Food Allergies in Children: What Are Food Allergies in Children
As a parent or caregiver, it’s vital to grasp the dangers of certain foods for kids’ health and safety. Adverse reactions can vary from mild discomfort to severe, life-threatening conditions. It’s critical to know the causes, symptoms, and ways to manage these allergies. This knowledge empowers parents and caregivers to protect their children’s well-being.
Delving into the details of this condition helps us better understand how to spot and manage it. This approach can significantly lower the risks it poses. Food allergies in children are a growing concern, affecting their quality of life. It’s vital for parents and caregivers to understand the facts. Food allergies are a serious health issue, different from food intolerance. Knowing the difference and their prevalence is key to managing them effectively.
The Immune System Response
Food allergies happen when the immune system sees a food as harmful and reacts against it. This reaction releases chemicals like histamine, causing symptoms from mild to severe. The immune system’s goal is to protect, but in allergies, this response is misguided, leading to health problems.
Food Allergy vs. Food Intolerance
Distinguishing between food allergies and intolerance is critical. Both involve adverse reactions to food, but they’re different. Food intolerance affects digestion, causing symptoms like bloating, without immune system involvement. Food allergies, on the other hand, are immune reactions that can be life-threatening.
Prevalence Among American Children
Food allergies in children are a major concern in the U.S. Data shows about 8% of children have a food allergy, with some being more common. The rise in food allergies over the years emphasizes the need for awareness and effective management.
Common Food Allergens in Children
Identifying the most common food allergens in children is essential for managing and potentially preventing allergic reactions. Food allergies are prevalent among children in the United States. Certain foods are more likely to trigger allergic reactions.
The “Big Eight” Food Allergens
The “Big Eight” food allergens are responsible for the majority of food allergy reactions in children. These include:
- Milk
- Eggs
- Fish
- Crustacean shellfish
- Tree nuts
- Peanuts
- Wheat
- Soy
These foods are considered high-risk for causing allergic reactions. They are often the focus of allergy testing and management plans.
Age-Related Patterns in Food Allergies
Food allergies can manifest at different ages, with some allergens being more prevalent at certain stages of childhood. For instance, milk and egg allergies are more common in infants and young children. Allergies to peanuts, tree nuts, and fish often persist into later childhood and adulthood.
Emerging Allergens in the American Diet
As dietary habits evolve, new and emerging allergens are being identified. Foods such as sesame, certain types of fruit, and other non-traditional allergens are becoming more recognized as causes of allergic reactions in children.
Understanding these emerging allergens is critical for effective allergy management. It is also important for staying updated with the latest research and guidelines.
The Science Behind Food Allergies
Exploring the science of food allergies uncovers the complex processes behind allergic reactions. These reactions involve multiple parts of the immune system. Grasping these mechanisms is key to creating effective treatments.
IgE-Mediated vs. Non-IgE-Mediated Reactions
Food allergies fall into two main categories: IgE-mediated and non-IgE-mediated. IgE-mediated reactions are the most prevalent, triggered by Immunoglobulin E (IgE) antibodies. Symptoms appear almost instantly after exposure to the allergen.
Non-IgE-mediated reactions, by contrast, are slower to develop and involve different immune system components. They often manifest as gastrointestinal issues or skin rashes. Here are some key differences between IgE-mediated and non-IgE-mediated reactions:
- IgE-mediated reactions are immediate, while non-IgE-mediated reactions are delayed.
- IgE-mediated reactions involve IgE antibodies, whereas non-IgE-mediated reactions involve other immune cells.
- Symptoms of IgE-mediated reactions can include anaphylaxis, while non-IgE-mediated reactions typically cause gastrointestinal or skin symptoms.
The Allergic Cascade
The allergic cascade is the sequence of events when the immune system reacts to an allergen. It involves the activation of immune cells, the release of chemical mediators, and the appearance of allergic symptoms. Even small amounts of an allergen can trigger this cascade.
