Diabetic Nephropathy: What is Diabetic Nephropathy?
Diabetic Nephropathy is a severe complication of diabetes, impacting the kidneys’ function. It hampers their ability to filter waste from the blood. If not managed, it can lead to kidney failure. For those with diabetes, managing Diabetic Nephropathy is essential. Early detection and treatment can slow the disease’s progression. This reduces the risk of kidney failure and the need for dialysis or a transplant.
Understanding the risks and taking proactive steps is key. It helps individuals with diabetes keep their kidneys healthy and maintain overall well-being. Exploring Diabetic Nephropathy reveals how diabetes affects kidney function. It’s a serious complication of diabetes, impairing the kidneys’ ability to filter waste from the blood.
Definition and Prevalence in the United States
Diabetic Nephropathy is kidney damage or disease caused by diabetes. It’s a major cause of chronic kidney disease and end-stage renal disease in the U.S. The CDC reports that diabetes is behind about 44% of new kidney failure cases. With 34 million people in the U.S. living with diabetes, the prevalence of Diabetic Nephropathy is significant.
The Kidney-Diabetes Connection
The kidneys and diabetes are closely linked. Prolonged high blood glucose levels can harm the blood vessels in the kidneys. This reduces their function. Such damage can lead to protein leakage into the urine, known as albuminuria. If not managed, it can cause more severe kidney damage. Effective diabetes management is key to preventing or slowing Diabetic Nephropathy.
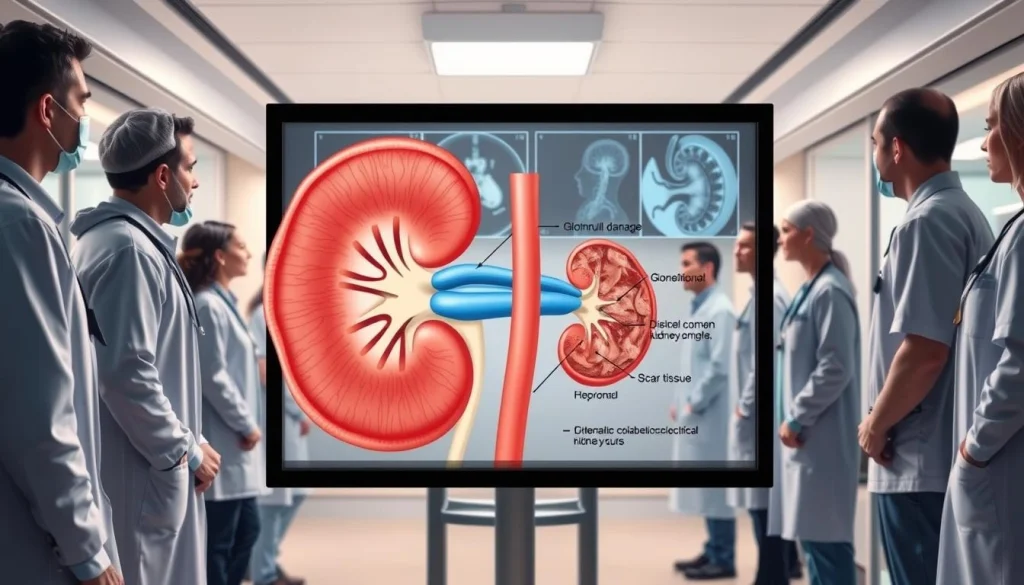
Pathophysiology of Diabetic Nephropathy
The pathophysiology of Diabetic Nephropathy is complex, involving metabolic and hemodynamic changes. These changes ultimately cause kidney damage.
Glomerular Changes and Basement Membrane Thickening
In Diabetic Nephropathy, the glomeruli undergo hypertrophy and hyperfiltration. This can cause the basement membrane to thicken. Such thickening disrupts the glomerular filtration barrier, allowing proteins to leak into the urine.
Hemodynamic Alterations
Hemodynamic changes, like increased glomerular pressure and blood flow, are key in Diabetic Nephropathy’s development. These changes can damage the glomeruli. They are often linked to hypertension, a common condition in diabetic patients.
