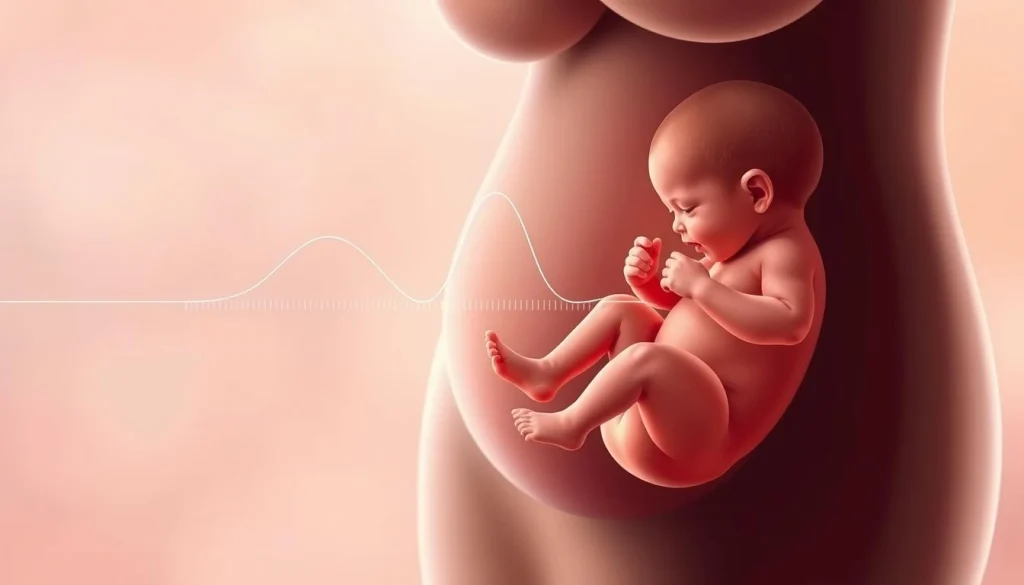
Gestational Diabetes: What is Gestational Diabetes?
Gestational diabetes emerges during pregnancy, often in the second or third trimester. It’s marked by elevated blood sugar levels. If not managed, it can endanger both mother and baby. Effective management of gestational diabetes is essential for a healthy pregnancy. This entails monitoring blood sugar, adhering to a balanced diet, and staying active. By doing so, women can mitigate risks and promote optimal health for themselves and their offspring. Gestational diabetes is a form of diabetes that appears during pregnancy and needs careful management. It’s a condition marked by high blood sugar levels first noticed during pregnancy.
Definition and Prevalence
Gestational diabetes occurs when the body becomes resistant to insulin, a hormone that controls blood sugar, during pregnancy. This resistance can cause blood glucose levels to rise. The Centers for Disease Control and Prevention (CDC) reports that gestational diabetes affects about 9.2% of pregnancies in the United States.
The risk of gestational diabetes varies among different groups. It’s influenced by factors like age, ethnicity, and pre-pregnancy weight. Knowing these factors helps identify women at higher risk.
How It Differs from Type 1 and Type 2 Diabetes
Gestational diabetes is distinct from Type 1 and Type 2 diabetes in its onset and causes. Unlike Type 1 diabetes, which is an autoimmune condition, and Type 2 diabetes, which is often linked to insulin resistance and is chronic, gestational diabetes develops during pregnancy.
Its main difference is its temporary nature; it usually goes away after pregnancy. Yet, women who have had gestational diabetes are at a higher risk of developing Type 2 diabetes later in life.
Causes and Risk Factors of Gestational Diabetes
Understanding the causes and risk factors of gestational diabetes is vital for expectant mothers. It involves hormonal changes, genetic predispositions, and pre-existing health conditions. Gestational diabetes mellitus (GDM) is a condition where high blood sugar levels are discovered during pregnancy in women not previously diagnosed with diabetes.
Hormonal Changes During Pregnancy
During pregnancy, the placenta produces hormones that help the baby grow. These hormones, though, block insulin action, leading to higher blood glucose levels. This natural insulin resistance is a key factor in the development of gestational diabetes.
Genetic Predisposition
Women with a family history of diabetes are more likely to develop gestational diabetes. This indicates a genetic component. Specific genetic markers can predispose individuals to insulin resistance and impaired insulin secretion.
