Fallopian Tubes: Anatomy and Structure of the Fallopian Tubes
The female reproductive system is a complex and highly specialized system that enables women to conceive and give birth. At the heart of this system are the Fallopian Tubes, which play a critical role in fertility and overall reproductive health. The importance of these tubes cannot be overstated. They provide the pathway for the egg to travel from the ovary to the uterus. Any issues with the Fallopian Tubes can significantly impact a woman’s ability to conceive.
Understanding the function and significance of the Fallopian Tubes is essential for maintaining reproductive health. It is also important for addressing any issues that may arise. Understanding the anatomy of the Fallopian Tubes is key to grasping their reproductive role. These tubes, also called oviducts, are muscular and vital to the female reproductive system.
Location and Physical Characteristics
The Fallopian Tubes reside in the pelvic cavity, stretching from the uterus to the ovaries. They measure about 10-12 cm in length and have a diameter ranging from 1-4 mm.
Dimensions and Segments
The Fallopian Tubes are segmented into four parts: the intramural, isthmic, ampullary, and infundibular. The intramural part is embedded in the uterine wall. The isthmic segment is narrower, connecting to the ampulla, where fertilization usually happens.
Structural Features
The Fallopian Tubes have unique features for their function. The fimbriae, which are finger-like at the tube’s end, aid in capturing the ovum released by the ovary.
Histological Composition
The Fallopian Tube’s wall is made of three layers: mucosa, muscularis, and serosa. The mucosa is lined with simple columnar epithelium.
Epithelial Lining
The epithelial lining of the Fallopian Tubes includes ciliated and non-ciliated cells. The cilia move in sync to push the ovum towards the uterus.
Muscular and Serosal Layers
The muscular layer is made of smooth muscle, aiding in ovum movement. The outermost serosal layer is a layer of connective tissue that covers the tube.
The Fallopian Tubes: Essential Components of the Female Reproductive System
The Fallopian Tubes are key to the female reproductive system. They are essential for fertilization and the early stages of embryo development.
Relationship to Other Reproductive Organs
The Fallopian Tubes are closely connected with the uterus and ovaries. This connection is vital for their function.
Connection to Uterus and Ovaries
The Fallopian Tubes link the ovaries to the uterus, acting as a pathway for the egg’s journey. This connection is critical for fertilization to happen.
The tubes are not directly attached to the ovaries but are positioned close enough to capture the released egg.
Position Within the Pelvic Cavity
In the pelvic cavity, the Fallopian Tubes are positioned laterally. They extend from the uterus towards the ovaries. Their location optimizes the capture of the ovum.
Blood Supply and Innervation
The Fallopian Tubes receive blood from the uterine and ovarian arteries. This dual blood supply is necessary for their proper functioning.
Arterial Supply
The arterial supply to the Fallopian Tubes comes from the tubal branches of both the uterine and ovarian arteries. This ensures the necessary oxygen and nutrients.
Venous Drainage and Nerve Supply
The venous drainage mirrors the arterial supply, with the tubes draining into the uterine and ovarian veins. The nerve supply comes from the autonomic nervous system.
Embryonic Development of Fallopian Tubes
The formation of Fallopian Tubes is a complex process involving precise cellular and molecular mechanisms. During embryonic development, the paramesonephric ducts give rise to the Fallopian Tubes, uterus, cervix, and upper vagina.
Formation During Fetal Development
The development of Fallopian Tubes begins around 6 weeks post-conception. The paramesonephric ducts fuse to form the uterovaginal primordium, which eventually differentiates into the various female reproductive organs. The Fallopian Tubes develop from the cranial portions of the paramesonephric ducts that remain unfused.
Developmental Abnormalities
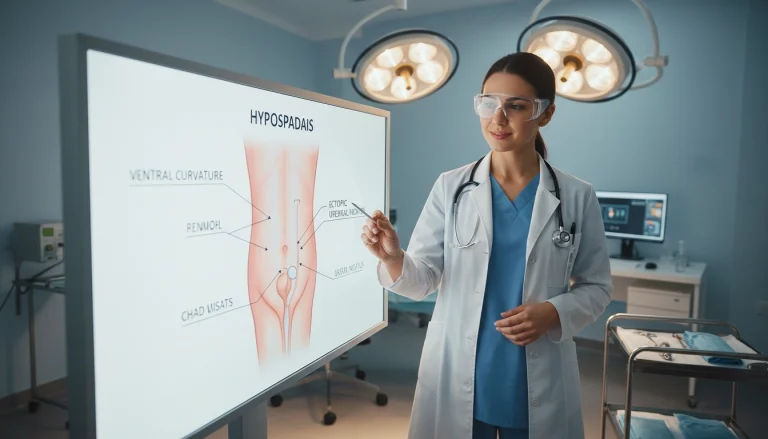
Developmental abnormalities can occur during the formation of Fallopian Tubes, leading to various congenital anomalies.