Metabolic Pathways and Inflammatory Processes
Advanced glycosylation end-products (AGEs) and metabolic pathways activation contribute to inflammation in Diabetic Nephropathy. These processes worsen kidney damage by promoting fibrosis and vascular dysfunction.
Grasping these mechanisms is vital for creating effective treatments. It’s essential to slow or halt Diabetic Nephropathy’s progression.
Risk Factors for Developing Diabetic Nephropathy
Understanding the risk factors for Diabetic Nephropathy is key to managing diabetes effectively. Several factors contribute to its development. Identifying these can help prevent or delay its onset.
Uncontrolled Blood Glucose
Uncontrolled blood glucose levels are a major risk factor for Diabetic Nephropathy. High blood sugar damages the kidneys’ blood vessels, impairing their function. It’s vital to keep blood glucose within target ranges to prevent kidney damage.
Hypertension and Cardiovascular Disease
Hypertension, or high blood pressure, is another significant risk factor. It damages the kidneys’ blood vessels, reducing their function. Cardiovascular disease, common in people with diabetes, also increases kidney disease risk.
Genetic Predisposition
Genetic factors also play a role in susceptibility to Diabetic Nephropathy. Those with a family history of kidney disease or diabetes are at higher risk. Understanding genetic predisposition aids in early identification and management.
Duration of Diabetes and Age of Onset
The duration of diabetes and the age at diagnosis are critical risk factors. The longer a person has diabetes, the higher their risk of Diabetic Nephropathy. Early onset diabetes increases the risk of complications, including kidney disease, later in life.
The Five Stages of Diabetic Nephropathy
The progression of diabetic nephropathy is divided into five stages, from initial hyperfiltration to end-stage renal disease. Understanding these stages is vital for effective disease management.
Stage 1: Hyperfiltration and Kidney Enlargement
In the first stage, the kidneys experience hyperfiltration, leading to kidney enlargement. This stage is characterized by an increase in glomerular filtration rate (GFR).
Stage 2: Silent Stage with Basement Membrane Thickening
The second stage is often silent, with patients not exhibiting noticeable symptoms. Yet, there is a thickening of the basement membrane, which is a critical indicator of disease progression.
Stage 3: Microalbuminuria
At this stage, patients begin to exhibit microalbuminuria, which is the presence of small amounts of albumin in the urine. This is an early warning sign that can be detected through urine tests.
Stage 4: Overt Nephropathy with Macroalbuminuria
The fourth stage is marked by overt nephropathy, characterized by macroalbuminuria, where larger amounts of albumin are present in the urine. This indicates significant kidney damage.
Stage 5: End-Stage Renal Disease
The final stage is end-stage renal disease (ESRD), where the kidneys have lost nearly all their ability to function. Patients at this stage require renal replacement therapy.
Here is a summary of the key characteristics of the five stages:
- Stage 1: Hyperfiltration and kidney enlargement
- Stage 2: Basement membrane thickening without symptoms
- Stage 3: Presence of microalbuminuria
- Stage 4: Macroalbuminuria and overt nephropathy
- Stage 5: End-stage renal disease requiring renal replacement therapy
Clinical Manifestations and Symptoms
Recognizing the symptoms of Diabetic Nephropathy is vital for timely intervention. This condition evolves through stages, often without noticeable symptoms until it has progressed significantly.
Early Warning Signs
Identifying Diabetic Nephropathy early is key to preventing its progression. Key indicators include microalbuminuria and slight blood pressure fluctuations.
Microalbuminuria Detection
Microalbuminuria, the presence of small albumin amounts in urine, signals early kidney damage. Regular screenings for microalbuminuria are critical for early detection.
Subtle Changes in Blood Pressure
Hypertension or slight blood pressure changes can indicate Diabetic Nephropathy onset. Regular blood pressure monitoring is essential for early detection.