Lifestyle and Pre-existing Conditions
Lifestyle factors and pre-existing health conditions significantly impact the risk of developing gestational diabetes. Key risk factors include:
- Being overweight or obese
- Having a sedentary lifestyle
- Consuming a diet high in sugars and unhealthy fats
- Having a history of gestational diabetes in a previous pregnancy
- Having polycystic ovary syndrome (PCOS)
Recognizing the Signs and Symptoms
It’s vital for expectant mothers to understand the signs and symptoms of gestational diabetes. This knowledge helps them manage their health during pregnancy. Often, gestational diabetes develops without clear symptoms, making it key for pregnant women to be vigilant about possible signs.
Common Symptoms
The symptoms of gestational diabetes can be mild and not always immediately apparent. Yet, some common indicators include:
- Increased thirst and hunger
- Frequent urination
- Fatigue
- Blurred vision
These symptoms can mimic those of a typical pregnancy, making diagnosis based on symptoms alone tricky. For more insights on managing health conditions during pregnancy, visit Acibadem International.
When Symptoms May Appear
Gestational diabetes usually develops in the second or third trimester, around 24 to 28 weeks. Symptoms may emerge gradually and subtly, highlighting the importance of regular prenatal check-ups for early detection.
Some women might not notice symptoms until the condition has advanced. So, screening for gestational diabetes is a standard part of prenatal care.
Diagnosis of Diabetes During Pregnancy (Gestational Diabetes)
Diagnosing gestational diabetes is vital for the health of both mother and baby. It involves a series of tests to check how well the body processes glucose. The diagnosis usually happens between 24 and 28 weeks of pregnancy. It can also be tested at other times based on risk factors.
Glucose Challenge Test
The glucose challenge test is a first step to identify pregnant women at risk for gestational diabetes. It involves drinking a glucose solution and then getting a blood sample to measure glucose levels. This test does not require fasting.
This test is usually done between 24 and 28 weeks of gestation. If the results show higher than normal levels, further testing may be needed.
Oral Glucose Tolerance Test
If the glucose challenge test shows a possible issue, an oral glucose tolerance test (OGTT) is done. This test requires fasting beforehand. It measures fasting blood glucose levels, then you drink a glucose solution, and blood glucose levels are measured again after one or two hours.
The OGTT is more precise than the glucose challenge test. It can diagnose gestational diabetes based on blood glucose levels.
Interpreting Test Results
Understanding the results of these tests is key to diagnosing gestational diabetes. The thresholds for diagnosis can vary slightly. But generally, higher blood glucose levels after the glucose challenge or OGTT indicate gestational diabetes.
Knowing the test results helps healthcare providers manage gestational diabetes well. This ensures the best outcomes for both mother and baby.
Effects on Maternal Health
Gestational diabetes significantly impacts maternal health, with both immediate and lasting effects. It’s vital to grasp these impacts to manage the condition effectively. This ensures the mother’s well-being.
Short-term Complications
Gestational diabetes can cause several short-term issues for the mother. These include a higher risk of preeclampsia, marked by high blood pressure and protein in the urine. Women with gestational diabetes are also more likely to need a cesarean delivery due to oversized babies.
Other short-term complications include urinary and yeast infections, common in women with gestational diabetes due to high glucose levels. Managing blood glucose levels is key to avoiding these risks.
Long-term Health Implications
The long-term health effects of gestational diabetes on mothers are profound. Women with gestational diabetes are at a higher risk of developing type 2 diabetes later in life. Research indicates that about 50% of these women will develop type 2 diabetes within 10 to 20 years post-delivery.
Also, gestational diabetes may raise the risk of cardiovascular disease. It can lead to metabolic syndrome, a group of conditions that increase the risk of heart disease, stroke, and type 2 diabetes. It’s essential for women with gestational diabetes to monitor and manage cardiovascular risk factors post-pregnancy.
Impacts on Fetal Development and Newborn Health
Understanding the implications of gestational diabetes on fetal development is critical for effective management. Gestational diabetes can impact the fetus in various ways, potentially leading to complications during pregnancy and after birth.
Risks During Pregnancy
Gestational diabetes increases the risk of several complications during pregnancy. These include:
- Macrosomia, where the baby grows too large, potentially complicating delivery.
- Polyhydramnios, an excessive amount of amniotic fluid, which can lead to preterm labor or premature rupture of membranes.
