Cancer Care with Radiotherapy: Radiotherapy (Radiation Treatment)
Radiotherapy, also known as Radiation Treatment, is a highly effective cancer treatment option. It has been widely used to improve patient outcomes. This treatment involves the use of high-energy particles or waves to destroy or damage cancer cells. It halts their growth and spread. As a key component of cancer care, Radiotherapy is often used alone or in combination with other treatments. These include surgery and chemotherapy. By targeting cancer cells precisely, Radiation Treatment helps to minimize damage to surrounding healthy tissues. This reduces the risk of side effects and improves the quality of life for patients.
Understanding Radiotherapy (Radiation Treatment)
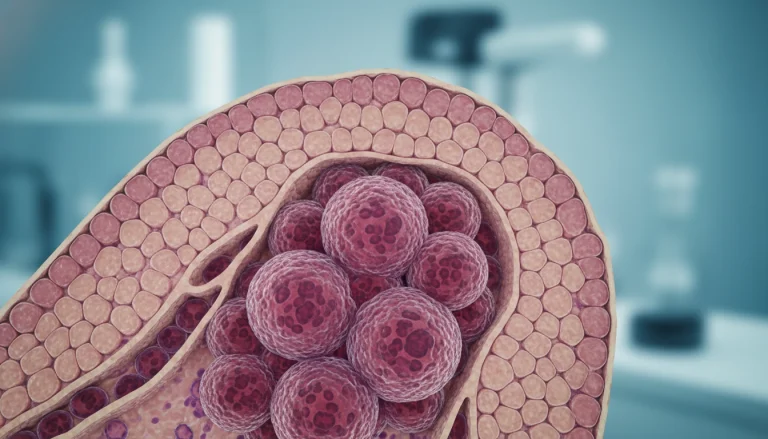
Radiotherapy has become a vital part of cancer treatment, bringing new hope to patients globally. It uses high-energy radiation to target and kill cancer cells or slow their growth. This treatment damages the DNA of cancer cells, preventing them from dividing and spreading.
The Science Behind Radiation Therapy
Radiation therapy delivers precise doses of radiation to areas with cancer cells. This radiation damages the DNA, causing cell death or stopping cell division. There are two main types: external beam radiation therapy, where radiation comes from outside, and internal radiation therapy (brachytherapy), where the source is placed near the tumor.
Goals and Applications of Radiotherapy
The main aim of radiotherapy is to destroy cancer cells with minimal harm to healthy tissues. It can be used alone or with surgery and chemotherapy. It’s used in various treatments, including curative, palliative, and adjuvant therapy.
Curative radiotherapy aims to remove cancer completely. Palliative radiotherapy aims to ease symptoms and improve life quality for those with advanced cancer. Radiotherapy is applied in many cancer types, such as breast, prostate, lung, and brain cancers. Its effectiveness makes it a key part of cancer treatment plans, giving patients a chance at cure or symptom relief.
History and Evolution of Radiation Therapy
The journey of radiation therapy’s development is long and marked by significant milestones. It has evolved over the years, leading to better treatment outcomes and patient care. This evolution is a testament to the continuous advancements in cancer treatment.
Early Discoveries and Applications
After Wilhelm Conrad Röntgen’s discovery of X-rays in 1895, radiation therapy’s medical use began. Initially, its applications were experimental, with mixed results. As knowledge about radiation and its biological effects grew, so did the techniques and equipment in radiation therapy.
By the early 20th century, radiation therapy became a common treatment for some cancers. The introduction of cobalt therapy in the 1950s was a major leap forward. It allowed for more precise radiation delivery to tumors, reducing harm to healthy tissues.
Modern Advancements in Radiotherapy Technology
Modern radiation therapy has seen major technological strides, including the advent of linear accelerators. These replaced cobalt machines in many facilities. The integration of computer technology has enabled advanced treatment planning and delivery methods, such as IMRT and IGRT.
These innovations have enhanced radiation therapy’s precision and effectiveness. They have led to better tumor control and fewer side effects. Ongoing research and development continue to expand the capabilities of radiation oncology.
Types of Radiotherapy
Grasping the various forms of radiotherapy is essential for managing cancer effectively. Radiotherapy, or radiation therapy, employs high-energy particles or waves to destroy cancer cells. The selection of radiotherapy type hinges on several factors. These include the cancer’s type and stage, the patient’s health, and the treatment’s objectives.
