Bladder Cancer: What is Bladder Cancer?
Bladder cancer starts in the bladder, a hollow organ in the pelvis that stores urine. It’s a significant health concern. Knowing its causes, symptoms, diagnosis, and treatment options is key for effective management. This condition impacts many people. Being informed is the first step in dealing with it. Awareness and education are vital. They help individuals seek medical attention quickly if symptoms appear.
Understanding risks and taking preventive measures can lower the chance of getting this condition. To grasp bladder cancer, it’s key to know the bladder’s role in the urinary system. Bladder cancer, or urothelial carcinoma, starts in the bladder. This organ is vital for urine storage.
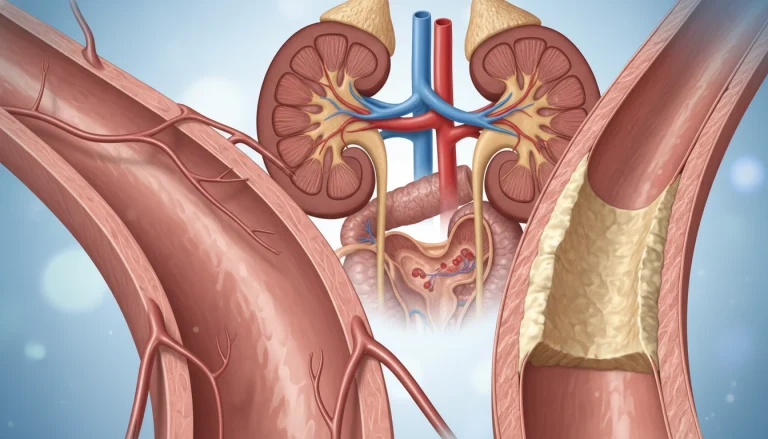
Definition and Bladder Anatomy
The bladder, a muscular sac in the pelvis, is essential for the urinary system. It’s covered in urothelial cells, which can turn cancerous. Knowing the bladder’s structure is critical to understanding cancer development and progression.
The bladder’s wall has layers like the urothelium, lamina propria, and muscularis propria. Cancer can invade these layers, impacting bladder function and potentially spreading to other areas.
The Urinary System Function
The urinary system, including the kidneys, ureters, bladder, and urethra, removes waste and excess fluids. The kidneys filter blood to create urine, which then goes through the ureters to the bladder. This process is vital for understanding bladder cancer’s effects on the urinary system.
The bladder controls urine storage and release through muscles and nerves. As cancer grows, it can disrupt this function. This leads to symptoms and complications.
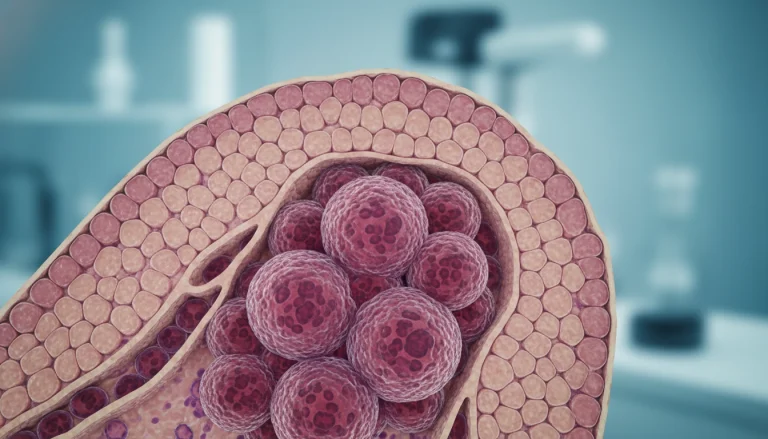
Types of Bladder Cancer
Grasping the various types of bladder cancer is vital for accurate diagnosis and treatment. Bladder cancer is divided into several categories based on the cell type and tumor characteristics.