- Fetal hypoglycemia, or low blood sugar in the fetus, though less common.
Potential Birth Complications
Babies born to mothers with gestational diabetes face higher risks for certain birth complications. These can include:
- Respiratory distress syndrome, requiring additional care in a neonatal unit.
- Birth injuries, such as shoulder dystocia, due to the baby’s larger size.
- Hypoglycemia after birth, due to the baby’s increased insulin production in response to the mother’s high blood glucose levels.
Long-term Effects on the Child
The effects of gestational diabetes do not end at birth. Children born to mothers with gestational diabetes are at a higher risk of:
- Developing obesity and type 2 diabetes later in life.
- Having a higher risk of metabolic syndrome, a cluster of conditions that increase the risk of heart disease, stroke, and diabetes.
Careful management of gestational diabetes is essential to minimize these risks and ensure the best possible outcomes for both mother and child.
Nutritional Management Strategies
A well-planned diet is key in managing gestational diabetes. It helps keep blood glucose levels in check, ensuring the health of both mother and baby.
Recommended Dietary Guidelines
Women with gestational diabetes should follow a diet rich in nutrients and fiber, but low in added sugars and saturated fats. This diet should include a variety of foods such as:
- Vegetables: dark leafy greens, broccoli, and other non-starchy vegetables
- Fruits: berries, citrus fruits, and apples
- Proteins: lean meats, fish, eggs, and legumes
- Whole grains: brown rice, quinoa, and whole-wheat bread
- Dairy: low-fat milk and yogurt
Choosing complex carbohydrates over simple ones is important. Also, be mindful of carbohydrate counting.
Meal Planning and Portion Control
Effective meal planning involves eating regular meals and snacks to keep blood glucose stable. Portion control is key to avoid overeating and manage carbs. A helpful approach is to:
- Divide your plate into sections: half for vegetables, one quarter for protein, and one quarter for carbohydrates.
- Use measuring cups or a food scale to gauge portion sizes.
- Plan meals and snacks in advance to avoid unhealthy choices.
Working with a Registered Dietitian
A registered dietitian can offer personalized dietary advice and meal planning strategies. They can help in:
- Creating a customized meal plan that considers dietary restrictions and preferences.
- Educating on how to read food labels and make healthy food choices.
- Monitoring progress and adjusting the meal plan as needed.
Collaborating with a registered dietitian can greatly improve nutritional management for gestational diabetes.
Physical Activity and Exercise Recommendations
Physical activity is key in managing gestational diabetes, benefiting both mother and baby. It helps control blood sugar, improves insulin sensitivity, and lowers the risk of pregnancy complications.
Safe Exercise Options During Pregnancy
Women with gestational diabetes have several safe exercise options. Brisk walking, swimming, and prenatal yoga are low-impact and can be adjusted for pregnancy stages. It’s vital to pick activities that are enjoyable and can be maintained throughout pregnancy.
- Brisk walking: Improves cardiovascular health and can be done almost anywhere.
- Swimming: Provides a full-body workout without putting excessive strain on the joints.
- Prenatal yoga: Enhances flexibility, balance, and can help with stress management.
Creating an Exercise Routine
Creating a pregnancy exercise routine requires considering several factors. The type of exercise, frequency, and intensity are all important. Aim for at least 150 minutes of moderate-intensity aerobic activity weekly, spread over several days. It’s also key to monitor blood sugar levels before and after exercise to see how it affects glucose levels.
Before starting any new exercise program, women should consult with their healthcare provider. Discuss any necessary precautions or modifications based on their health status and pregnancy progression.
Blood Glucose Monitoring and Management
Blood glucose monitoring is key in managing gestational diabetes, ensuring both mother and baby stay healthy. It involves accurately tracking blood glucose levels and understanding what those levels should be.
Home Blood Sugar Testing
Home blood sugar testing is a vital tool for managing gestational diabetes. It uses a glucometer to measure blood glucose at various times, like waking up and after meals. This helps track how food and activities impact blood sugar.
For accurate results, it’s essential to follow glucometer instructions, calibrate it often, and keep it clean. Good hygiene is also critical when handling the device and test strips.

Target Blood Glucose Levels
Knowing the target blood glucose levels is vital for effective gestational diabetes management. The usual targets are:
- Fasting: Less than 95 mg/dL
- 1 hour after meals: Less than 140 mg/dL
- 2 hours after meals: Less than 120 mg/dL
These targets can vary based on individual health needs and healthcare provider recommendations.