Advanced Symptoms
As Diabetic Nephropathy advances, more evident symptoms emerge. These include edema, fluid retention, and uremic symptoms.
Edema and Fluid Retention
Edema, or swelling, in the legs and feet, and fluid retention are common in advanced Diabetic Nephropathy. This is due to the kidneys’ reduced ability to remove fluid.
Uremic Symptoms
Uremic symptoms, such as nausea, vomiting, and fatigue, occur when waste products accumulate in the blood. This happens due to the kidneys’ decreased function.
Diagnostic Approaches for Diabetic Nephropathy
To diagnose Diabetic Nephropathy, healthcare providers employ a variety of tests. These tests assess kidney function and detect damage. Early detection and monitoring are critical.
Urine Tests for Albumin
Urine tests are essential for detecting albumin, a protein that signals kidney damage. The presence of albumin in urine is an early indicator of Diabetic Nephropathy.
Spot Urine Albumin-to-Creatinine Ratio
The spot urine albumin-to-creatinine ratio is a convenient test. It measures albumin levels against creatinine in a single sample. This test helps gauge the severity of kidney damage.
24-Hour Urine Collection
A 24-hour urine collection test measures total albumin excreted over 24 hours. It offers a detailed assessment of kidney function.
Blood Tests for Kidney Function
Blood tests evaluate kidney function by measuring waste products in the blood. These tests help determine the extent of kidney damage.
eGFR Measurement
The estimated Glomerular Filtration Rate (eGFR) is a key test. It estimates the rate at which waste is filtered through the kidneys. A lower eGFR indicates poorer kidney function.
Creatinine and BUN Levels
Creatinine and Blood Urea Nitrogen (BUN) levels are measured to assess kidney function. Elevated levels indicate impaired kidney function.
Imaging and Biopsy Considerations
In some cases, imaging tests or kidney biopsy may be necessary. These tests provide valuable information for diagnosis and treatment planning.
Glycemic Control in Managing Diabetic Nephropathy
Maintaining tight glycemic control is essential for slowing the progression of Diabetic Nephropathy. Effective glycemic control helps in reducing the strain on the kidneys and delaying the onset of complications associated with diabetes.
Target HbA1c Levels for Kidney Protection
Targeting the right HbA1c levels is critical for kidney protection in diabetic patients. The American Diabetes Association recommends an HbA1c target of less than 7% for most adults. Adjustments may be necessary based on individual patient factors, such as the risk of hypoglycemia.
- HbA1c levels should be monitored regularly to ensure they remain within the target range.
- Tighter control (HbA1c
Continuous Glucose Monitoring Benefits
Continuous Glucose Monitoring (CGM) systems provide real-time data on glucose levels. This helps patients and healthcare providers make informed decisions about diabetes management.
- CGM can help identify glucose patterns and trends, enabling proactive adjustments to treatment plans.
- It can also reduce the risk of hypoglycemic events by alerting patients to low glucose levels.
- CGM data can be used to optimize insulin dosing and improve overall glycemic control.
Insulin Management Strategies
Effective insulin management is critical for achieving and maintaining glycemic control. Several strategies are available, including multiple daily injections and insulin pump therapy.
Multiple Daily Injections
Multiple daily injections involve administering insulin multiple times a day to mimic the body’s natural insulin production. This approach requires careful planning and coordination.
- It allows for flexibility in managing glucose levels throughout the day.
- Requires accurate carbohydrate counting and insulin dosing.
Insulin Pump Therapy
Insulin pump therapy involves wearing a small device that delivers insulin continuously throughout the day. It offers more precise control over insulin delivery.
- Pumps can be programmed to deliver different basal rates throughout the day.
- They also allow for bolus doses to be administered at mealtimes.
Blood Pressure Management for Renal Protection
Managing high blood pressure is key to protecting kidney function in those with Diabetic Nephropathy. High blood pressure can speed up kidney disease progression. It’s a vital aspect of treatment.