Cellular Mechanisms
Cellular mechanisms are vital in the development of food allergies. Immune cells like T cells and mast cells are central to the allergic response. Understanding their interaction and role in the reaction is essential for developing targeted therapies.
The key cellular mechanisms include:
- The activation of T cells, which coordinate the immune response.
- The release of histamine and other chemical mediators from mast cells, leading to allergic symptoms.
- The production of IgE antibodies by B cells, which are central to IgE-mediated reactions.
Recognizing Food Allergy Symptoms
Food allergies in children can manifest in various ways, from mild discomfort to severe reactions. It’s vital to recognize these symptoms early to manage the allergy effectively.
Mild to Moderate Symptoms
Mild to moderate symptoms include skin rashes, itching, swelling, stomach cramps, diarrhea, and vomiting. These reactions often occur within minutes to hours after exposure to the allergen. Children may also show behavioral changes or irritability.
Severe Symptoms and Anaphylaxis
Severe reactions can lead to anaphylaxis, a potentially life-threatening condition. Symptoms include difficulty breathing, rapid heartbeat, dizziness, confusion, and a drop in blood pressure. Anaphylaxis can cause airway constriction, leading to asphyxiation if not treated quickly.
Delayed Reactions
Some reactions can be delayed, making diagnosis harder. These delayed reactions may appear several hours after ingestion and can manifest as gastrointestinal symptoms or eczema flare-ups. A food diary can help identify allergens in such cases.
When to Seek Emergency Care
If a child shows signs of anaphylaxis or severe reaction, immediate emergency care is necessary. Administering epinephrine via an EpiPen or other auto-injector is the first step. Call emergency services right away, as anaphylaxis can be fatal without prompt treatment.
Understanding the spectrum of food allergy symptoms and knowing when to seek help is critical for the safety and well-being of children with food allergies.
Risk Factors for Developing Food Allergies
Children’s susceptibility to food allergies stems from a mix of genetic, environmental, and lifestyle elements. Recognizing these factors empowers parents and caregivers to take preventive measures. This could potentially lower the risk of their child developing a food allergy.
Genetic Predisposition
Children with a family history of allergies are more likely to develop food allergies. If one or both parents have an allergy, their child’s risk increases significantly.
Environmental Factors
Environmental factors, such as early exposure to certain foods and the gut microbiome, are critical in allergy development. The way a child is introduced to foods and their environment can shape their immune system’s response.
The Hygiene Hypothesis
The hygiene hypothesis posits that a lack of early exposure to certain microorganisms may increase allergy risk. It suggests that a moderate level of microbial exposure is essential for a robust immune system.
Early Life Exposures
Early life exposures, like breastfeeding and the timing of solid food introduction, are linked to food allergy development. Studies indicate that introducing certain foods early may lower allergy risk to those foods.
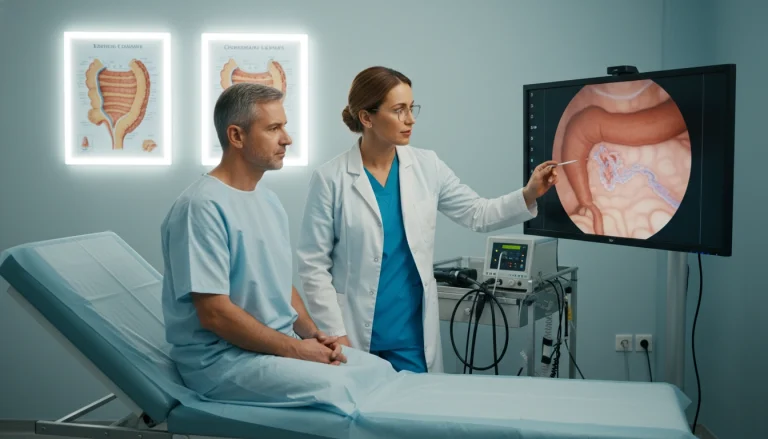
Diagnosing Food Allergies in Children
Diagnosing food allergies in children requires a detailed approach. It involves reviewing medical history, conducting physical exams, and using various diagnostic tools. Accurate diagnosis is key for effective management and treatment.
