Facet Joint Syndrome: Anatomy and Biomechanics of the Spine
Facet Joint Syndrome is a condition that affects the spine, causing pain and discomfort. Understanding this condition is key for effective management and treatment. The condition occurs when the facet joints in the spine become inflamed or irritated. This leads to various symptoms. Causes can range from injury to degenerative changes. This guide will explore the causes, symptoms, and treatments of Facet Joint Syndrome. It aims to provide valuable insights for those affected by this condition.
Understanding Facet Joints and Their Function
Grasping the concept of facet joints is key to understanding the spinal column’s mechanics. These small stabilizing joints are situated between and behind adjacent vertebrae. They are vital for the spine’s flexibility and stability.
Anatomy of Facet Joints
The anatomy of facet joints is intricately complex, involving both structure and function. Formed by the articulation of the superior and inferior articular processes of adjacent vertebrae, these joints are synovial. They contain a synovial membrane that produces fluid, reducing friction and enabling smooth movement.
- The superior articular process faces backward and upward.
- The inferior articular process faces forward and downward.
- The joints are covered with cartilage, facilitating smooth articulation.
Role in Spinal Movement and Stability
Facet joints are integral to spinal movement and stability. They guide the spine’s movement, allowing for flexion, extension, rotation, and lateral bending. They also provide stability to the spinal column. The orientation of the facet joints varies along the spine, influencing the type and range of motion at different spinal levels.
- In the cervical spine, facet joints are oriented to allow for a wide range of motion.
- In the lumbar spine, they are oriented to provide stability and support heavy loads.
- Their structure helps in distributing loads and stresses across the spine.
Facet Joint Syndrome: Definition and Overview
Facet Joint Syndrome is a major source of back pain, requiring a close look at its definition and who it affects. This condition impacts the facet joints in the spine, causing pain and discomfort. Knowing its clinical definition and how common it is is key for proper diagnosis and treatment.
Clinical Definition
Facet Joint Syndrome is marked by pain and inflammation in the facet joints. These joints are vital for spinal flexibility and stability. Symptoms include localized pain, stiffness, and a reduced range of motion. Diagnosing this condition involves both clinical evaluation and imaging studies.
The syndrome is linked to degenerative changes, trauma, or repetitive strain on the facet joints. A clear clinical definition is vital for distinguishing Facet Joint Syndrome from other back pain causes. Key diagnostic criteria include pain patterns, response to diagnostic injections, and imaging findings.
- Pain localized to the facet joint area
- Stiffness and limited mobility
- Pain exacerbated by specific movements
Prevalence and Demographics
Facet Joint Syndrome is widespread, affecting many people, with its prevalence rising with age. It is a major contributor to chronic back pain in older adults, studies show.
Demographically, it impacts both genders, though some studies suggest a slightly higher prevalence in women. Jobs that involve heavy lifting or bending also increase the risk of developing Facet Joint Syndrome.