Target Blood Pressure Goals in Diabetic Kidney Disease
The American Diabetes Association suggests a blood pressure goal of less than 140/90 mmHg for Diabetic Nephropathy patients. For some, aiming for less than 130/80 mmHg might be more suitable, based on individual risk and health.
Reaching these goals requires ongoing monitoring and adjustments to treatment plans.
First-Line Antihypertensive Medications
ACE inhibitors or ARBs are the first choice for hypertension treatment in Diabetic Nephropathy. These drugs offer kidney protection beyond lowering blood pressure.
They reduce kidney pressure and decrease urine protein loss.
Combination Therapy Approaches
Often, one medication isn’t enough to hit blood pressure targets. Combination therapy with different types of blood pressure medications is common.
Typical combinations include ACE inhibitors or ARBs with diuretics, calcium channel blockers, or beta-blockers.
Pharmacological Interventions for Diabetic Nephropathy
Managing Diabetic Nephropathy requires a multi-faceted approach. This includes pharmacological interventions aimed at slowing disease progression. Different medications have been found to protect the kidneys and improve patient outcomes.
ACE Inhibitors and ARBs Mechanisms
ACE inhibitors and ARBs are key treatments for Diabetic Nephropathy. They block the renin-angiotensin-aldosterone system (RAAS). This action reduces intraglomerular pressure and proteinuria. It not only slows kidney disease but also offers cardiovascular benefits.
- Reduce proteinuria
- Lower blood pressure
- Slow kidney disease progression
SGLT2 Inhibitors and Kidney Outcomes
SGLT2 inhibitors are a significant advancement in Diabetic Nephropathy treatment. They reduce glucose reabsorption in the kidneys. This decrease in hyperfiltration and intraglomerular pressure protects the kidneys.
GLP-1 Receptor Agonists
GLP-1 receptor agonists offer benefits for Diabetic Nephropathy patients. They improve blood sugar control, promote weight loss, and reduce cardiovascular events. They also slow kidney disease progression.
Emerging Drug Therapies in Clinical Trials
New drug therapies are being explored for Diabetic Nephropathy. These include novel RAAS inhibitors, anti-inflammatory agents, and innovative compounds. They target specific pathways involved in kidney damage.
- Novel RAAS inhibitors
- Anti-inflammatory agents
- Innovative compounds targeting kidney damage pathways
In conclusion, pharmacological interventions are vital in Diabetic Nephropathy management. Understanding the mechanisms and benefits of various medications helps healthcare providers tailor treatment plans. This approach improves kidney outcomes for individual patients.
Dietary Modifications for Kidney Protection
For those with Diabetic Nephropathy, specific dietary changes can greatly benefit kidney health. A well-thought-out diet can manage the condition and slow kidney damage progression.
Protein Intake Recommendations
Protein intake is key for individuals with Diabetic Nephropathy. The type and amount of protein consumed can impact kidney function.
Plant vs. Animal Protein Sources
Plant-based proteins, like beans, lentils, and tofu, are often preferred. They are lower in saturated fats and higher in fiber than animal proteins. Increasing plant-based proteins can ease kidney strain.
Calculating Optimal Protein Needs
The right protein amount varies by age, weight, and kidney disease stage. A moderate protein intake is generally advised. Healthcare providers or dietitians can help determine the exact needs.
Sodium Restriction Strategies
Reducing sodium intake is vital for managing blood pressure and preventing further kidney damage. Limiting high-sodium foods and using herbs and spices for flavor instead of salt is effective.
Phosphorus and Potassium Management
Those with Diabetic Nephropathy may need to limit phosphorus and potassium intake. Kidney damage can cause imbalances in these minerals. Working with healthcare providers to monitor and adjust dietary intake is critical.
Lifestyle Interventions and Their Impact
The role of lifestyle interventions in managing Diabetic Nephropathy is immense. Adopting healthy habits can greatly slow kidney disease progression. This is a key aspect of managing the condition.
Exercise Benefits and Recommendations
Exercise is vital for Diabetic Nephropathy management. It enhances blood sugar control and maintains blood pressure. It also lowers the risk of heart disease.