Medical History and Physical Examination
Understanding a child’s medical history is vital in diagnosing food allergies. Healthcare providers collect information on symptoms, reaction timing, and any dietary or environmental changes. A physical exam helps spot signs of allergic reactions or other conditions that might be causing symptoms.
Skin Prick Tests
Skin prick tests are a common tool for diagnosing allergies. A small amount of the suspected allergen is applied to the skin, and a lancet pricks it. The skin is then watched for signs of an allergic reaction, like redness, swelling, or itching.
Blood Tests for Specific IgE
Blood tests measure specific IgE antibodies, which indicate an allergic reaction. These tests can pinpoint the specific allergens causing the reaction.
Oral Food Challenges
Oral food challenges involve the child eating small amounts of the suspected allergenic food under medical supervision. This test is considered the most reliable method for diagnosing food allergies.
Elimination Diets
Elimination diets remove suspected allergenic foods from the child’s diet for 2-4 weeks. If symptoms improve, foods are reintroduced one at a time to monitor for reactions.
The diagnostic process for food allergies in children combines these methods. Healthcare providers use medical history, physical exams, and diagnostic tests to determine the presence and severity of a food allergy.
- Medical history and physical examination provide initial clues.
- Skin prick tests and blood tests help identify specific allergens.
- Oral food challenges and elimination diets confirm the diagnosis.
Food Allergies in Children: Infants and Toddlers
Infants and toddlers are highly susceptible to food allergies, making early detection and management critical. Food allergies occur when the immune system overreacts to a specific food. In young children, this can lead to various symptoms.
Early Signs and Symptoms
It’s vital to recognize the early signs and symptoms of food allergies in infants. Common indicators include skin rashes, digestive issues, and severe reactions like anaphylaxis. Parents should watch for any changes in their child’s behavior or physical state after feeding.
Some infants may show mild symptoms, while others may experience severe reactions. It’s essential for parents to collaborate with their pediatrician to identify any possible allergies.
Breastfeeding Considerations
Breastfeeding is recommended for infants, including those at risk of food allergies. Mothers with a family history of allergies may need to adjust their diet. Foods consumed by the mother can pass through breast milk and potentially cause an allergic reaction in the infant.
Introduction of Solid Foods
The introduction of solid foods is a critical period for infants. Recent guidelines suggest introducing foods like peanuts early to reduce allergy risk. Parents should consult with their pediatrician to develop a safe plan for introducing new foods.
Formula Options for Allergic Infants
For infants not breastfed or weaned off breast milk, choosing the right formula is essential. For those with cow’s milk allergy, hypoallergenic formulas are available. These formulas have proteins broken down into smaller pieces, reducing the risk of allergic reactions.
- Extensively hydrolyzed formulas (e.g., Nutramigen)
- Amino acid-based formulas (e.g., Neocate)
- Partially hydrolyzed formulas (used for prevention in some cases)
Managing Food Allergies in Children
Understanding and managing food allergies in children is vital. It involves being prepared for emergencies and ensuring proper nutrition despite dietary restrictions. Effective management requires a combination of strategies to minimize allergic reactions and promote overall well-being.
Creating an Allergy Action Plan
An allergy action plan is essential. It outlines steps for allergic reactions. It includes the child’s medical history, known allergens, and symptoms of an allergic reaction. It also details the appropriate treatment, including epinephrine use with an EpiPen.
Parents must collaborate with healthcare providers to create this plan. It should be tailored to the child’s specific needs. Sharing the plan with caregivers, teachers, and others is also critical.