Urothelial Carcinoma (Transitional Cell Carcinoma)
Urothelial carcinoma, also known as transitional cell carcinoma, is the prevalent form of bladder cancer, making up about 90% of cases. It emerges from the urothelial cells that cover the bladder’s interior. This cancer can be split into low-grade and high-grade tumors, depending on the cancer cell appearance.
Squamous Cell Carcinoma
Squamous cell carcinoma is a less frequent bladder cancer type, constituting around 4% of cases in the United States. It develops from squamous cells, flat cells that may form in the bladder lining due to chronic irritation or infection. Squamous cell carcinoma generally has a worse prognosis than urothelial carcinoma.
Adenocarcinoma and Other Rare Types
Adenocarcinoma is a rare bladder cancer form, originating from glandular cells. Other rare types include:
- Small cell carcinoma
- Sarcoma
- Lymphoma
- Melanoma
These rare types exhibit unique pathological features and may necessitate distinct treatment methods.
Small Cell Carcinoma
Small cell carcinoma of the bladder is a highly aggressive and rare subtype, often linked with a poor prognosis. It closely resembles small cell lung cancer and tends to grow and spread rapidly. This requires immediate and aggressive treatment.
Classifying bladder cancer into these types is critical for selecting the most suitable treatment strategy and predicting outcomes.
Bladder Cancer Statistics and Epidemiology
The impact of bladder cancer is significant, with a complex pattern influenced by various risk factors and geographical differences. It ranks among the top ten most prevalent cancers globally, affecting millions. This condition poses a substantial burden on public health.
Incidence and Prevalence in the United States
In the U.S., bladder cancer is the fourth most common cancer in men and the twelfth in women. Statistics show about 83,000 new cases each year, leading to around 17,000 deaths annually. The majority of cases occur in those over 65, highlighting the disease’s prevalence among the elderly.
Global Distribution Patterns
Bladder cancer incidence varies worldwide, with higher rates in developed countries. Southern and Western Europe, North America, and parts of Africa have the highest rates. These disparities are due to lifestyle, environmental factors, and healthcare access differences.
Grasping these epidemiological trends is critical for crafting effective prevention strategies and bettering bladder cancer outcomes.
Risk Factors for Bladder Cancer
Understanding the risk factors for bladder cancer is key to prevention and early detection. Several factors have been identified that can increase an individual’s likelihood of developing this disease.
Tobacco Use and Smoking
Tobacco use, mainly smoking, is the most significant risk factor for bladder cancer. Chemicals from tobacco smoke are absorbed into the bloodstream, filtered by the kidneys, and end up in the urine. This damages the bladder lining. Smokers are at least three times more likely to develop bladder cancer compared to non-smokers. For more information on bladder cancer, visit Acıbadem International.
- Smoking increases the risk of bladder cancer by exposing the bladder to carcinogens.
- Chemicals from tobacco smoke are absorbed and then excreted in the urine, damaging the bladder.
- Quitting smoking can significantly reduce the risk of developing bladder cancer over time.
Occupational Chemical Exposures
Exposure to certain chemicals in the workplace is another significant risk factor for bladder cancer. Industries that use or produce chemicals like aromatic amines, benzidine, and certain dyes have been linked to an increased risk. Workers in these industries should take protective measures to minimize exposure.
- Workers in the dye, rubber, and leather industries are at higher risk.
- Exposure to chemicals like benzidine and beta-naphthylamine increases bladder cancer risk.
- Using protective equipment and following safety guidelines can reduce exposure risks.
Age, Gender, and Race Considerations
Bladder cancer risk increases with age, with most cases diagnosed in people over 55. Men are more likely to develop bladder cancer than women, and there are also racial differences in incidence rates. Understanding these demographic risk factors can help in targeting preventive measures.
Chronic Bladder Inflammation and Infections
Chronic inflammation or infections of the bladder, such as those caused by long-term catheter use or schistosomiasis, can increase the risk of developing bladder cancer. Managing these conditions is critical for preventing bladder cancer.
- Chronic bladder inflammation can lead to cancerous changes in the bladder lining.