External Beam Radiation Therapy
External Beam Radiation Therapy (EBRT) is a prevalent method where radiation originates from outside the body. It targets cancer sites using a machine that emits high-energy beams.
Conventional External Beam Radiation
Conventional EBRT, the most common radiation therapy, employs X-rays or gamma rays to target tumors. It is administered in fractions over several weeks.
Proton Therapy
Proton therapy, a form of EBRT, utilizes protons instead of X-rays. It’s beneficial for treating tumors near critical structures, as it delivers a high dose to the tumor while protecting surrounding healthy tissues.
Electron Beam Therapy
Electron beam therapy, another EBRT variant, treats superficial tumors using electrons. It’s effective for skin cancers or tumors near the surface.
Internal Radiation Therapy (Brachytherapy)
Brachytherapy places a radioactive source directly inside or near the tumor. This method delivers high doses of radiation to the cancer site while minimizing harm to healthy tissues.
High-Dose Rate Brachytherapy
High-dose rate brachytherapy administers radiation at a high dose rate for a short duration. It’s often used for treating certain gynecological and prostate cancers.
Low-Dose Rate Brachytherapy
Low-dose rate brachytherapy delivers radiation at a low dose rate continuously over an extended period. It’s commonly applied for prostate cancer treatment.
Systemic Radiation Therapy
Systemic radiation therapy employs radioactive substances given orally or intravenously. These substances target cancer cells throughout the body selectively.
It’s used for treating certain thyroid cancers and other cancers that have spread throughout the body.
The Radiotherapy Treatment Process
The journey through radiotherapy starts with an initial consultation, a critical step. This process involves several stages, from preparation to treatment sessions. It ensures radiation is precisely targeted.
Initial Consultation and Assessment
The initial consultation is key. Here, the radiation oncologist assesses the patient’s condition and reviews their medical history. They discuss treatment options, explaining the diagnosis, treatment plan, and possible side effects. Imaging tests like CT scans, MRI, or PET scans are reviewed to determine the cancer’s extent and the best radiotherapy approach.
Simulation and Treatment Planning
After the initial consultation, simulation and treatment planning follow. This stage is essential for mapping the treatment area and determining the optimal radiation dosage.
CT Simulation
CT simulation uses a CT scanner to locate the tumor and surrounding anatomy. The patient is positioned on a CT table, with immobilization devices ensuring consistent positioning. Markers or tattoos are placed on the skin to guide radiation therapists during treatment.
Treatment Plan Development
A team of radiation oncologists, physicists, and dosimetrists then develop a personalized treatment plan. This plan outlines the total radiation dose, number of fractions, and technique. Advanced software is used to optimize the plan, ensuring the tumor receives the maximum dose while protecting healthy tissues.
Treatment Sessions and Duration
Radiotherapy treatment sessions are conducted on an outpatient basis, Monday through Friday, over several weeks. Each session lasts between 15 to 30 minutes, with the actual radiation delivery taking only a few minutes. During sessions, the patient is positioned correctly using markers or tattoos from the simulation. The treatment is painless, allowing patients to breathe normally and relax.
The number of treatment sessions depends on the cancer type and stage, as well as treatment goals. Patients are monitored regularly to assess their response and manage side effects.
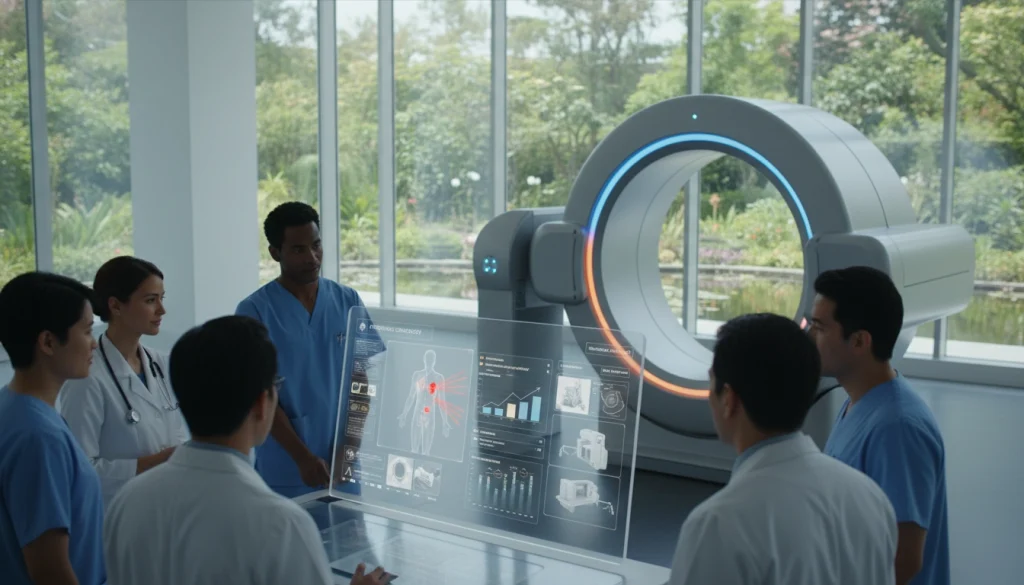
Advanced Radiotherapy Techniques
Advanced radiotherapy techniques have transformed cancer treatment, providing precise and effective methods to target tumors. These modern approaches have significantly improved patient outcomes. They do this by minimizing damage to surrounding healthy tissues.
