconsciousness.
Agent Selection
Choosing the right inhalational agent is critical. Sevoflurane is often chosen for its rapid onset and minimal airway irritation.
Mask Techniques
Proper mask technique is vital for successful inhalational induction. The mask must fit snugly to prevent leaks.
Intravenous Induction
Intravenous induction is used in older children or those with certain medical conditions in pediatric anesthesia.
Vascular Access Challenges
One challenge of intravenous induction is obtaining vascular access in children. This is due to their small vein size.
Medication Dosing
Accurate dosing of anesthetic medications is essential. For more information on managing pediatric patients with complex conditions, visit Acibadem International.
Rapid Sequence Induction
Rapid sequence induction is used in emergency surgeries or when there’s a high risk of aspiration.
Indications in Pediatrics
In pediatric patients, rapid sequence induction is indicated for quick airway securing.
Modified Approaches
Modified rapid sequence induction techniques may be used for pediatric patients’ unique needs.
Distraction Techniques
Distraction techniques can reduce anxiety during induction. These include technology-based distractions and comfort items.
Technology-Based Distractions
Tablets or virtual reality devices can distract children during induction, making it less stressful.
Comfort Items
Allowing children to bring a favorite toy or blanket can provide comfort during induction.
The key to successful induction in pediatric anesthesia is tailoring the technique to the individual child’s needs. This ensures a smooth and safe procedure.
- Inhalational induction is often used in pediatric anesthesia due to its non-invasive nature.
- Intravenous induction requires careful vascular access and medication dosing.
- Rapid sequence induction is used in emergency situations or when there’s a high risk of aspiration.
- Distraction techniques can significantly reduce anxiety during induction.
Airway Management in Pediatric Anesthesia
Pediatric airway management is a complex field, demanding specialized knowledge and tools. It’s vital for the safety and comfort of children undergoing anesthesia. Ensuring a secure airway is critical.
Equipment Selection
Choosing the right equipment is key in pediatric airway management. It involves determining the correct size of airway devices and using specialized pediatric tools.
Size Calculations
Accurate size calculations are essential for a proper fit. Formulas and guidelines help determine the right size of endotracheal tubes and other devices.
Specialized Pediatric Devices
Pediatric anesthesia often requires specialized devices. These are designed for the unique anatomy of children, including pediatric-sized laryngoscope blades and endotracheal tubes.
Difficult Airway Anticipation
Anticipating a difficult airway is a critical step in pediatric anesthesia. It involves assessing risk factors and preparing strategies.
Risk Assessment Tools
Various tools and assessments help predict airway difficulties. These include evaluating the child’s medical history, anatomical features, and other factors.
Preparation Strategies
Having a well-planned strategy is essential for managing a difficult airway. This may involve having alternative airway devices available and a team prepared for complications.
Intubation Techniques
The technique used for intubation in pediatric patients is critical. It significantly impacts the success and safety of the procedure.
Direct vs. Video Laryngoscopy
Both direct and video laryngoscopy have their place in pediatric intubation. The choice depends on the situation and the anesthesiologist’s expertise.
Supraglottic Airway Devices
Supraglottic airway devices offer an alternative to endotracheal intubation. They are useful in situations where intubation is challenging or not necessary.
Effective airway management in pediatric anesthesia requires knowledge, skill, and the right equipment. Understanding the unique challenges and using appropriate techniques ensures the best outcomes for young patients.
Monitoring During Pediatric Anesthesia
Ensuring the safety and well-being of children during surgical procedures is critical. This requires a blend of standard and advanced monitoring techniques. These methods are tailored to meet the unique needs of pediatric patients.
Standard Monitoring Parameters
Standard monitoring parameters are vital for assessing children’s vital signs and overall condition under anesthesia. These include:
- Heart rate and rhythm
- Blood pressure
- Oxygen saturation
- End-tidal CO2
Vital Signs Interpretation
Understanding age-related normal values is key to interpreting vital signs in pediatric patients. Recognizing deviations from these norms is also essential.