- Age: Prevalence increases with age
- Gender: Slightly more common in women
- Occupation: Higher risk in jobs involving heavy physical labor
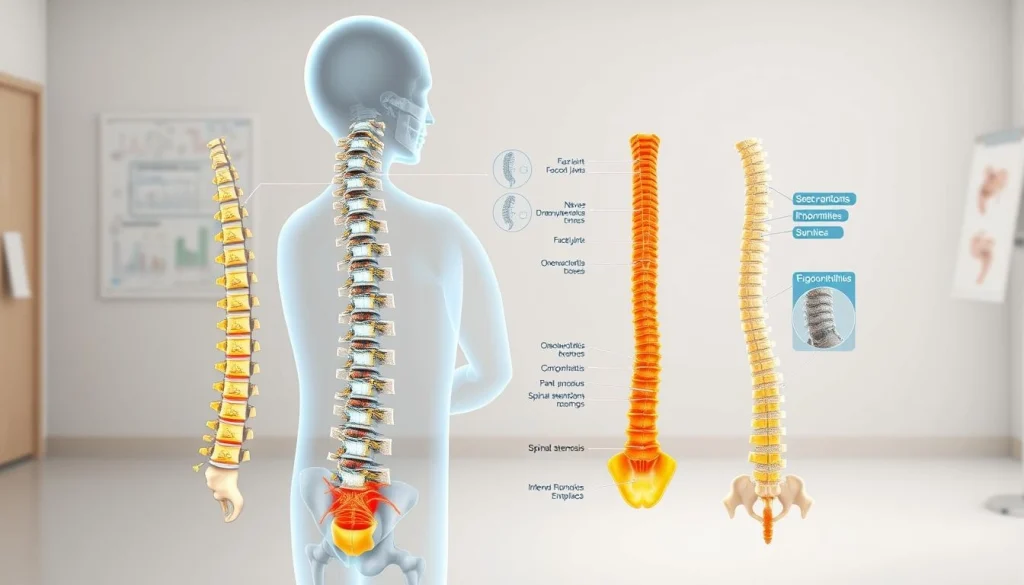
Anatomy and Biomechanics of the Spine
Grasping the anatomy and biomechanics of the spine is key for diagnosing and treating spinal issues. The spine, a complex structure, supports the body, enables movement, and safeguards vital neural elements.

Vertebral Column Structure
The vertebral column, made up of 33 vertebrae, is divided into five sections: cervical, thoracic, lumbar, sacrum, and coccyx. Vertebrae stack atop each other, with intervertebral discs serving as shock absorbers. This setup allows for both flexibility and support.
- Cervical vertebrae support the head and enable neck movement.
- Thoracic vertebrae are attached to the ribs, forming the thoracic cage.
- Lumbar vertebrae bear the majority of the body’s weight.
How Facet Joints Work
Facet joints, also known as zygapophysial joints, are synovial joints between the articular processes of adjacent vertebrae. They guide the movement of the spine and provide stability, mainly during rotational movements. The facet joints work in tandem with the intervertebral discs to facilitate smooth spinal motion.
Load Distribution in the Spine
The spine distributes loads through a combination of vertebral bodies, intervertebral discs, and facet joints. The vertebral bodies and discs handle the majority of the compressive load. Facet joints help guide and stabilize the spine during various movements. Proper load distribution is vital for preventing excessive wear and tear on spinal components.
- Vertebral bodies and discs bear the majority of the compressive load.
- Facet joints share some of the load, mainly during extension and rotation.
- Abnormal load distribution can lead to conditions like Facet Joint Syndrome.
Common Causes of Facet Joint Pain
Understanding the causes of facet joint pain is key to effective management and treatment. Facet joint pain can stem from various sources. Identifying the underlying cause is vital for a targeted treatment plan.
Age-Related Degeneration
Age-related degeneration is a common cause of facet joint pain. As people age, the facet joints naturally wear and tear, leading to degenerative changes. This can cause pain and stiffness. Bone spurs and thickened ligaments can further contribute to pain.
Traumatic Injuries
Traumatic injuries, like those from a car accident or a fall, can also cause facet joint pain. These injuries can lead to inflammation and irritation of the facet joints. This results in pain and discomfort. In some cases, traumatic injuries can cause micro-fractures or other damage to the facet joints, leading to chronic pain.
Osteoarthritis
Osteoarthritis is another significant contributor to facet joint pain. This degenerative joint disease can affect the facet joints, leading to pain, stiffness, and limited mobility. Osteoarthritis can cause the cartilage in the facet joints to break down, resulting in bone-on-bone contact and pain.
Other Contributing Factors
Other factors can contribute to facet joint pain, including:
- Poor posture or biomechanics
- Repetitive strain or overuse
- Genetic predisposition
- Previous spinal surgery or conditions
These factors can increase the risk of developing facet joint pain and can exacerbate existing conditions. Understanding these contributing factors is essential for developing an effective treatment plan.
Risk Factors for Developing Facet Joint Syndrome
Some people are more likely to get Facet Joint Syndrome due to various factors. These include demographic, lifestyle, and occupational elements. Knowing these risk factors can aid in preventing and managing the condition early on.