3D Conformal Radiation Therapy
3D Conformal Radiation Therapy (3D-CRT) uses advanced imaging technologies to deliver radiation beams that conform to the tumor’s shape. This precision reduces the exposure of surrounding tissues to radiation. It minimizes the risk of side effects.
Intensity-Modulated Radiation Therapy (IMRT)
Intensity-Modulated Radiation Therapy (IMRT) is an advanced version of 3D-CRT. It modulates the intensity of the radiation beams. This precision allows for higher doses to be delivered to the tumor while sparing critical structures.
Image-Guided Radiation Therapy (IGRT)
Image-Guided Radiation Therapy (IGRT) uses imaging technologies during treatment to ensure accurate radiation delivery. IGRT allows for real-time adjustments. This improves treatment precision and reduces complications.
Stereotactic Radiosurgery (SRS)
Stereotactic Radiosurgery (SRS) is a highly precise radiation therapy used for brain tumors and abnormalities. It delivers a high dose of radiation in a single fraction. This minimizes damage to surrounding brain tissue.
Stereotactic Body Radiation Therapy (SBRT)
Stereotactic Body Radiation Therapy (SBRT) is similar to SRS but treats tumors outside the brain. SBRT delivers high doses of radiation over a few fractions. It offers a potent treatment for various cancers. For more information on SBRT, visit SBRT treatment options.
The key benefits of these advanced radiotherapy techniques include:
- Enhanced precision in targeting tumors
- Reduced risk of damage to surrounding healthy tissues
- Improved patient outcomes due to more effective treatment
- Potential for shorter treatment durations
These techniques represent significant advancements in radiotherapy. They offer new hope for patients with various types of cancer.
Common Side Effects of Radiotherapy
Understanding the common side effects of radiotherapy is essential for patients undergoing this treatment. Radiotherapy, while effective in treating cancer, can cause a range of side effects. These occur due to its impact on both cancerous and healthy cells.
Short-term Side Effects
Short-term side effects occur during or shortly after radiotherapy treatment. These effects are usually temporary but can be uncomfortable.
Skin Changes
Radiotherapy can cause skin changes, including redness, itching, and dryness, similar to sunburn. Proper skin care can help mitigate these effects.
Fatigue
Fatigue is a common side effect, where patients feel extremely tired. This can be managed by getting plenty of rest and maintaining a balanced diet.
Site-Specific Effects
Depending on the area being treated, radiotherapy can cause site-specific side effects. For example, radiation to the head and neck area can cause mouth sores and difficulty swallowing.
Long-term Side Effects
Long-term side effects can occur months or even years after radiotherapy has ended. These can include fibrosis, secondary cancers, and organ damage, depending on the dose and area treated.

Managing and Minimizing Side Effects
Managing side effects is critical for improving the quality of life for patients undergoing radiotherapy. This can involve a combination of medical treatments, lifestyle changes, and supportive care.
For instance, using specific creams can help with skin reactions, while dietary adjustments can help manage gastrointestinal side effects. Regular follow-up with healthcare providers is also essential for monitoring and addressing any long-term effects.
Radiotherapy for Different Cancer Types
Radiotherapy is a vital treatment for various cancers, including breast, prostate, lung, and brain tumors. It’s tailored to each cancer type, considering the tumor’s location, size, and stage. This personalized approach ensures patients get the most effective treatment for their condition.
Breast Cancer Radiation
Radiotherapy is a common treatment for breast cancer, often after surgery. It aims to eliminate remaining cancer cells, reducing recurrence risk. The treatment targets the breast with precision, minimizing damage to healthy tissue.