- Treating and managing chronic infections can reduce bladder cancer risk.
Causes and Mechanisms of Bladder Cancer Development
The etiology of bladder cancer is complex, involving environmental exposures and genetic alterations. Understanding these factors is key to developing effective prevention and treatment strategies.
Carcinogenic Substances and Pathways
Carcinogenic substances are a major factor in bladder cancer development. These substances are found in tobacco smoke, certain industrial chemicals, and environmental pollutants. Once absorbed, they are excreted in urine, potentially damaging the bladder lining.
- Tobacco smoke contains numerous carcinogens that are known to increase the risk of bladder cancer.
- Industrial chemicals, such as aromatic amines, have been linked to bladder cancer in workers exposed to these substances.
- Certain dietary factors and contaminants in drinking water may also contribute to bladder cancer risk.
Genetic Mutations and Molecular Changes
Genetic mutations are a critical component in the development of bladder cancer. These mutations can occur due to environmental exposures or errors in DNA replication.
Common Genetic Alterations
Several genes are frequently mutated in bladder cancer, including TP53, PIK3CA, and FGFR3. These mutations can lead to uncontrolled cell growth and tumor formation.
Hereditary Factors
While most bladder cancers are sporadic, hereditary factors can also play a role. Certain genetic syndromes, such as Lynch syndrome, have been associated with an increased risk of bladder cancer.
Signs and Symptoms of Bladder Cancer
Identifying the early signs of bladder cancer is key to timely diagnosis and effective treatment. Bladder cancer often shows specific symptoms that can greatly affect a person’s quality of life.
Early Warning Signs
Early detection of bladder cancer can significantly improve treatment outcomes. Two primary early warning signs are hematuria and urinary changes.
Hematuria (Blood in Urine)
Hematuria, or blood in the urine, is the most common symptom of bladder cancer. It can make urine appear pink, red, or dark brown. It’s vital to seek medical evaluation to find the cause, as hematuria can stem from other conditions too.
Urinary Changes and Discomfort
Urinary changes, such as increased frequency, urgency, or discomfort while urinating, can also signal bladder cancer. These symptoms should not be dismissed, as they can worsen over time.
Advanced Symptoms and Complications
As bladder cancer advances, more severe symptoms can emerge. These include pain in the pelvic area, lower back, or sides. Advanced bladder cancer can also cause urinary tract obstruction, kidney damage, or metastasis to other parts of the body.
In conclusion, being aware of bladder cancer symptoms is essential for early detection and treatment. If you notice unusual urinary changes or discomfort, it’s critical to consult a healthcare professional for proper evaluation and care.
Diagnostic Approaches and Testing
Diagnosing bladder cancer involves several steps, from initial checks to detailed imaging. Accurate diagnosis is key to understanding the cancer’s stage and grade. This information is essential for choosing the right treatment.
Initial Evaluation and Urinalysis
The first step in diagnosing bladder cancer includes a detailed medical history and physical exam. Urinalysis is a critical part of this, as it looks for blood or other unusual substances in the urine. These signs can lead to further testing.
Cystoscopy and Biopsy Procedures
Cystoscopy lets doctors see inside the bladder with a cystoscope. It helps spot tumors or other issues. If something looks off, a biopsy might be done to check for cancer cells.
Imaging Studies and Biomarkers
Imaging studies are vital for diagnosing and staging bladder cancer. They help figure out how far the disease has spread. This is important for planning treatment.
CT Urography and MRI
CT urography is a CT scan that focuses on the urinary system. It’s great for finding bladder tumors and checking the upper urinary tract. MRI can also help by examining the bladder and nearby tissues.
Emerging Diagnostic Technologies
New technologies are being developed to better detect and monitor bladder cancer. These include biomarkers and advanced imaging. They aim to improve diagnosis and help guide treatment choices.
Staging and Grading of Bladder Cancer
Accurate staging and grading are critical for clinicians to create a treatment plan that meets the patient’s needs. Staging determines the cancer’s spread, while grading examines the cancer cells under a microscope.