Aerobic Exercise Guidelines
Aerobic activities, like walking, cycling, or swimming, are essential. Aim for 150 minutes weekly. This can be achieved with 30 minutes daily, five days a week.
Resistance Training Considerations
Resistance training, done twice a week, boosts muscle and strength. It includes weightlifting or bodyweight exercises. This is in addition to aerobic exercises.
Smoking Cessation and Alcohol Moderation
Quitting smoking is critical for Diabetic Nephropathy patients. Smoking hastens kidney damage. Also, limiting alcohol intake is advised. Excessive drinking harms kidney health.
By embracing these lifestyle changes, Diabetic Nephropathy patients can enhance their health. They can also slow their kidney disease progression.
Complications Associated with Diabetic Nephropathy
Diabetic nephropathy brings a host of complications that greatly affect patient outcomes. These issues fall into cardiovascular, hematological, and metabolic disorders. Each category presents unique challenges for those affected.
Cardiovascular Complications and Risk Stratification
Cardiovascular disease is a significant complication of diabetic nephropathy. Patients with this condition face a higher risk of heart-related events. Tools like the Framingham Risk Score help identify those at greatest risk.
- Hypertension management
- Lipid control
- Antiplatelet therapy
Anemia and Bone Mineral Disease
Anemia and bone mineral disease are common in diabetic nephropathy patients. Anemia stems from reduced erythropoietin production. Bone mineral disease arises from calcium and phosphate metabolism issues.
Electrolyte Imbalances and Metabolic Acidosis
Advanced diabetic nephropathy often leads to electrolyte imbalances, like hyperkalemia, and metabolic acidosis. Managing these requires close monitoring and adjustments to diet and medication.
Renal Replacement Therapy Options
For those with advanced Diabetic Nephropathy, renal replacement therapy is essential. It involves treatments that replace kidney function when it fails. These therapies are designed to manage the condition effectively.
Hemodialysis Modalities
Hemodialysis is a key form of renal replacement therapy. It filters blood outside the body to remove waste. There are several methods for undergoing hemodialysis.
In-Center Hemodialysis
In-center hemodialysis requires patients to visit a dialysis center several times a week. It offers a structured environment with medical supervision.
Home Hemodialysis
Home hemodialysis allows patients to dialyze in their own homes. This option provides more flexibility and can lead to better health outcomes due to more frequent dialysis.
Peritoneal Dialysis Techniques
Peritoneal dialysis uses the peritoneum in the abdomen as a membrane for exchanging fluids and dissolved substances. It serves as an alternative to hemodialysis.
- Continuous Ambulatory Peritoneal Dialysis (CAPD)
- Automated Peritoneal Dialysis (APD)
Kidney Transplantation Considerations
Kidney transplantation is the best option for eligible patients, improving survival and quality of life. Patients can explore kidney transplantation as a viable treatment.
Living vs. Deceased Donor
The choice between a living and deceased donor kidney transplant depends on several factors. These include the availability of a living donor and the patient’s health condition.
Post-Transplant Management
After a kidney transplant, patients need lifelong immunosuppressive therapy. They also require regular follow-ups to monitor graft function and manage complications.
Special Considerations for Vulnerable Populations
Diabetic Nephropathy impacts different populations in distinct ways, requiring tailored approaches for vulnerable groups. Its effects are most pronounced in pediatric and elderly patients. These groups face unique challenges in managing and treating the condition.
Pediatric Patients with Diabetic Nephropathy
Pediatric patients with Diabetic Nephropathy need meticulous care to slow disease progression. Key considerations include:
- Monitoring kidney function through regular urine tests and blood work
- Maintaining tight glycemic control to prevent further kidney damage
- Adjusting treatment plans as the child grows and develops
Effective management in pediatric patients involves a multidisciplinary team. This team includes pediatric nephrologists, endocrinologists, and dietitians. Family support and education are also vital in helping young patients stick to their treatment plans.