Emergency Medication and EpiPen Use
Emergency medication, like epinephrine auto-injectors, is vital for severe allergic reactions. Parents need to understand how to administer epinephrine. They should recognize signs that indicate its use, such as difficulty breathing or rapid heartbeat.
Nutritional Considerations
Ensuring a balanced diet is key despite avoiding certain foods. Common allergens like milk, eggs, nuts, and wheat are also nutrient-rich. This can make it challenging to provide a well-rounded diet.
Finding Safe Substitutes
Finding safe substitutes for allergenic foods is essential. For example, children allergic to milk can have calcium-fortified non-dairy milk. Those allergic to nuts can try sunflower seed butter instead of peanut butter.
Reading food labels carefully is critical to avoid allergens and cross-contamination risks. Consulting with a registered dietitian or healthcare provider can offer valuable guidance on managing the child’s diet.
Treatment Options for Food Allergies
Food allergy treatment has seen significant advancements, providing various strategies for management. Despite the lack of a cure, these options can greatly reduce risks and enhance life quality for those affected.
Strict Avoidance Strategies
At the heart of managing food allergies is strict avoidance of the allergenic food. This requires diligent label reading, asking about food preparation when dining out, and educating others about the allergy. It’s essential to involve family, caregivers, and school staff in this awareness.
Oral Immunotherapy (OIT)
Oral Immunotherapy is a promising method that gradually increases exposure to the allergenic food to build tolerance. While it has shown promise in reducing allergic reaction severity, it carries risks. It necessitates close medical monitoring.
Sublingual Immunotherapy (SLIT)
Sublingual Immunotherapy involves placing a small amount of the allergen under the tongue. This method is being explored for its ability to desensitize individuals to specific allergens. Its effectiveness varies, and further research is required.
Emerging Treatments and Clinical Trials
Ongoing research into food allergy treatments is yielding promising results, with several emerging therapies in clinical trials. These include innovative immunotherapy forms and other groundbreaking approaches. They offer hope for managing and potentially curing food allergies in the future.
Preventing Food Allergies
With the rise in food allergies, understanding prevention is key. Recent studies aim to find ways to lower allergy risk. This is vital for public health.
Current Guidelines for Allergen Introduction
Experts now suggest introducing allergens early in a child’s diet. This method is backed by research. It shows early exposure can lower allergy risk.
The LEAP Study and Early Peanut Introduction
The LEAP study found introducing peanuts early in infancy cuts peanut allergy risk. This study has shaped guidelines for other allergens too.
Maternal Diet During Pregnancy and Breastfeeding
Maternal diet during pregnancy and breastfeeding might prevent food allergies. Some studies indicate that eating allergens during these times can shape the infant’s immune system.
The Role of Gut Microbiome
The gut microbiome is essential for immune system development. Ongoing research explores its role in food allergy prevention. For insights on diet and health, visit Acibadem International.

Navigating School with Food Allergies
Ensuring the safety of children with food allergies in schools demands a multi-faceted approach. This includes policy development, education, and preparedness. As a parent, navigating the school environment to protect your child can seem daunting. Yet, with the right strategy, it’s fully attainable.
School Policies and 504 Plans
Understanding and implementing school policies is essential for managing food allergies effectively. A critical component is the 504 Plan. This legally binding document outlines the accommodations your child will receive to ensure their safety.
- Meet with school administrators to discuss your child’s needs.
- Develop a clear plan for emergency situations.
- Ensure that all relevant staff members are aware of your child’s condition and the plan in place.
Educating Teachers and Staff
Educating teachers and staff about food allergies is vital. They need to understand the signs of an allergic reaction, know how to administer epinephrine using an EpiPen, and be aware of your child’s specific allergy plan.
Handling School Lunches and Special Events
Managing school lunches and special events requires careful planning. Parents should collaborate with the school cafeteria to identify safe meal options. They must also ensure that staff are aware of possible allergens.
- Review school menus in advance.
- Pack safe lunches or snacks when necessary.