Age and Gender Considerations
Age is a key risk factor for Facet Joint Syndrome, with older adults more commonly affected. This is because facet joints naturally degenerate with age. Gender also influences the risk, with women more likely to develop the syndrome, possibly due to hormonal changes post-menopause.
Lifestyle Factors
Lifestyle choices greatly impact the risk of Facet Joint Syndrome. A sedentary lifestyle weakens back muscles and leads to poor posture, straining facet joints. On the other hand, jobs involving heavy lifting or repetitive bending also increase the risk.
Occupational Hazards
Jobs with manual labor, heavy lifting, or prolonged sitting or standing raise the risk of Facet Joint Syndrome. Workers in jobs requiring frequent twisting, bending, or overhead reaching face additional stress on their facet joints. This makes them more prone to the condition.
Recognizing Symptoms of Facet Joint Syndrome
Identifying Facet Joint Syndrome symptoms is the first step towards managing the condition and improving quality of life. This condition affects the spine and surrounding areas, manifesting through various symptoms.
Pain Patterns and Characteristics
The pain from Facet Joint Syndrome is usually localized to the affected joint area. It can feel like a dull ache or sharp pain, often getting worse with specific movements or activities.
Pain can occur on one side of the spine or spread to areas like the buttocks or thighs. The pattern of pain helps healthcare providers distinguish Facet Joint Syndrome from other spinal conditions.
Movement Limitations
Facet Joint Syndrome can cause reduced mobility and stiffness in the spine area. Patients may struggle with certain movements or activities due to pain or stiffness.
The extent of movement limitations varies based on the condition’s severity and the facet joints involved. Some people may feel stiffer after resting or being inactive.
Differentiating from Other Back Conditions
Distinguishing Facet Joint Syndrome from other back conditions is vital for proper treatment. Symptoms can overlap with other spinal disorders, requiring a detailed diagnosis.
Healthcare providers use clinical evaluation, patient history, and diagnostic tests to differentiate Facet Joint Syndrome from conditions like herniated discs, spinal stenosis, or degenerative disc disease.
Understanding Facet Joint Syndrome symptoms is essential for an accurate diagnosis and effective management plan.
Diagnostic Approaches for Facet Joint Syndrome
Diagnosing Facet Joint Syndrome involves a detailed process. It combines clinical assessments and imaging studies. This approach is key to accurately identifying the condition and excluding other back pain causes.
Physical Examination Techniques
Physical exams are vital in diagnosing Facet Joint Syndrome. Healthcare professionals use palpation to find tender spots. They also conduct range of motion tests to check flexibility and pain during movement. Specific maneuvers are used to trigger facet joint pain.
These methods help doctors pinpoint the pain source and measure its impact on function.
Imaging Studies
Imaging studies are essential for confirming Facet Joint Syndrome diagnosis. They help evaluate joint degeneration. MRI, CT scans, and X-rays are commonly used. MRI shows soft tissue and inflammation, CT scans reveal bony details, and X-rays check spinal alignment.
Together, these images provide a complete picture for an accurate diagnosis.
Diagnostic Nerve Blocks
Diagnostic nerve blocks are a valuable tool in diagnosing Facet Joint Syndrome. By injecting an anesthetic into facet joint nerves, doctors can confirm if the joints are causing pain. If pain relief is significant, it supports the Facet Joint Syndrome diagnosis.
Using these diagnostic methods together ensures a precise diagnosis. It also guides the best treatment options for Facet Joint Syndrome patients.
Conservative Treatment Options
For those dealing with Facet Joint Syndrome, conservative treatments are key to managing pain and improving life quality. These non-surgical methods are the initial approach. They aim to lessen pain, boost mobility, and enhance spinal health.
Physical Therapy Approaches
Physical therapy is essential in managing Facet Joint Syndrome conservatively. A customized exercise plan can strengthen muscles, enhance flexibility, and decrease pain. Manual therapy, including massage and joint mobilization, also offers benefits.