End-Tidal CO2 Monitoring
End-tidal CO2 monitoring is critical. It assesses ventilation and detects issues like respiratory depression or equipment malfunction.
Advanced Monitoring Techniques
Advanced techniques offer deeper insights into anesthesia depth and neuromuscular function. They complement standard monitoring.
Depth of Anesthesia Monitoring
Monitoring anesthesia depth prevents awareness during surgery and excessive anesthesia.
Neuromuscular Monitoring
Neuromuscular monitoring is vital for managing neuromuscular blockade. It ensures adequate recovery before extubation.
Age-Specific Considerations
Pediatric anesthesia monitoring must be tailored to the child’s age and developmental stage.
Neonatal Monitoring Challenges
Monitoring neonates is challenging due to their small size and fragile physiology.
Equipment Adaptations
Monitoring equipment must be appropriately sized and calibrated for pediatric patients.
Combining standard and advanced monitoring techniques with age-specific considerations ensures safe anesthesia administration to children.
Pharmacology of Pediatric Anesthetic Agents
Understanding the pharmacology of anesthetic agents is key to safe and effective anesthesia in children. The unique physiology of pediatric patients demands careful consideration of various pharmacological factors.
Dosing Principles
Dosing principles in pediatric anesthesia are based on the child’s weight and age. Accurate calculations are essential to avoid underdosing or overdosing.
Weight-Based Calculations
Weight-based calculations are the most common method in pediatric anesthesia. This method ensures the dose is proportional to the child’s size.
Body Surface Area Considerations
In some cases, body surface area (BSA) is used to calculate doses, mainly for medications with a narrow therapeutic index. BSA calculations provide a more accurate estimate of the child’s metabolic capacity.
Commonly Used Medications
Pediatric anesthesia involves various medications, each with specific roles.
Induction Agents
- Propofol is commonly used for induction due to its rapid onset and recovery profile.
- Etomidate is another option, mainly in patients with cardiovascular instability.
Maintenance Agents
- Sevoflurane is a popular choice for maintenance due to its favorable pharmacokinetic profile.
- Isoflurane is also used, mainly in older children.
Pharmacokinetic Differences
Children exhibit different pharmacokinetic profiles compared to adults, affecting how anesthetic agents are distributed and cleared.
Distribution Volume Variations
The distribution volume of anesthetic agents can vary significantly in children due to differences in body composition.
Clearance Rate Differences
Children generally have a higher clearance rate for many anesthetic agents, requiring adjusted dosing strategies.
Adjunctive Medications
Adjunctive medications play a critical role in managing pain and preventing postoperative nausea and vomiting.
Analgesics
- Fentanyl is commonly used for pain management due to its potency and rapid onset.
- Acetaminophen is also used for mild to moderate pain.
Antiemetics
- Ondansetron is a popular choice for preventing postoperative nausea and vomiting.
- Dexamethasone is also used for its antiemetic properties.
Managing Fluid and Blood Loss in Children
Effective fluid management and blood loss estimation are key in pediatric anesthesia. Children undergoing surgery need careful fluid status and blood loss management. This ensures their safety and the best possible outcomes.
Calculating Fluid Requirements
Calculating fluid needs in children involves two parts: maintenance and deficit replacement.
Maintenance Needs
Maintenance fluid needs are based on the child’s weight. Different rates apply to different weight ranges.
Deficit Replacement
Deficit replacement estimates and replaces fluids lost due to fasting and surgery.
Blood Loss Estimation
Estimating blood loss in pediatric patients combines visual assessment and laboratory monitoring.
Visual Assessment Techniques
Visual assessment estimates blood loss by observing suction containers and surgical sponges.
Laboratory Monitoring
Laboratory monitoring uses serial hemoglobin or hematocrit measurements to assess blood loss impact.
Transfusion Thresholds
Understanding transfusion thresholds is vital for managing significant blood loss in children.