- Communicate with teachers about special events or celebrations that may involve food.
Preparing Your Child to Self-Advocate
As your child grows, it’s essential to teach them how to self-advocate. This includes understanding their allergy, recognizing symptoms, and knowing how to ask for help.
By empowering your child with the knowledge and skills to manage their food allergy, you’re helping them navigate the school environment with confidence.
The Psychological Impact of Food Allergies
Food allergies pose not just physical risks but also have a significant psychological impact on children and their families. The need for constant vigilance to manage these allergies can increase stress levels. This affects overall well-being.
Anxiety and Quality of Life
Children with food allergies often feel heightened anxiety due to the fear of accidental exposure and severe reactions. This anxiety can significantly impact their quality of life. It affects their daily activities and social interactions.
Families also face strain, needing to be constantly prepared for emergencies and navigating complex social situations. This includes school events or dining out.
Social Challenges for Children
Food allergies can lead to social challenges for children, including feelings of isolation or being different from their peers. They may struggle with participating in activities involving food, such as birthday parties or school lunches.
Supporting Your Child’s Emotional Health
Supporting a child’s emotional health is critical. Open communication about their allergies and feelings is key. Encouraging normalcy and participation in safe activities can boost their confidence and sense of inclusion.
Family Dynamics and Sibling Considerations
Food allergies can affect family dynamics, with siblings sometimes feeling neglected or responsible for their allergic brother or sister. It’s vital to address these feelings and ensure all children feel supported and understood.
By fostering a supportive environment and educating family members about food allergies, families can mitigate some of the psychological impacts. This promotes a healthier, more balanced family life.
Cross-Reactivity and Oral Allergy Syndrome
Understanding cross-reactivity is key to managing food allergies. It can lead to unexpected reactions to foods that seem unrelated. This happens when the immune system mistakenly identifies similar proteins in different substances, causing an allergic response.
Understanding Cross-Reactive Foods
Cross-reactive foods have similar protein structures. This similarity causes the immune system to react to them in a similar way. For example, those allergic to birch pollen may experience oral allergy syndrome (OAS) when eating apples or carrots due to cross-reactivity.
Common Cross-Reactivity Patterns
There are common patterns in cross-reactivity. For instance, individuals with a ragweed allergy may react to melons or bananas. This is because certain tree pollens and specific fruits or vegetables share similar protein structures.
Managing Oral Allergy Syndrome
Managing OAS requires avoiding cross-reactive foods during peak pollen seasons. It’s also important to be aware of the foods most likely to cause a reaction. Cooking or processing foods can sometimes reduce their allergenicity.
Reading Food Labels and Avoiding Hidden Allergens
For families with food allergies, reading food labels is a daily task. It’s essential to know what’s in the food you buy to avoid dangerous allergens.
Understanding FDA Labeling Laws
The FDA mandates that food labels list the top eight allergens. These include milk, eggs, fish, shellfish, tree nuts, peanuts, wheat, and soybeans. Labels must clearly state the presence of these allergens in simple terms.
Precautionary Allergen Labeling
Precautionary labels, like “may contain,” are not FDA-regulated. They indicate a possible presence of an allergen but do not guarantee it. Consumers need to be cautious, as these labels suggest a risk, not a certainty.
Hidden Sources of Common Allergens
Allergens can be found in unexpected foods. For instance, peanuts might be in sauces or spice blends. Knowing these hidden sources is vital to avoid exposure.
Dining Out Safely with Food Allergies
When dining out, tell your server about your food allergy. Inquire about ingredients and how they are prepared. Some restaurants have specific protocols for handling food allergies, so it’s worth asking.
By being vigilant and informed, individuals with food allergies can significantly reduce their risk of exposure to allergens. Always read labels carefully and ask questions when eating out.
Outgrowing Food Allergies in Children
Children with food allergies often wonder if they’ll always have to avoid certain foods. The chance of outgrowing a food allergy is complex. It depends on several factors, including the allergy type and the child’s condition.