Therapists teach patients about proper posture and body mechanics to lessen facet joint strain. This improves spinal mobility and strength, aiding in Facet Joint Syndrome management.
Medication Management
Medication management is a critical part of Facet Joint Syndrome treatment. Over-the-counter pain relievers like acetaminophen or ibuprofen can manage pain and inflammation. For some, prescription medications like muscle relaxants or oral steroids might be suggested for short-term use.
It’s vital for patients to collaborate with their healthcare provider to find the most effective medication plan with minimal side effects. Medication should be part of a broader conservative treatment strategy for best results.
Lifestyle Modifications
Lifestyle changes are vital for effectively managing Facet Joint Syndrome. Maintaining a healthy weight reduces spinal load, including facet joints. Regular, low-impact exercises like walking or swimming also help manage symptoms.
Further, ergonomic adjustments in daily activities and workspaces can reduce spinal strain. Simple actions, like stretching regularly and improving sitting posture, can significantly aid in managing Facet Joint Syndrome.
Interventional Procedures for Pain Relief
For those with Facet Joint Syndrome, interventional procedures offer a ray of hope when traditional treatments fall short. These methods aim directly at the facet joints, aiming to alleviate chronic pain for those in need.
Facet Joint Injections
Facet joint injections are a prevalent treatment for Facet Joint Syndrome. They involve injecting a local anesthetic and/or corticosteroid into the affected joint, guided by imaging. This approach is both diagnostic and therapeutic.
- Diagnostic injections help pinpoint the facet joint as the pain source.
- Therapeutic injections aim to reduce inflammation and provide pain relief.
- The procedure is minimally invasive, often performed on an outpatient basis.
Radiofrequency Ablation
Radiofrequency ablation (RFA) uses radio waves to generate heat, disabling pain-transmitting nerves from the facet joints. This method offers sustained pain relief, surpassing the temporary effects of injections.
RFA is ideal for those who have seen significant pain reduction from facet joint injections but seek a more lasting solution.
Emerging Minimally Invasive Techniques
New, minimally invasive techniques are emerging to tackle Facet Joint Syndrome. These include:
- Endoscopic procedures for direct visualization and treatment of facet joints.
- Laser or radiofrequency denervation methods.
- Minimally invasive spinal fusion for severe cases.
These innovative methods aim to deliver effective pain relief with shorter recovery times and fewer complications.

Surgical Interventions: When and Why
For those with severe Facet Joint Syndrome, surgery might be the best option. It’s usually considered when other treatments don’t work well enough.
Indications for Surgery
Surgery is needed for those with Facet Joint Syndrome who haven’t seen relief from other treatments. This includes physical therapy, medication, and injections. The main reasons are:
- Severe, debilitating pain
- Significant loss of function or mobility
- Failure of conservative treatments
Common Surgical Procedures
Several surgeries can treat Facet Joint Syndrome. These include:
- Facet joint fusion or arthrodesis, which stabilizes the joint
- Decompression surgery to relieve nerve pressure
- Minimally invasive procedures like endoscopic facet joint surgery
Recovery and Rehabilitation
Recovery from surgery for Facet Joint Syndrome involves rest and rehabilitation. This includes physical therapy to improve strength and mobility. The recovery process varies based on the surgery type.
Understanding the role of surgery helps patients and healthcare providers make better treatment choices for Facet Joint Syndrome.
When to Seek Medical Attention
Knowing when to seek medical help is key for those suspecting Facet Joint Syndrome. This condition shows through various symptoms, some needing immediate care.
Red Flag Symptoms
Some symptoms are urgent and require immediate medical attention. These include:
- Severe pain that does not improve with rest
- Loss of bladder or bowel control
- Progressive weakness or numbness in the legs
- Recent trauma or injury to the back
Seeing any of these symptoms means you should visit a healthcare provider right away.