Tracking and Record Keeping
Tracking and record keeping are essential in blood glucose monitoring. Keeping a log of readings, along with diet, exercise, and symptoms, helps spot patterns. This information aids in making informed decisions about managing gestational diabetes.
Many glucometers have digital memory and can upload data to computers or mobile devices. This makes tracking easier and allows for sharing data with healthcare providers during prenatal visits.
Medication and Insulin Therapy
Managing gestational diabetes sometimes requires medication or insulin to keep blood glucose levels healthy. While diet and exercise are the initial steps, some women may need more to control their blood sugar effectively.
When Medication Becomes Necessary
Medication or insulin therapy is needed when lifestyle changes alone cannot manage gestational diabetes. A healthcare provider will assess the situation and decide the best treatment plan.
- High blood glucose levels despite dietary changes and exercise
- Presence of certain risk factors or complications
- Inability to achieve target blood glucose levels through lifestyle modifications alone
Types of Insulin Used During Pregnancy
Insulin is often the preferred treatment for gestational diabetes because it’s safe for the fetus. It doesn’t cross the placenta. Various types of insulin are used, including:
- Rapid-acting insulin: Taken before meals to manage postprandial glucose spikes
- Short-acting insulin: Administered before meals and at bedtime
- Intermediate-acting insulin: Provides background insulin coverage
- Long-acting insulin: Offers a steady, prolonged release of insulin
Administration and Safety Considerations
Insulin administration requires careful planning and monitoring. Women on insulin therapy need to learn proper injection techniques, dosing, and storage. Regular blood glucose monitoring is essential to adjust insulin doses as needed.
Safety considerations include being aware of hypoglycemia signs and knowing how to treat it. Insulin doses may need to be adjusted based on diet, exercise, or other factors.
The Healthcare Team: Collaborative Management Approach
Gestational diabetes management thrives under a multidisciplinary team’s care. This team-based strategy ensures a holistic approach, aiming for the best health outcomes for both mother and child.
A team for gestational diabetes includes specialists from various fields. They collaborate to manage the condition effectively. This approach is vital for addressing the complex needs that pregnancy brings.
Obstetricians and Maternal-Fetal Medicine Specialists
Obstetricians are key in managing gestational diabetes. They oversee the pregnancy and monitor the health of both mother and fetus. Maternal-fetal medicine specialists offer additional expertise, handling high-risk cases with precision.
Endocrinologists and Diabetes Educators
Endocrinologists specialize in diabetes management, crafting treatment plans that meet individual needs. Diabetes educators educate patients on managing their condition. This includes monitoring blood glucose levels and insulin administration when needed.
Nutritionists and Other Support Professionals
Nutritionists or registered dietitians create personalized meal plans. These plans help manage blood sugar levels while ensuring the mother and fetus receive the necessary nutrients. Nurses and social workers may also join the team, providing additional care and resources.
This diverse team of healthcare professionals offers a holistic approach to care. Their collaboration improves outcomes for women with gestational diabetes.
Labor, Delivery, and Postpartum Considerations
Labor, delivery, and the postpartum period pose unique challenges for women with gestational diabetes. A detailed care plan is essential for their health and that of their baby. Effective management during these times is critical.
Delivery Planning with Gestational Diabetes
Planning for delivery is key in managing gestational diabetes. Women should discuss their options with their healthcare provider. This includes the possibility of induced labor or cesarean section if complications occur. A birth plan helps ensure the mother’s needs are met while managing risks.
Blood Sugar Management During Labor
Keeping blood sugar levels in check during labor is vital to avoid complications. Continuous glucose monitoring is often recommended. Insulin or other medications may be used to maintain safe blood glucose levels, ensuring a safe delivery.
Postpartum Blood Sugar Changes
After delivery, blood sugar levels usually return to normal. Yet, women with gestational diabetes are at higher risk of developing type 2 diabetes later. Postpartum care includes monitoring blood glucose and discussing long-term health strategies with a healthcare provider. Breastfeeding is encouraged, as it benefits both mother and baby, including a lower risk of type 2 diabetes for the mother.