Elderly Patients with Multiple Comorbidities
Elderly patients with Diabetic Nephropathy often have multiple comorbidities, making their care more complex. Important considerations include:
- Managing hypertension and cardiovascular disease
- Adjusting medication regimens to account for decreased kidney function
- Monitoring for signs of anemia and bone mineral disease
In elderly patients, a holistic care plan is essential. It should address Diabetic Nephropathy and other comorbid conditions. This approach aims to enhance overall health outcomes and improve quality of life.
Preventive Strategies and Early Intervention
Understanding and implementing preventive strategies and early intervention techniques are key to managing Diabetic Nephropathy. These methods can significantly slow the disease’s progression. Effective prevention and early intervention are essential.
Screening Recommendations and Frequency
Regular screening for Diabetic Nephropathy is critical for early detection. The American Diabetes Association suggests annual screening for microalbuminuria. This is recommended for patients with Type 1 diabetes after 5 years of diagnosis. It also applies to all patients with Type 2 diabetes from the start.
- Annual urine albumin-to-creatinine ratio test
- Serum creatinine test to estimate GFR
- Blood pressure monitoring
Multidisciplinary Care Approach
A multidisciplinary care approach is vital for managing Diabetic Nephropathy effectively. It involves coordination among various healthcare professionals.
Role of Nephrologists
Nephrologists are critical in managing Diabetic Nephropathy, mainly in advanced stages. They assist in diagnostic procedures and in creating a treatment plan.
Coordination with Endocrinologists
Coordination with endocrinologists is essential for managing diabetes and its complications. Endocrinologists are key in optimizing glycemic control. This is vital for preventing Diabetic Nephropathy progression.
Living Well with Diabetic Kidney Disease
Diabetic Nephropathy, a serious complication of diabetes, requires a holistic approach to slow disease progression and maintain quality of life. Patient empowerment is key, enabling individuals to actively participate in their care.
Managing kidney disease involves making informed lifestyle choices, following medication regimens, and monitoring health indicators regularly. Patients can better handle the challenges of Diabetic Nephropathy by understanding their condition and the necessary management strategies.
Effective management of Diabetic Nephropathy includes controlling blood glucose levels, managing blood pressure, and adopting a kidney-friendly diet. These actions not only slow kidney disease progression but also reduce the risk of cardiovascular complications.
Support from healthcare providers, family, and support groups is essential for patient empowerment. They offer emotional support and practical guidance. With these resources, individuals with Diabetic Nephropathy can lead active and fulfilling lives despite their condition.
FAQ
Q: What is Diabetic Nephropathy?
A: Diabetic Nephropathy is a severe kidney issue linked to diabetes. It causes kidney damage, leading to reduced function and possibly complete kidney failure.
Q: What are the risk factors for developing Diabetic Nephropathy?
A: Risk factors include high blood sugar, high blood pressure, genetic factors, and long-standing diabetes.
Q: How is Diabetic Nephropathy diagnosed?
A: Diagnosis involves urine tests for albumin, blood tests for kidney function, and sometimes imaging or biopsy.
Q: What is the role of glycemic control in managing Diabetic Nephropathy?
A: Controlling blood sugar is key in managing Diabetic Nephropathy. It helps slow kidney damage. Target HbA1c levels, use of continuous glucose monitoring, and insulin management are vital.
Q: How can lifestyle interventions impact Diabetic Nephropathy?
A: Lifestyle changes like exercise, quitting smoking, and drinking less alcohol can help. They reduce complications and slow disease progression.
Q: What are the complications associated with Diabetic Nephropathy?
A: Complications include heart issues, anemia, bone disease, electrolyte imbalances, and metabolic acidosis.
Q: What are the renal replacement therapy options for advanced Diabetic Nephropathy?
A: Options include hemodialysis, peritoneal dialysis, and kidney transplantation for advanced cases.
Q: How can patients live well with Diabetic Nephropathy?
A: Patients can manage their condition with a team approach, a healthy lifestyle, and following treatment plans.