Finding the Right Specialist
When you suspect Facet Joint Syndrome, finding the right specialist is essential. Begin with your primary care physician, who can direct you to an orthopedic surgeon or physiatrist. Make sure the specialist has a background in spinal conditions.
Reading reviews and asking for recommendations from those who’ve dealt with similar issues can also help.
Related Conditions and Comorbidities
It’s vital to grasp the related conditions and comorbidities linked to Facet Joint Syndrome for effective management. This condition often coexists with other spinal disorders, making diagnosis and treatment more complex.
Spinal Stenosis
Spinal stenosis narrows the spinal canal, putting pressure on the spinal cord and nerves. It commonly occurs with Facet Joint Syndrome, mainly in older adults. Symptoms include pain, numbness, and weakness in the back and legs.
Degenerative Disc Disease
Degenerative disc disease affects the spine, causing wear and tear of intervertebral discs. This leads to pain and reduced mobility. The degeneration of discs can also contribute to Facet Joint Syndrome by altering the spine’s biomechanics.
Spondylolisthesis
Spondylolisthesis happens when a vertebra slips forward over the one below it. It’s often linked to Facet Joint Syndrome, as the misalignment stresses the facet joints. Symptoms include lower back pain and stiffness.
Understanding these related conditions is key to creating a thorough treatment plan for patients with Facet Joint Syndrome.
Moving Forward: Living Well with Facet Joint Syndrome
Managing Facet Joint Syndrome demands a holistic strategy. It involves effective management tactics to lessen symptoms and enhance life quality. Understanding the condition and taking a proactive approach helps individuals overcome its challenges.
Effective management of Facet Joint Syndrome requires lifestyle changes, physical therapy, and sometimes, interventional procedures. Maintaining a healthy weight, regular exercise, and good posture can greatly reduce facet joint strain. For insights into surgical options like Anterior Cervical Discectomy and Fusion (ACDF), visit Acibadem Health Group’s resource on ACDF. It offers detailed information on the procedure and its advantages.
Adopting management strategies for Facet Joint Syndrome is key to regaining health control. It involves staying informed about the condition’s progression and adjusting treatment plans as needed. With the right strategy, individuals can live active and meaningful lives despite Facet Joint Syndrome’s challenges.
FAQ About Facet Joint Syndrome
Q: What is Facet Joint Syndrome?
A: Facet Joint Syndrome is a condition affecting the facet joints in the spine. It causes pain and stiffness. This happens when the joints become inflamed or irritated, often due to wear and tear, injury, or degenerative conditions.
Q: What are the symptoms of Facet Joint Syndrome?
A: Symptoms include localized pain in the neck or back, stiffness, and limited range of motion. Pain can spread to the shoulders or buttocks. It worsens with certain movements or activities.
Q: How is Facet Joint Syndrome diagnosed?
A: Diagnosis involves a physical exam, medical history, and imaging like X-rays, CT scans, or MRI. Diagnostic nerve blocks may confirm the diagnosis.
Q: What are the treatment options for Facet Joint Syndrome?
A: Treatments range from conservative methods like physical therapy and medication to interventional procedures. Facet joint injections and radiofrequency ablation are examples. In severe cases, surgery may be needed.
Q: Can Facet Joint Syndrome be prevented?
A: While some risk factors like age and genetics are unavoidable, a healthy lifestyle can reduce the risk. Regular exercise, proper posture, and a balanced diet are key.
Q: How does age affect the risk of developing Facet Joint Syndrome?
A: Age significantly increases the risk due to natural wear and tear on the facet joints. As people age, joints become less stable and more prone to inflammation and irritation.
Q: Are there any lifestyle changes that can help manage Facet Joint Syndrome?
A: Yes, maintaining a healthy weight, regular exercise, and good posture can help manage symptoms. They slow the progression of Facet Joint Syndrome.
Q: What is the role of physical therapy in treating Facet Joint Syndrome?
A: Physical therapy is vital in managing Facet Joint Syndrome. It improves flexibility, strengthens spinal muscles, and enhances spinal mobility.