Congenital Absence
Congenital absence of Fallopian Tubes, also known as tubal agenesis, is a rare condition often associated with other reproductive tract anomalies. It can result from genetic mutations or environmental factors during fetal development.
Accessory Ostia
Accessory ostia are abnormal openings in the Fallopian Tubes, which can increase the risk of ectopic pregnancy. These anomalies occur when there is an abnormal formation of the tubal ostia during embryonic development.
Some common developmental abnormalities include:
- Tubal duplication
- Accessory tubes
- Congenital tubal occlusion
Physiological Functions
The Fallopian Tubes are essential for several key processes in human reproduction. They are not just passive conduits but actively engage in egg transport, fertilization, and early embryo development and transport.
Role in Egg Transport
The Fallopian Tubes play a vital role in capturing the ovum released from the ovary and transporting it towards the uterus. This process is facilitated by the fimbriae, finger-like projections at the end of the tubes, and the ciliary movement within the tubes.
- The fimbriae create a gentle current that guides the ovum into the tube.
- Ciliary movements and muscular contractions of the tube wall help propel the egg towards the uterus.
Fertilization Process
Fertilization typically occurs in the ampulla, the widest portion of the Fallopian Tube. The tube provides an optimal environment for sperm to meet and fertilize the egg.
- The Fallopian Tube’s secretions nourish the sperm and egg.
- The ampulla’s spacious environment allows for the fusion of sperm and egg.
Early Embryo Development and Transport
After fertilization, the zygote undergoes several divisions while being transported towards the uterus. The Fallopian Tube provides the necessary environment for early embryo development.
- The tube’s secretions support the developing embryo.
- The embryo is transported through the tube by ciliary action and peristalsis.
In summary, the physiological functions of the Fallopian Tubes are multifaceted and critical for successful reproduction. Their roles in egg transport, fertilization, and early embryo development highlight their importance in the female reproductive system.
Hormonal Influence on Fallopian Tube Function
The functioning of the Fallopian tubes is deeply connected to hormonal influences, mainly estrogen and progesterone. These hormones are key in managing various Fallopian tube functions. This includes ciliary activity, secretory function, muscular contractility, and the overall tubal environment.
Estrogen Effects
Estrogen significantly impacts the Fallopian tubes, affecting both ciliary activity and secretory function.
Ciliary Activity Regulation
Estrogen boosts ciliary beat frequency, ensuring the efficient transport of the egg through the Fallopian tubes. This is vital for fertility, as it aids in the egg’s journey to the uterus.
Secretory Function
Estrogen also controls the secretory activity of the Fallopian tube epithelium. It creates a nourishing environment for the developing embryo. The secretions provide vital nutrients and growth factors.
Progesterone Effects
Progesterone, in contrast, has specific effects on the Fallopian tubes, mainly on muscular contractility and the tubal environment.
Muscular Contractility
Progesterone influences the contractility of the Fallopian tube musculature. It affects the embryo’s movement towards the uterus. This ensures the embryo arrives on time for implantation.
Tubal Environment Modulation
Progesterone also shapes the composition of tubal secretions, creating an ideal environment for early embryonic development. The balance between estrogen and progesterone is essential for maintaining the right conditions for fertilization and early embryo development.
The interaction between estrogen and progesterone is critical for the proper functioning of the Fallopian tubes. Any imbalance can result in reproductive problems.
- Estrogen and progesterone regulate ciliary activity and secretory function.
- Progesterone modulates muscular contractility and tubal environment.
- The balance between these hormones is vital for fertility.
Common Fallopian Tube Disorders
The health of the Fallopian tubes is vital for normal reproductive function. Disorders in this area can lead to significant issues, including infertility and chronic pain. These conditions can severely impact a woman’s reproductive health.
Pelvic Inflammatory Disease (PID)
Pelvic Inflammatory Disease (PID) is a major disorder affecting the Fallopian tubes. It often results from bacterial infections. Prompt treatment is essential to prevent severe consequences.
Causative Organisms
The primary causes of PID are sexually transmitted bacteria. Neisseria gonorrhoeae and Chlamydia trachomatis are common culprits. Other bacteria from the vaginal flora can also contribute to the infection.