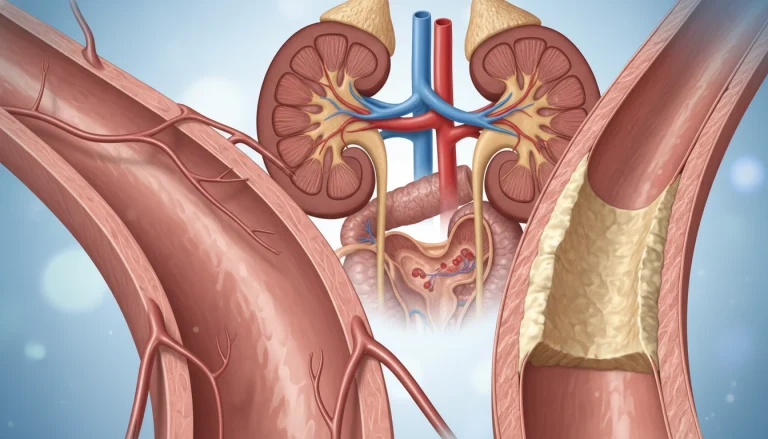
Prostate Cancer Radiation
Radiotherapy for prostate cancer can be external or internal through brachytherapy. Small radioactive seeds are implanted in the prostate gland. External beam radiation therapy (EBRT) is also used, sometimes with hormone therapy. The choice depends on the cancer’s stage and the patient’s health.
Lung Cancer Radiation
Lung cancer treatment often includes radiotherapy, suitable for those not fit for surgery or with advanced disease. Stereotactic body radiation therapy (SBRT) delivers precise, high doses to the tumor. This method controls tumor growth and relieves symptoms.
Brain Tumor Radiation
Radiotherapy is a key treatment for brain tumors, both benign and malignant. Stereotactic radiosurgery (SRS) delivers a high dose in one session, sparing brain tissue. Fractionated radiotherapy divides the dose into smaller fractions, given over several sessions, reducing side effects.
Head and Neck Cancer Radiation
Head and neck cancers are often treated with radiotherapy, sometimes with chemotherapy or surgery. Intensity-modulated radiation therapy (IMRT) is commonly used. It targets tumors with complex shapes precisely, reducing dose to nearby structures. This minimizes side effects like dry mouth and swallowing difficulties.
Here are some key benefits of radiotherapy for different cancer types:
- Tailored treatment plans based on the specific cancer type and stage
- Effective in controlling tumor growth and alleviating symptoms
- Can be used alone or in combination with other treatments like surgery and chemotherapy
- Advanced techniques like IMRT, SBRT, and SRS offer precise targeting and reduced side effects
Preparing for Radiotherapy Treatment
Understanding the steps involved in preparing for radiotherapy can greatly reduce anxiety. Radiotherapy is a common cancer treatment. Being well-prepared can significantly improve your experience.
Physical Preparation
Physical preparation is key before starting radiotherapy. You may undergo tests to assess your health and cancer extent. Your healthcare team will guide you on maintaining a healthy diet and staying hydrated.
They may also advise on avoiding certain medications or supplements that could affect radiotherapy. Following your radiation oncologist’s specific instructions is vital. This includes skin care in the treatment area to minimize side effects.
Mental and Emotional Preparation
Mental and emotional preparation is just as important as physical preparation. Radiotherapy can be tough, both physically and emotionally. Seeking support from family, friends, or support groups is encouraged.
Stress-reducing activities like meditation or yoga can be beneficial. Your healthcare team can offer resources and recommendations for managing emotional aspects of radiotherapy.
Practical Considerations
Practical considerations are also vital in preparing for radiotherapy. This includes planning for daily transportation to treatment sessions, which can last several weeks.
Transportation Planning
Reliable transportation is essential, as you may not be able to drive after treatment. Consider asking a friend or family member for help. Look into local transportation services as well.
Work and Family Arrangements
You may need to adjust work or family responsibilities during treatment. Discussing your schedule with your employer and family is important. This ensures a smooth experience for everyone involved.