Emotional and Psychological Aspects of Gestational Diabetes
Gestational diabetes is more than a medical condition; it’s a deeply personal journey. It brings a mix of emotions, from denial and anxiety to fear about the future. Understanding and support are key to navigating this emotional landscape.
Coping with Diagnosis and Management
Coming to terms with the diagnosis requires a deep understanding of the condition. Expectant mothers are advised to learn about gestational diabetes, its management, and its impact on pregnancy. This knowledge empowers them to cope better.
Healthcare providers are essential in this journey. They offer guidance and reassurance, helping to develop a management plan that suits the individual’s lifestyle. This makes managing the condition more feasible.
Support Systems and Resources
A robust support system is critical for managing the emotional toll of gestational diabetes. This includes family, friends, and support groups. These networks allow women to share their experiences and find solace.
- Family support offers both emotional comfort and practical assistance.
- Support groups provide a community of peers facing similar challenges.
- Online resources and forums offer additional information and support.
Addressing Anxiety and Stress
Managing anxiety and stress is vital for overall well-being. Techniques like mindfulness, meditation, and yoga can help alleviate stress. These practices promote relaxation and reduce anxiety levels.
Self-care is also essential for expectant mothers. Engaging in activities that bring joy and relaxation is important. For those needing extra support, professional help like counseling or therapy is available.
Living Well Beyond Gestational Diabetes: Long-term Health Strategies
Experiencing gestational diabetes calls for adopting long-term health strategies to avoid Type 2 diabetes. Lifestyle changes are key to maintaining health and well-being.
Women who’ve had gestational diabetes should aim for a healthy weight, eat a balanced diet, and stay active. These habits not only boost health but also lower the risk of Type 2 diabetes later on.
Eating a diet full of whole foods like fruits, vegetables, whole grains, and lean proteins is essential. Regular exercise, such as walking or swimming, helps manage blood sugar and improves insulin sensitivity.
Regular health check-ups are vital for monitoring health after gestational diabetes. By making smart lifestyle choices and staying proactive, women can greatly reduce their risk of Type 2 diabetes and keep their overall health in check.
FAQ About Gestational Diabetes
Q: What is gestational diabetes?
A: Gestational diabetes is a condition where blood sugar levels spike during pregnancy. It typically appears in the second or third trimester. Hormonal changes, insulin resistance, and liver glucose production are the main culprits.
Q: What are the risk factors for developing gestational diabetes?
A: Several factors increase the risk of gestational diabetes. These include a family history of diabetes, being overweight or obese, and a history of gestational diabetes in previous pregnancies. Being over 35 years old, having a history of delivering large babies, or having polycystic ovary syndrome (PCOS) also raise the risk.
Q: How is gestational diabetes diagnosed?
A: Diagnosis involves a glucose challenge test or an oral glucose tolerance test. The glucose challenge test measures blood sugar after a sugary drink. The oral glucose tolerance test checks blood sugar after fasting and then consuming a sugary drink.
Q: What are the symptoms of gestational diabetes?
A: Symptoms may include increased thirst and urination, fatigue, blurred vision, and recurring infections. Yet, many women with gestational diabetes show no symptoms at all.
Q: How is gestational diabetes managed?
A: Management includes dietary changes, physical activity, and sometimes insulin therapy or medication. Women work with their healthcare team to create a personalized plan.
Q: What are the risks associated with gestational diabetes?
A: Gestational diabetes can lead to complications like preeclampsia, premature birth, and the need for cesarean delivery. It also increases the risk of Type 2 diabetes later in life.
Q: How does gestational diabetes affect the baby?
A: It can lead to complications such as macrosomia, birth trauma, and neonatal hypoglycemia. It may also increase the risk of obesity and Type 2 diabetes in the baby later on.
Q: Can gestational diabetes be prevented?
A: While prevention is not guaranteed, maintaining a healthy weight, staying active, and eating a balanced diet can help. Early prenatal care and screening are also key to early detection and management.
Q: What is the postpartum follow-up for gestational diabetes?
A: Postpartum, women should have their blood glucose levels checked to ensure they return to normal. They should also be screened for Type 2 diabetes at regular intervals in the following years.
Q: How can women with a history of gestational diabetes reduce their risk of developing Type 2 diabetes?
A: To reduce the risk of Type 2 diabetes, women should maintain a healthy weight, stay active, eat a balanced diet, and get regular check-ups with their healthcare provider.