Progression and Complications
Untreated PID can lead to severe complications. These include chronic pelvic pain, infertility, and an increased risk of ectopic pregnancy. The infection can spread, causing further damage to the reproductive system.
Hydrosalpinx
Hydrosalpinx is characterized by fluid accumulation in the Fallopian tube. It often results from damage caused by PID or other infections. This condition can block the tube, affecting fertility.
Diagnosis of hydrosalpinx typically involves ultrasound imaging. Treatment may include surgery to restore tubal patency or, in some cases, removal of the affected tube.

Pyosalpinx and Tubo-ovarian Abscess
Pyosalpinx occurs when the Fallopian tube fills with pus due to infection. A tubo-ovarian abscess is a more severe condition where the infection spreads to involve the ovary and surrounding tissues, forming an abscess.
Both conditions are serious and require immediate medical attention. Treatment usually involves antibiotics. In severe cases, surgical drainage or removal of the affected structures may be necessary.
Common symptoms include:
- Severe pelvic pain
- Fever
- Abnormal vaginal discharge
Early diagnosis and treatment are critical to prevent long-term damage and complications.
Ectopic Pregnancy
An ectopic pregnancy occurs when a fertilized egg implants outside the uterus, usually in the fallopian tube. This condition is life-threatening. It’s important to understand its causes, risk factors, symptoms, and treatment options to manage it effectively.
Causes and Risk Factors
Factors that prevent the fertilized egg from passing through the fallopian tube can lead to ectopic pregnancy. These include previous damage or surgery to the tubes, pelvic inflammatory disease (PID), smoking, and being older.
Other risk factors include endometriosis and the use of assisted reproductive technologies. Identifying these risk factors is key to early detection and treatment.
Symptoms and Diagnosis
Symptoms of ectopic pregnancy can vary. They often include abdominal pain, vaginal bleeding, and missing periods. The severity of these symptoms can vary among individuals.
Clinical Presentation
Clinical presentation may include abdominal tenderness, adnexal mass, and signs of shock in severe cases. Healthcare providers must be alert to these signs.
Diagnostic Imaging
Diagnostic imaging, like transvaginal ultrasound, is critical in diagnosing ectopic pregnancy. It helps locate the pregnancy and assess its viability and size.
Treatment Options
The treatment for ectopic pregnancy depends on several factors. These include the size and location of the ectopic pregnancy, the patient’s health, and her desire for future fertility.
Medical Management
Medical management involves using medications like methotrexate to terminate the ectopic pregnancy. This method is used when the pregnancy is detected early and is not causing severe symptoms.
Surgical Intervention
Surgical intervention is needed when the ectopic pregnancy is advanced, causing significant symptoms, or when there’s a risk of rupture. Surgical options include salpingectomy or salpingostomy.
Ectopic pregnancy is a complex condition that requires prompt and appropriate management to prevent serious complications. It’s vital for both healthcare providers and the general public to be aware of its causes, symptoms, and treatment options.
Fallopian Tube Cancer
Fallopian tube cancer is a serious condition that demands immediate medical care. It’s a rare cancer that starts in the Fallopian tubes. These tubes are vital for the female reproductive system.
Risk Factors and Prevalence
Fallopian tube cancer is quite rare, making up a small fraction of gynecological cancers. Certain genetic mutations, like BRCA1 and BRCA2, increase the risk. Family history of ovarian or breast cancer also plays a role. Infertility or pelvic inflammatory disease might also be linked to it.
Symptoms and Diagnosis
The symptoms of Fallopian tube cancer can be vague, making it hard to diagnose. They might include abdominal pain, abnormal vaginal bleeding, and pelvic masses. Doctors use imaging like ultrasound or CT scans and tissue samples for diagnosis.
Treatment Approaches
Treatment for Fallopian tube cancer varies based on the disease’s stage and spread. It usually combines surgery, chemotherapy, and sometimes targeted therapy.
Surgical Options
Surgery is a key treatment for Fallopian tube cancer. It often involves removing the uterus, ovaries, and possibly, tumors. This approach aims to remove all cancerous tissue.
Chemotherapy Protocols
Chemotherapy is used for Fallopian tube cancer, mainly in advanced stages or after surgery. The choice of chemotherapy depends on genetic mutations present in the cancer.
Diagnostic Procedures for Fallopian Tube Assessment
Several diagnostic techniques are used to assess Fallopian tube health. These methods are essential for spotting abnormalities and grasping an individual’s reproductive health.