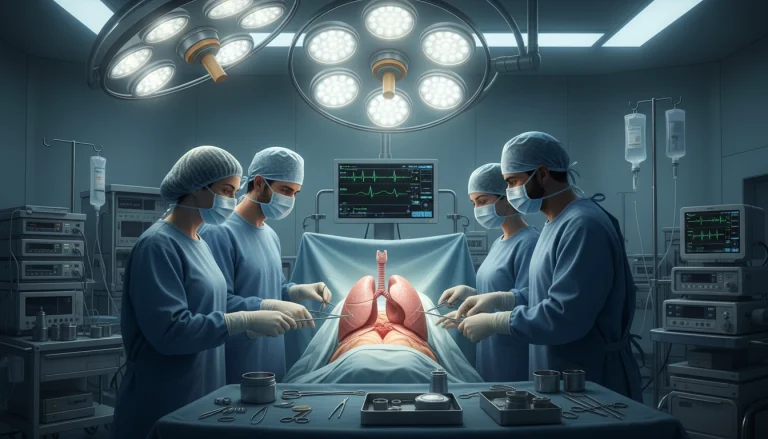
Combining Radiotherapy with Other Treatments
Integrating radiotherapy with other treatments is now a key part of cancer care. This approach allows for personalized treatment plans tailored to each patient’s needs. It’s a step towards more effective cancer management.
Neoadjuvant and Adjuvant Radiotherapy
Neoadjuvant radiotherapy is given before the main treatment, like surgery. It aims to shrink tumors, making them easier to remove. Adjuvant radiotherapy follows the primary treatment to kill any cancer cells left behind.
Chemoradiation Therapy
Chemoradiation therapy combines radiotherapy with chemotherapy. It’s used to treat many cancers, like head and neck, lung, and cervical cancer. This method boosts treatment effectiveness.
Radiotherapy with Immunotherapy
Radiotherapy can be paired with immunotherapy to boost the immune system’s cancer-fighting abilities. This combination shows great promise in treating various cancers.
Radiotherapy with Targeted Therapies
Targeted therapies aim at specific cancer cells. When paired with radiotherapy, they can lead to better treatment outcomes. This method is being tested in clinical trials.
By combining radiotherapy with other treatments, healthcare providers can craft effective plans. These plans aim to improve patient outcomes and quality of life.
Cost and Insurance Considerations for Radiotherapy
Understanding the financial aspects of radiotherapy is key for patients to make informed decisions about their treatment.
Average Costs of Different Radiotherapy Types
The costs of radiotherapy vary significantly based on the type of therapy. Here are some general estimates:
- External Beam Radiation Therapy (EBRT): The cost can range from $10,000 to $50,000 or more, depending on the complexity and number of sessions.
- Internal Radiation Therapy (Brachytherapy): Costs can range from $5,000 to $20,000.
- Stereotactic Body Radiation Therapy (SBRT): This advanced technique can cost between $15,000 to $60,000.
Insurance Coverage in the United States
Most health insurance plans in the United States cover radiotherapy, but the extent of coverage can vary. For instance:
- Medicare: Covers radiotherapy for cancer treatment, including EBRT and brachytherapy.
- Private Insurance: Many private insurers cover radiotherapy, but patients should check their specific plans.
Financial Assistance Programs
Several financial assistance programs are available to help patients cover the costs of radiotherapy, including:
- The Patient Access Network Foundation (PANF)
- The Cancer Financial Assistance Coalition (CFAC)
Life During and After Radiotherapy
Radiotherapy can be a challenging experience, but understanding what to expect during and after treatment can make a significant difference. As patients navigate their treatment journey, they often face various physical and emotional changes.
Daily Life During Treatment
During radiotherapy, patients may experience fatigue, skin reactions, and other side effects that can impact their daily activities. It’s essential to find ways to manage these challenges effectively.
Managing Work and Activities
Patients may need to adjust their work schedule or daily routines to accommodate treatment. Here are some tips:
- Communicate with your employer about your treatment schedule
- Prioritize tasks and conserve energy
- Take regular breaks to rest
Nutrition and Self-Care
Maintaining a healthy diet and practicing self-care can help patients cope with treatment side effects. Consider the following:
- Eating a balanced diet rich in fruits, vegetables, and whole grains
- Staying hydrated by drinking plenty of water
- Engaging in relaxation techniques, such as meditation or deep breathing
Recovery Timeline
The recovery timeline after radiotherapy varies depending on the individual and the type of cancer being treated. Generally, patients can expect to start feeling better within a few weeks to a few months after completing treatment.
Follow-up Care and Monitoring
Follow-up care is critical after radiotherapy to monitor for any signs of cancer recurrence and to manage any long-term side effects. Patients should work closely with their healthcare team to develop a follow-up care plan.
Latest Research and Future Directions in Radiotherapy
The latest research in radiotherapy is revolutionizing how radiation therapy is administered. It’s becoming more precise and tailored to each patient. Studies are ongoing to introduce new technologies and methods. These aim to improve treatment results and lessen side effects.