Age-Specific Hemoglobin Targets
Transfusion thresholds vary by age. Different hemoglobin targets apply to neonates, infants, and older children.
Component Therapy Selection
Selecting the right blood component for transfusion depends on the clinical context and patient needs.

Temperature Regulation During Pediatric Procedures
Keeping a stable body temperature is key during pediatric surgeries. Children’s ability to regulate their body temperature is not as developed as adults’. This makes them more prone to temperature changes.
Preventing Hypothermia
Hypothermia is a big risk for kids due to their high surface area to weight ratio. The cold of the operating room also plays a role.
Risk Factors in Children
- Young age
- Low body weight
- Prolonged exposure to cold environments
- Certain medical conditions
Preventive Strategies
To prevent hypothermia, several strategies are used. These include pre-warming, using warm blankets, and keeping the operating room warm.
Warming Techniques
Warming techniques are critical to keep pediatric patients at a normal temperature during procedures.
Passive Warming Methods
- Using warm blankets
- Insulating the patient with drapes
Active Warming Devices
Active warming devices, like forced-air warming systems, are very effective in keeping patient temperatures stable.
Temperature Monitoring
It’s essential to continuously monitor temperature to catch any temperature changes quickly.
Monitoring Site Selection
The choice of where to monitor temperature can impact accuracy. Common spots include the esophagus, rectum, and bladder.
Continuous vs. Intermittent Monitoring
Continuous monitoring offers real-time data. This allows for quick action if temperature issues arise.
Common Complications in Pediatric Anesthesia
Pediatric anesthesia is generally safe but can lead to complications that require careful management. Anesthesiologists must be vigilant and prepared to address these issues promptly. This ensures the best outcomes for young patients.
Respiratory Events
Respiratory complications are common in pediatric anesthesia. Two significant events are laryngospasm and bronchospasm.
Laryngospasm
Laryngospasm is a sudden, severe constriction of the vocal cords, causing airway obstruction. It’s more common in children due to their smaller airway diameter and higher reactivity.
Bronchospasm
Bronchospasm involves the constriction of the airways, making ventilation difficult. It’s often seen in children with asthma or respiratory infections.
Cardiovascular Complications
Cardiovascular issues, such as bradycardia and hypotension, can arise during pediatric anesthesia.
Bradycardia
Bradycardia, or an abnormally slow heart rate, can lead to decreased cardiac output. It’s often managed with atropine.
Hypotension
Hypotension, or low blood pressure, can result from various factors, including anesthetic agents and blood loss. It requires prompt treatment to maintain adequate perfusion of vital organs.
Emergence Delirium
Emergence delirium is a state of agitation and confusion that can occur as the child emerges from anesthesia. It’s a significant concern due to its distressing nature and injury risk.
Risk Factors
Risk factors for emergence delirium include young age, type of surgery, and the use of certain anesthetic agents. For more information on managing such conditions, visit Acıbadem International for insights into pediatric care.
Management Strategies
Management strategies include the use of sedatives, maintaining a calm environment, and involving parents in the recovery process.
Postoperative Nausea and Vomiting
Postoperative nausea and vomiting (PONV) are common complications that can lead to dehydration and electrolyte imbalances.
Prophylaxis Approaches
Prophylaxis approaches include the use of antiemetic medications and ensuring adequate hydration.
Treatment Options
Treatment options for PONV involve administering antiemetics and providing supportive care.
Special Considerations for Different Age Groups
Age-specific considerations are vital for safe and effective anesthesia in pediatric patients. Children’s unique physiological traits and developmental stages require tailored anesthetic strategies. This ensures the best outcomes for each age group.
Neonatal Anesthesia
Neonates face significant challenges due to their physiological immaturity. Key factors include physiologic instability and medication sensitivities. These factors are critical in neonatal anesthesia.
Physiologic Instability
Neonates have limited physiological reserve, making them prone to hemodynamic instability. Close monitoring and careful management of fluids and vasoactive medications are essential.