Hysterosalpingography (HSG)
Hysterosalpingography is a specialized imaging method. It evaluates the uterine cavity’s shape and checks the Fallopian tubes’ patency.
Procedure Technique
In an HSG procedure, a contrast agent is injected through the cervix into the uterine cavity. X-ray images are taken as the contrast material fills the uterus and moves through the Fallopian tubes.
Interpretation of Results
HSG results are based on the contrast material’s flow. If it freely flows through the tubes and spills out, the tubes are patent. Any blockages or irregular flow can signal tubal occlusion issues.
Sonohysterography and Ultrasound Evaluation
Sonohysterography combines ultrasound with saline infusion into the uterus. It visualizes the uterine cavity and checks tubal patency. This method offers insights into the uterus’s morphology and can spot abnormalities within the uterine cavity.

Laparoscopy and Falloposcopy
Laparoscopy is a surgical procedure that allows direct visualization of the pelvic organs, including the Fallopian tubes. It involves small abdominal incisions for a laparoscope, giving a clear view of the external tubal surface. Falloposcopy inserts a thin scope through the fimbriated end of the Fallopian tube to see its interior.
These diagnostic procedures are vital for evaluating Fallopian tube health and spotting issues that could affect fertility.
Surgical Procedures Involving the Fallopian Tubes
Surgical interventions targeting the Fallopian tubes are essential for managing various gynecological issues. These procedures span from sterilization methods to corrective surgeries aimed at restoring tubal function.
Tubal Ligation for Sterilization
Tubal ligation is a surgical method for female sterilization. It involves blocking or cutting the Fallopian tubes to prevent pregnancy.
Traditional Methods
Traditional tubal ligation methods include the Pomeroy technique, where a part of the tube is removed. The Irving procedure involves removing a tube segment and ligating the ends.
Modern Techniques
Modern techniques, like applying clips or rings to the tubes, offer reversible options. These methods are less invasive and can sometimes be reversed.
Tubal Reversal Procedures
Tubal reversal surgery aims to restore the Fallopian tubes’ patency after a tubal ligation. Success depends on the initial ligation method and the tube’s remaining length.
Salpingectomy and Salpingostomy
Salpingectomy involves removing a Fallopian tube, often due to ectopic pregnancy or severe damage. Salpingostomy makes an incision in the tube to remove an ectopic pregnancy while preserving the tube.
These surgical procedures showcase the range of interventions for managing Fallopian tube-related conditions. The procedure choice depends on the condition, patient’s reproductive goals, and individual factors.
Impact of Fallopian Tube Disorders on Fertility
Disorders affecting the Fallopian tubes have a significant impact on female fertility, leading to various reproductive health issues. The Fallopian tubes play a critical role in reproductive function, facilitating the transport of the egg and embryo. Damage or blockage in these tubes can lead to infertility or ectopic pregnancy.
Tubal Factor Infertility: Prevalence and Causes
Tubal factor infertility is a major cause of female infertility, accounting for a significant portion of cases. The prevalence of tubal infertility varies, often resulting from pelvic inflammatory disease, endometriosis, or previous tubal surgery.
Proximal Tubal Blockage
Proximal tubal blockage occurs when there is an obstruction at the uterine end of the Fallopian tube. This condition can result from tubal spasm, mucus plugs, or more severe conditions like salpingitis isthmica nodosa.
Distal Tubal Damage
Distal tubal damage involves the fimbrial end of the tube and is often associated with hydrosalpinx or tubal ectopic pregnancy. The damage can lead to impaired ovum pickup and fertilization.
Diagnostic Evaluation of Tubal Infertility
The diagnostic evaluation of tubal infertility involves several methods, including hysterosalpingography (HSG), sonohysterography, and laparoscopy. HSG is a primary diagnostic tool that provides detailed images of the uterine cavity and Fallopian tubes.
These diagnostic approaches help identify the site and extent of tubal damage, guiding appropriate treatment strategies for tubal infertility.
Assisted Reproductive Technologies for Fallopian Tube Issues
Assisted reproductive technologies have transformed the treatment of Fallopian tube-related infertility. They offer effective solutions for those facing challenges due to damaged or blocked tubes.
In Vitro Fertilization (IVF) Procedures
In vitro fertilization is a key assisted reproductive technology for addressing Fallopian tube issues. It involves fertilizing an egg with sperm outside the body. Then, the embryo is transferred to the uterus.