Emerging Technologies and Approaches
Several emerging technologies are reshaping radiotherapy. These include advanced imaging, sophisticated treatment planning systems, and innovative radiation delivery methods.
FLASH Radiotherapy
FLASH radiotherapy is a groundbreaking method. It delivers radiation at extremely high rates. This could reduce damage to healthy tissues while keeping tumors under control. Though in its early stages, it shows great promise.
Artificial Intelligence in Treatment Planning
Artificial intelligence (AI) is being used in radiotherapy planning. It aims to optimize dose distribution and enhance treatment outcomes. AI algorithms can process complex data, guiding clinicians in their decisions.
Personalized Radiation Treatment
Personalized radiation treatment is tailored to each patient’s unique tumor and anatomy. This approach seeks to maximize radiotherapy’s effectiveness while minimizing side effects.
Reducing Treatment Time and Sessions
Research is underway to shorten radiotherapy sessions. Techniques like hypofractionation and stereotactic body radiation therapy (SBRT) are being explored. These aim to improve patient convenience and possibly enhance treatment outcomes.
Navigating Your Radiotherapy Journey
Starting a radiotherapy journey can be daunting, but with the right support, it becomes more manageable. A dedicated care team is essential, providing medical guidance, emotional support, and navigating the treatment path.
A multidisciplinary team, including radiation oncologists, nurses, and other specialists, is key. They collaborate to create a tailored treatment plan, manage side effects, and address patient concerns. This ensures a cohesive approach to care.
Patients also benefit from organizations focused on cancer care and radiotherapy. These groups offer counseling, support groups, and educational materials. They help patients deal with the emotional and practical aspects of radiotherapy.
Radiotherapy success hinges on medical expertise, personal strength, and support from healthcare and loved ones. Understanding the treatment and using available resources can enhance the patient’s experience. This approach improves their quality of life during treatment.
For more information and support, numerous reputable organizations are available. By tapping into these resources and maintaining a strong support network, patients can confidently navigate their radiotherapy journey.
FAQ About Cancer Care with Radiotherapy
Q: What is radiotherapy?
A: Radiotherapy, also known as radiation therapy, is a cancer treatment. It uses high-energy particles or waves to destroy or damage cancer cells.
Q: How does radiotherapy work?
A: Radiotherapy delivers high-energy radiation to the tumor site. This kills cancer cells or slows their growth. The goal is to destroy cancer cells while minimizing damage to healthy tissues.
Q: What are the different types of radiotherapy?
A: There are several types of radiotherapy, including external beam radiation therapy, brachytherapy, and systemic radiation therapy. Each type has its specific applications and benefits.
Q: What is external beam radiation therapy?
A: External beam radiation therapy is a type of radiotherapy. A machine outside the body directs radiation beams to the tumor site. It is a common treatment for various types of cancer.
Q: What is brachytherapy?
A: Brachytherapy is a type of radiotherapy. A small amount of radioactive material is placed inside or near the tumor. It allows for a high dose of radiation to be delivered directly to the cancer cells.
Q: How is radiotherapy treatment planned?
A: Radiotherapy treatment planning involves a team of healthcare professionals. They include radiation oncologists, medical physicists, and radiation therapists. Together, they create a personalized treatment plan tailored to the patient’s specific needs.
Q: What are the common side effects of radiotherapy?
A: Common side effects of radiotherapy include fatigue, skin changes, and site-specific effects. These can include hair loss or mouth sores. The severity and duration of these side effects vary depending on the treatment area and dose.
Q: How can side effects be managed?
A: Side effects can be managed through a combination of medications, lifestyle changes, and self-care techniques. Patients should discuss their side effects with their healthcare team to determine the best course of action.
Q: Can radiotherapy be combined with other cancer treatments?
A: Yes, radiotherapy can be combined with other cancer treatments. These include chemotherapy, immunotherapy, and targeted therapies. The combination of treatments can enhance their effectiveness and improve patient outcomes.
Q: What is the cost of radiotherapy?
A: The cost of radiotherapy varies depending on the type and duration of treatment, as well as the location and healthcare provider. Patients should discuss their insurance coverage and financial options with their healthcare team.
Q: How can I prepare for radiotherapy?
A: Preparing for radiotherapy involves physical, emotional, and practical preparations. Patients should follow their healthcare team’s guidance on preparing for treatment. This includes managing their diet, transportation, and work arrangements.