TNM Classification System
The TNM classification system is widely used for staging bladder cancer. It considers three main components: the tumor’s size and extent (T), nearby lymph node involvement (N), and distant metastasis (M).
T (Tumor) Staging
T staging evaluates the primary tumor’s extent, ranging from Ta (non-invasive papillary carcinoma) to T4 (tumor invading beyond the bladder).
N (Node) and M (Metastasis) Staging
N staging assesses lymph node involvement, while M staging checks for distant metastasis. Both are critical for determining the cancer’s spread.
Clinical vs. Pathological Staging
Clinical staging is based on diagnostic tests before treatment. Pathological staging is determined after surgical removal of the tumor, providing more accurate information.
Histological Grading and Its Significance
Histological grading assesses the aggressiveness of cancer cells. A higher grade indicates more abnormal cells, correlating with a worse prognosis.
Understanding the grade helps in deciding the intensity of treatment and predicting the likelihood of recurrence.
Treatment Options for Non-Muscle Invasive Bladder Cancer
Effective treatment for non-muscle invasive bladder cancer involves a combination of surgical and adjuvant therapies. The main aim is to remove the tumor, prevent its return, and stop it from becoming muscle-invasive.
Transurethral Resection of Bladder Tumor (TURBT)
TURBT is a key procedure for diagnosing and treating non-muscle invasive bladder cancer. It removes the tumor and a part of the bladder wall to check how deep it is. This is done under general or spinal anesthesia.
The TURBT procedure accurately stages and grades the tumor. This information helps decide on further treatment. It’s often followed by intravesical therapy to lower recurrence risk.

Intravesical Therapy Approaches
Intravesical therapy involves putting therapeutic agents directly into the bladder. It’s used to treat non-muscle invasive bladder cancer by targeting remaining cancer cells after TURBT.
BCG Immunotherapy
BCG (Bacillus Calmette-Guérin) immunotherapy is a common intravesical treatment for high-risk non-muscle invasive bladder cancer. It boosts the immune system to fight cancer cells, reducing recurrence and progression risk.
Chemotherapy Agents
Intravesical chemotherapy uses agents like mitomycin C to kill bladder cancer cells. It’s often given right after TURBT to clear any remaining cancer cells.
Surveillance and Follow-up Protocols
Regular surveillance is key for patients with non-muscle invasive bladder cancer. It involves cystoscopy, urine cytology, and imaging studies at set times.
Surveillance helps catch recurrence early, allowing for timely treatment and better outcomes. The schedule and duration of follow-up depend on the patient’s risk level.
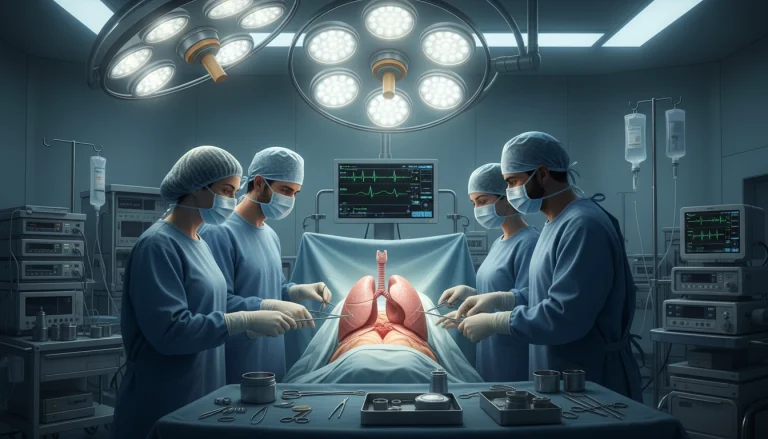
Treatment Strategies for Muscle Invasive Bladder Cancer
Managing muscle-invasive bladder cancer requires a multi-faceted approach. This includes surgery and therapy. Given its aggressive nature, prompt and effective treatment is essential to enhance patient outcomes.