Medication Sensitivities
The immature liver and kidneys in neonates affect drug metabolism and excretion. This can lead to increased sensitivity and prolonged drug action. Dose adjustments and careful medication selection are critical.
Infant Anesthesia
Infants, from one month to one year, have unique anesthetic considerations. Key factors include the risk of rapid desaturation and temperature vulnerability.
Rapid Desaturation Risk
Infants have a higher metabolic rate and less functional residual capacity. This makes them prone to rapid desaturation during anesthesia induction. Pre-oxygenation and gentle induction techniques are vital.
Temperature Vulnerability
Infants are at risk of hypothermia due to their high surface area to volume ratio. Maintaining a warm operating room environment and using warming devices are important strategies.
Toddler and Preschool Considerations
Toddlers and preschoolers require special attention due to their unique behavioral and psychological needs. Separation anxiety and behavioral management are significant considerations.
Separation Anxiety
Young children may experience distress when separated from their parents. Strategies such as parental presence during induction and gentle, child-friendly communication can help alleviate this anxiety.
Behavioral Management
Effective behavioral management involves creating a calm and reassuring environment. Techniques such as distraction and the use of child-friendly language can facilitate a smoother anesthetic experience.
School-Age and Adolescent Patients
Older children and adolescents have different needs. These include considerations for autonomy and assent, as well as addressing developmental concerns.
Autonomy and Assent
School-age children and adolescents should be involved in the decision-making process. Explanations should be tailored to their level of understanding. Obtaining assent is an important aspect of respecting their autonomy.
Developmental Concerns
This age group may have specific developmental concerns. These include anxiety or previous traumatic experiences. Appropriate preoperative preparation and support are necessary.
Anesthesia for Children with Special Healthcare Needs
Children with special healthcare needs require a customized approach to anesthesia. Their complex medical conditions demand careful planning and consideration. This ensures safe and effective anesthetic care.
Congenital Heart Disease
Congenital heart disease is a critical factor in pediatric anesthesia. Children with these conditions need precise hemodynamic management.
Cyanotic vs. Acyanotic Lesions
Cyanotic lesions, leading to lower oxygen saturation, demand different management strategies than acyanotic lesions. It’s essential to understand the child’s heart condition’s specific anatomy and physiology.
Hemodynamic Management
Hemodynamic management focuses on maintaining optimal blood pressure and cardiac output. Specific medications and careful monitoring are often required during the procedure.
Respiratory Disorders
Respiratory disorders, such as asthma and cystic fibrosis, pose unique challenges for anesthesiologists. Preoperative assessment and optimization of respiratory function are critical.
Asthma
Children with asthma need careful management to prevent bronchospasm during anesthesia. This may involve bronchodilators and avoiding triggers.
Cystic Fibrosis
Cystic fibrosis patients often have thick secretions, requiring aggressive pulmonary toilet. Understanding their respiratory status and having the right equipment available is vital.
Neuromuscular Conditions
Neuromuscular conditions can increase the risk of malignant hyperthermia and may require postoperative ventilation. Careful preoperative evaluation is necessary to anticipate these risks.
Malignant Hyperthermia Risk
Certain neuromuscular conditions are associated with a higher risk of malignant hyperthermia, a potentially life-threatening condition. Being prepared with dantrolene and having a plan in place is essential.
Postoperative Ventilation Needs
Children with neuromuscular conditions may require postoperative ventilation due to respiratory muscle weakness. Planning for postoperative care is critical.
Genetic Syndromes
Genetic syndromes, such as Down syndrome and mucopolysaccharidoses, have unique anesthetic considerations. Understanding the associated anatomical and physiological abnormalities is key to providing safe care.
Down Syndrome
Children with Down syndrome may have associated cardiac defects and airway challenges. Preoperative evaluation should include assessment of these issues.