Candidate Selection
Those with severe Fallopian tube damage or blockage, or those who have failed other fertility treatments, are often candidates for IVF. A detailed evaluation is necessary to determine if IVF is suitable.
Success Rates
IVF success rates depend on several factors, including age, egg quality, and the clinic’s expertise. Generally, women under 35 have higher success rates with IVF.
Tubal Surgery vs. IVF: Comparative Outcomes
When deciding on treatment for Fallopian tube-related infertility, tubal surgery and IVF are both options. Tubal surgery aims to repair or unblock the tubes. IVF, on the other hand, bypasses the tubes entirely.
The choice between tubal surgery and IVF depends on various factors. These include the extent of tubal damage, the patient’s age, and other fertility factors. Seeking advice from a fertility specialist is essential in choosing the best treatment plan.
Preventive Measures for Fallopian Tube Health
Ensuring the health and function of the Fallopian tubes is critical. Adopting certain practices and being proactive about reproductive health can significantly lower the risk of disorders. This proactive approach is key to maintaining their integrity.
Infection Prevention Strategies
Infections pose a significant risk to Fallopian tube health. It’s essential to implement strategies to prevent infections. This is a fundamental step in safeguarding these vital structures.
Safe Sexual Practices
Practicing safe sex is vital. Using condoms and limiting sexual partners can help prevent sexually transmitted infections (STIs). These infections are a common cause of Fallopian tube damage.
Prompt Treatment of Infections
Timely treatment of infections, including STIs, is critical. Early diagnosis and treatment can prevent severe complications like pelvic inflammatory disease (PID). PID can severely damage the Fallopian tubes.
Regular Gynecological Check-ups and Screening
Regular gynecological check-ups and screenings are essential for Fallopian tube health. These visits enable early detection of issues like infections or abnormalities. This ensures timely intervention and care.
Combining infection prevention strategies with regular gynecological care is a proactive approach. It helps protect Fallopian tube health and overall reproductive well-being. This dual strategy is vital for maintaining optimal health.
Current Research and Future Directions in Fallopian Tube Medicine
Recent advancements in medical technology have greatly enhanced our grasp of Fallopian Tube medicine. Current studies aim to create new diagnostic and therapeutic methods for addressing Fallopian Tube-related issues.
Research is underway to explore artificial intelligence’s role in detecting tubal damage and predicting the success of fertility treatments. The future of Fallopian Tube medicine might include the development of less invasive surgical methods and tailored treatment plans.
Scientists are also delving into the genetic aspects of Fallopian Tube disorders. This could pave the way for targeted therapies. The integration of ongoing research and future advancements in Fallopian Tube medicine is expected to significantly improve patient outcomes and fertility treatments.
FAQ About Fallopian Tubes
Q: What is the primary function of the Fallopian Tubes in the female reproductive system?
A: The Fallopian Tubes’ main role is to move the egg from the ovary to the uterus. This allows fertilization to take place.
Q: What are the different segments of the Fallopian Tubes?
A: The Fallopian Tubes are segmented into four parts: the interstitial, isthmic, ampullary, and infundibular regions.
Q: How do hormonal changes affect the Fallopian Tubes?
A: Hormones like estrogen and progesterone impact the Fallopian Tubes. They affect ciliary activity, secretory functions, and muscle contractions.
Q: What is the most common cause of Fallopian Tube damage?
A: Pelvic inflammatory disease (PID) is a major cause of Fallopian Tube damage. It often stems from bacterial infections like chlamydia and gonorrhea.
Q: How is Fallopian Tube damage diagnosed?
A: To diagnose Fallopian Tube damage, tests like hysterosalpingography (HSG), sonohysterography, and laparoscopy are used.
Q: What are the treatment options for ectopic pregnancy?
A: Ectopic pregnancy treatment includes medical management with methotrexate and surgical options like salpingectomy or salpingostomy.
Q: Can Fallopian Tube cancer be prevented?
A: Preventing Fallopian Tube cancer is challenging. Yet, regular gynecological exams and screenings can help catch it early.
Q: What is the success rate of tubal reversal procedures?
A: Tubal reversal success rates vary. They depend on age, sterilization method, and tube length.
Q: How do assisted reproductive technologies (ART) help women with Fallopian Tube issues?
A: ART, like IVF, aids women with Fallopian Tube problems. It bypasses the damaged tubes to help conceive.
Q: What are some preventive measures for maintaining Fallopian Tube health?
A: To keep Fallopian Tubes healthy, practice safe sex, treat infections promptly, and visit your gynecologist regularly.