Radical Cystectomy and Lymph Node Dissection
Radical cystectomy, the removal of the bladder, is a primary treatment. It often involves removing surrounding lymph nodes to prevent cancer spread. For more information on bladder cancer treatment options, visit https://acibademinternational.com/bladder-cancer/.
Urinary Diversion Techniques
After radical cystectomy, urinary diversion techniques are necessary. These methods redirect urine flow.
Ileal Conduit
An ileal conduit uses a portion of the intestine for urine flow. It’s commonly used due to its simplicity.
Neobladder Reconstruction
Neobladder reconstruction creates a new bladder from intestine. It aims to maintain normal urinary function.
Neoadjuvant and Adjuvant Therapies
Neoadjuvant therapies, like chemotherapy, are given before surgery. They aim to shrink tumors. Adjuvant therapies are used post-surgery to eliminate remaining cancer cells, reducing recurrence risk.
Radiation Therapy in Bladder Cancer Management
Radiation therapy is a key treatment for bladder cancer, providing a viable option for patients. It aims to kill cancer cells or slow their growth. It can be used alone or with other treatments.
External Beam Radiation Techniques
External beam radiation therapy (EBRT) is a common method for treating bladder cancer. It uses high-energy beams from outside the body to target and destroy cancer cells. EBRT is given over several weeks, with sessions five days a week.
Bladder Preservation Approaches
Bladder preservation strategies aim to keep the patient’s quality of life high by avoiding radical cystectomy. One such approach is trimodal therapy.
Trimodal Therapy
Trimodal therapy combines transurethral resection of bladder tumor (TURBT), chemotherapy, and radiation therapy. This approach has shown promising results in preserving bladder function while treating cancer effectively.
Patient Selection Criteria
Choosing the right patients for bladder preservation is critical. Factors like tumor size, stage, and patient health are considered when deciding on trimodal therapy.
- Tumor characteristics
- Patient’s overall health
- Previous treatments
Radiation therapy is a valuable option for bladder cancer patients, whether used alone or with other therapies. Understanding different radiation techniques and bladder preservation approaches helps healthcare providers tailor treatment plans to individual needs.
Advanced Systemic Treatments for Bladder Cancer
The field of bladder cancer treatment is rapidly advancing with new systemic treatments. These innovations hold great promise for better patient outcomes and improved quality of life.
Conventional Chemotherapy Regimens
Chemotherapy remains a key treatment for bladder cancer, mainly for advanced stages. Gemcitabine and cisplatin are common choices. They are often given before or after surgery to lower cancer recurrence risk.
Immunotherapy Breakthroughs
Immunotherapy is a game-changer in bladder cancer treatment. It leverages the body’s immune system for a targeted approach to the disease.
Checkpoint Inhibitors
Checkpoint inhibitors like pembrolizumab and atezolizumab are effective against advanced bladder cancer. They work by boosting the immune system. These drugs are approved for treating locally advanced or metastatic bladder cancer.
Response Predictors
Research focuses on predicting how well patients will respond to immunotherapy. Biomarkers, such as PD-L1 expression, are being studied to find the best candidates for these treatments.
Targeted Therapies and Precision Medicine
Targeted therapies and precision medicine are becoming more common in bladder cancer treatment. These methods aim to customize treatment based on the patient’s tumor, potentially leading to better results.

Prognosis and Survival Rates
The prognosis for bladder cancer patients varies significantly based on the stage and grade of the disease at diagnosis. Understanding the prognosis and survival rates is essential for patients to make informed decisions about their treatment.
Survival Statistics by Stage and Grade
Survival rates for bladder cancer are closely linked to the stage and grade of the tumor. Here are some key statistics:
- For patients with non-muscle invasive bladder cancer, the 5-year survival rate is approximately 90%.
- For those with muscle-invasive bladder cancer, the 5-year survival rate drops to around 50-60%.
- Patients with metastatic bladder cancer have a 5-year survival rate of about 15%.