Mucopolysaccharidoses
Mucopolysaccharidoses can lead to significant airway and cardiac complications. Anticipating these challenges and having the right equipment and expertise available is vital.
Future Directions in Pediatric Anesthesia Safety
The field of pediatric anesthesia is constantly evolving. This is due to ongoing research and advancements aimed at improving safety protocols. As medical technology and our understanding of pediatric physiology grow, new anesthetic agents and monitoring techniques are being developed. These are designed to meet the unique needs of children.
Looking ahead, the adoption of more sophisticated monitoring systems and the development of safer anesthetic drugs are key. A multidisciplinary approach will remain essential. It ensures that anesthesiologists stay current with the latest guidelines and research findings.
By focusing on pediatric anesthesia safety and exploring new directions, healthcare providers can work together. This collaboration is vital in minimizing risks and improving outcomes for children undergoing surgical procedures. It’s a critical step in advancing the field and ensuring the best possible care for young patients.
FAQ
Q: What are the unique physiological characteristics of pediatric patients that affect anesthesia?
A: Pediatric patients have distinct anatomical, metabolic, and respiratory system variations. These differences are significant and require special consideration from anesthesiologists.
Q: What types of anesthesia are used in pediatric care?
A: Various types of anesthesia are used, including general anesthesia, regional anesthesia, sedation options, and local anesthesia applications. Each has specific applications and considerations.
Q: How is pre-anesthetic assessment conducted for children?
A: Pre-anesthetic assessment involves evaluating the child’s medical history and conducting physical examination protocols. Laboratory testing requirements vary based on age and specific medical conditions.
Q: How are children prepared for anesthesia?
A: Children are prepared through age-appropriate communication and psychological preparation. Techniques like play therapy and visual aids help reduce anxiety. Fasting guidelines are also followed.
Q: What is the role of parental involvement in anesthetic care for children?
A: Parental involvement includes education and informed consent. Parents are present during induction and provide post-operative support. This plays a vital role in managing expectations, reducing anxiety, and monitoring for complications.
Q: What are the different induction techniques used in pediatric anesthesia?
A: Induction techniques include inhalational induction, intravenous induction, rapid sequence induction, and distraction techniques. The choice depends on the child’s condition and the procedure.
Q: How is airway management handled in pediatric anesthesia?
A: Airway management involves selecting appropriate equipment and anticipating difficult airways. Techniques like direct and video laryngoscopy, and supraglottic airway devices are used.
Q: What monitoring is done during pediatric anesthesia?
A: Monitoring includes standard parameters like vital signs and end-tidal CO2. Advanced techniques such as depth of anesthesia and neuromuscular monitoring are also used. Age-specific considerations are taken into account.
Q: How are anesthetic agents dosed for children?
A: Dosing principles include weight-based calculations and body surface area considerations. Understanding pharmacokinetic differences in children is essential for effective dosing.
Q: How is fluid and blood loss managed in children during surgery?
A: Managing fluid and blood loss involves calculating fluid requirements and estimating blood loss. Understanding transfusion thresholds, including age-specific hemoglobin targets, is also important.
Q: Why is temperature regulation important during pediatric procedures?
A: Maintaining normothermia is vital. Preventive strategies against hypothermia and various warming techniques are used. Careful temperature monitoring ensures the child’s temperature remains stable.
Q: What are some common complications in pediatric anesthesia?
A: Complications include respiratory events like laryngospasm, cardiovascular issues such as bradycardia, emergence delirium, and postoperative nausea and vomiting. Each requires specific management strategies.
Q: Are there special considerations for different age groups in pediatric anesthesia?
A: Yes, different age groups present unique challenges. From neonatal physiological instability to the autonomy and assent considerations in school-age children and adolescents, each age group requires tailored care.
Q: How are children with special healthcare needs managed during anesthesia?
A: Children with special needs, such as those with congenital heart disease, respiratory disorders, neuromuscular conditions, or genetic syndromes, require tailored anesthetic care. This is based on their specific conditions.