Which Allergies Are Commonly Outgrown
Some food allergies are more likely to be outgrown than others. For example, allergies to milk, eggs, wheat, and soy often fade during childhood. On the other hand, allergies to peanuts, tree nuts, fish, and shellfish tend to persist.
Factors Affecting Resolution
The likelihood of outgrowing a food allergy varies. It depends on the allergy’s severity, the presence of other allergies or conditions like asthma, and specific IgE antibody levels. Children with lower specific IgE antibody levels are more likely to outgrow their allergy.
Periodic Re-Testing and Food Challenges
Regular re-testing is key to see if a child has outgrown their food allergy. This might involve blood tests or supervised oral food challenges. An oral food challenge is the most reliable method for diagnosing food allergies and determining if an allergy has been outgrown.
Moving Forward: Hope and Research for Food Allergic Families
Families dealing with food allergies can find solace in the quick progress in Food Allergy Research. New treatments are emerging, bringing hope for better management and even a cure for these allergies.
The medical field is advancing rapidly in grasping the intricacies of food allergies. This has led to the development of innovative treatments. Oral Immunotherapy (OIT) and Sublingual Immunotherapy (SLIT) are among the promising methods being studied. They aim to make individuals less reactive to certain allergens.
There is a growing sense of hope for families as research continues to advance. The dedication of scientists, healthcare professionals, and advocacy groups is driving this progress. As we learn more about food allergies, we can look forward to more effective treatments and possibly life-changing solutions.
Despite the challenges ahead, the progress made so far is a beacon of hope. By keeping up with the latest in Food Allergy Research, families can face their challenges with renewed confidence and hope for the future.
FAQ
Q: What are the most common food allergens in children?
A: In children, the most prevalent food allergens include peanuts, tree nuts, milk, eggs, fish, shellfish, wheat, and soy. These are commonly known as the “Big Eight” food allergens.
Q: How are food allergies diagnosed in children?
A: Diagnosing food allergies in children involves a thorough medical history and physical exam. It also includes skin prick tests, blood tests for specific IgE, oral food challenges, and elimination diets.
Q: What is the difference between a food allergy and food intolerance?
A: A food allergy is an immune reaction to a specific food. In contrast, food intolerance is a non-allergic reaction, often related to digestion or other factors.
Q: Can food allergies be outgrown?
A: Yes, some children outgrow their food allergies, like milk and egg allergies. Yet, allergies to peanuts, tree nuts, fish, and shellfish tend to persist.
Q: How can I manage my child’s food allergy at school?
A: Managing your child’s food allergy at school requires collaboration with teachers and staff. Develop a 504 plan, educate them about the allergy, and ensure they know how to administer emergency medication.
Q: What is oral immunotherapy (OIT) and is it effective?
A: Oral immunotherapy (OIT) involves gradually increasing exposure to an allergenic food to build tolerance. It shows promise but effectiveness varies. It must be done under medical supervision.
Q: How can I prevent my child from developing a food allergy?
A: Introducing allergenic foods, like peanuts, early in a child’s life may reduce allergy risk. Breastfeeding and a balanced diet also play roles in prevention.
Q: What are the signs and symptoms of anaphylaxis?
A: Anaphylaxis is a severe, life-threatening allergic reaction. Symptoms include difficulty breathing, rapid heartbeat, dizziness, confusion, and a drop in blood pressure. Immediate medical attention is required.
Q: How do I read food labels to avoid allergens?
A: To avoid allergens, carefully read food labels. Look for the “Big Eight” allergens and any precautionary labeling, such as “may contain” or “processed in a facility with.”
Q: Can food allergies affect a child’s emotional well-being?
A: Yes, food allergies can affect a child’s emotional well-being, causing anxiety, stress, and social challenges. Supporting their emotional health through open communication and education is vital.