Factors Affecting Prognosis
Several factors influence the prognosis of bladder cancer patients. These include clinical factors and molecular/genetic markers.
Clinical Factors
Clinical factors that affect prognosis include:
- Tumor stage and grade
- Presence of lymph node involvement
- Patient’s overall health and age
Molecular and Genetic Markers
Molecular and genetic markers are increasingly being used to predict prognosis. Some of the key markers include:
- Genetic mutations such as TP53 and RB1
- Expression of certain proteins like PD-L1
Understanding these factors helps healthcare providers tailor treatment plans to individual patients, potentially improving their prognosis.
Living with Bladder Cancer
Managing bladder cancer requires a holistic approach. It involves medical treatment, lifestyle adjustments, and emotional support. This ensures a better quality of life for those affected.
Quality of Life Considerations
Quality of life is essential for bladder cancer patients. Treatment options and their side effects can greatly impact daily life. They affect a patient’s ability to perform routine tasks and maintain social relationships.
It’s vital to manage symptoms and side effects. This can be achieved through medication, lifestyle changes, and supportive care. These measures help reduce the disease’s impact and its treatment’s side effects.
Psychological Impact and Mental Health
The psychological effects of bladder cancer can be significant. Anxiety, depression, and fear of recurrence are common. These emotions can weigh heavily on patients.
Access to mental health resources is critical. Counseling and support groups are essential. Healthcare providers must offer care that includes psychological support.
Support Resources and Patient Advocacy
Support resources are key for bladder cancer patients. They include patient advocacy groups, online forums, and local support networks. These resources help patients navigate their challenges.
- Patient advocacy groups provide valuable information and support.
- Online forums offer a platform for patients to share their experiences.
- Local support networks provide emotional support and practical assistance.
By utilizing these resources, patients can manage their condition better. This improves their quality of life significantly.
Advances in Bladder Cancer Research and Future Directions
Recent years have brought significant progress in bladder cancer research. This has greatly improved our understanding of the disease and its treatment. New trends and therapies are being explored to better patient outcomes.
Targeted therapies are a key area of research, aiming to target specific weaknesses in bladder cancer cells. Immunotherapy has also shown promise, with checkpoint inhibitors proving effective for some patients.
The future of bladder cancer research will likely involve more precision medicine. This will use advances in genomics and biomarker discovery. The aim is to tailor treatments to each patient’s unique tumor characteristics.
As research advances, we can look forward to better diagnostic tools and treatments. Patient care will also improve. The outlook for bladder cancer management is promising, with new breakthroughs on the horizon.
FAQ
Q: What are the common symptoms of bladder cancer?
A: Symptoms include blood in urine, frequent need to urinate, painful urination, and abdominal pain.
Q: What are the risk factors for developing bladder cancer?
A: Risk factors include tobacco use, exposure to chemicals, age, gender, and chronic bladder issues.
Q: How is bladder cancer diagnosed?
A: Diagnosis involves urinalysis, cystoscopy, biopsy, and imaging like CT urography and MRI.
Q: What are the different types of bladder cancer?
A: Main types are urothelial carcinoma, squamous cell carcinoma, adenocarcinoma, and rare small cell carcinoma.
Q: How is bladder cancer staged and graded?
A: Staging uses the TNM system, and grading is based on tumor histology.
Q: What are the treatment options for non-muscle invasive bladder cancer?
A: Treatment includes TURBT, intravesical therapy (BCG or chemotherapy), and surveillance.
Q: What are the treatment strategies for muscle-invasive bladder cancer?
A: Treatment involves radical cystectomy, urinary diversion, and neoadjuvant or adjuvant therapies.
Q: Can bladder cancer be prevented?
A: While prevention is not guaranteed, reducing risk factors like tobacco use and chemical exposure can help.
Q: What is the prognosis for bladder cancer patients?
A: Prognosis depends on stage, grade, and other factors, affecting survival rates.
Q: Are there any new treatments or research directions for bladder cancer?
A: Yes, research includes immunotherapy, targeted therapies, and precision medicine.