Gastric Bypass: What is Gastric Bypass Surgery?
For those battling obesity, weight loss surgery can be a transformative choice. The Gastric Bypass procedure stands out as a highly effective option. This surgery creates a small stomach pouch and reconfigures the digestive tract. It aids in substantial weight loss. By shrinking the stomach, patients consume less, feel satiated quicker, and see enhancements in health linked to obesity.
The advantages of this surgery go beyond mere weight reduction. It boosts overall health and enhances life quality. This makes Gastric Bypass a favored option for those aiming for a lasting obesity solution. Gastric Bypass surgery is a vital treatment for severe obesity and related health problems. It changes the digestive system to help with significant weight loss.
Definition and Basic Procedure
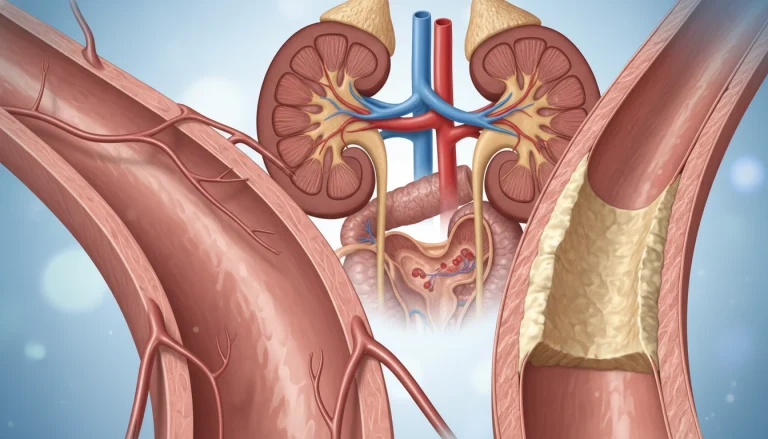
Gastric Bypass surgery, or Roux-en-Y Gastric Bypass, is a complex operation. It creates a small stomach pouch and reroutes the intestine. The surgery has two parts: a restrictive element that limits food intake and a malabsorptive element that reduces nutrient absorption.
The surgery is often done laparoscopically, using small incisions and a camera. This method leads to fewer complications and a quicker recovery compared to open surgery.
History and Development
The idea of Gastric Bypass surgery started in the 1950s as a weight loss method. Over time, the technique has improved greatly. Advances in technology and understanding obesity as a metabolic disorder have played key roles.
The introduction of laparoscopic techniques in the 1990s made Gastric Bypass surgery more appealing. It became known for its minimally invasive nature and shorter recovery time. Today, it’s seen as one of the most effective weight loss surgeries, leading to substantial weight loss and health improvements.
How Gastric Bypass Works
Gastric Bypass surgery works through a dual mechanism. It restricts food intake and alters nutrient absorption. This combination is key to its effectiveness in achieving significant weight loss.
The Restrictive Component
The restrictive component of Gastric Bypass surgery involves creating a small stomach pouch. This pouch significantly reduces the amount of food that can be consumed at one time. Patients feel full sooner, reducing overall calorie consumption.
By restricting the volume of food, the Gastric Bypass procedure aids in weight loss. It reduces the total caloric intake.
The Malabsorptive Component
The malabsorptive component involves rerouting a portion of the small intestine. This reduces the body’s ability to absorb nutrients from the food consumed. Even when more food is eaten, the body absorbs fewer calories.
The combination of reduced food intake and decreased nutrient absorption facilitates substantial weight loss. This is in patients who undergo Gastric Bypass surgery.
Types of Gastric Bypass Procedures
There are various gastric bypass procedures, each with its own set of benefits and considerations. The choice of procedure hinges on several factors. These include the patient’s health, body mass index (BMI), and past surgical history.
Roux-en-Y Gastric Bypass
The Roux-en-Y gastric bypass is the most frequently performed gastric bypass surgery. It involves creating a small pouch from the stomach. This pouch is then connected directly to the small intestine.
Standard Technique
The standard Roux-en-Y technique divides the stomach into a small upper pouch and a larger lower portion. The small intestine is rearranged to connect to the new stomach pouch.
Variations
Variations of the Roux-en-Y procedure include adjustments in the length of the intestinal limbs. These adjustments can affect the degree of malabsorption and weight loss.
Mini Gastric Bypass
The mini gastric bypass is a simpler version of the Roux-en-Y. It involves a single connection between the stomach and the small intestine. It’s less invasive but may have different outcomes.
Other Variations
Other variations include the single-anastomosis gastric bypass and the banded gastric bypass. Each has its advantages and possible complications. The choice depends on individual patient factors.
Understanding the different types of gastric bypass procedures is essential for patients. It helps them make informed decisions about their weight loss surgery.
Benefits of Gastric Bypass
Gastric bypass surgery offers more than just weight loss. It positively impacts various health and wellbeing aspects. This surgery has shown to be beneficial for many.
Weight Loss Outcomes
Gastric bypass surgery results in significant weight loss for obese individuals. Studies indicate that patients can lose a substantial percentage of excess body weight within the first year post-surgery.
Resolution of Obesity-Related Conditions
The surgery also improves or resolves obesity-related health conditions. This includes better management of Type 2 diabetes and cardiovascular disease.
Type 2 Diabetes Improvement
Type 2 diabetes, often linked with obesity, sees improvement with gastric bypass surgery. It can even lead to remission in some cases.
Cardiovascular Benefits
Cardiovascular health also benefits from gastric bypass surgery. Patients often see a decrease in blood pressure and improvements in lipid profiles.
Psychological and Quality of Life Improvements
Beyond physical health, gastric bypass surgery enhances psychological wellbeing and quality of life. Patients often report increased self-esteem and better social and physical activity participation.

Risks and Possible Complications
It’s vital for those thinking about Gastric Bypass surgery to understand the risks and complications. This procedure can lead to significant weight loss. Yet, it’s important to know about the possible negative effects.
Short-Term Surgical Risks
Gastric Bypass surgery, like any major surgery, comes with immediate risks. These include infection, bleeding, and reactions to anesthesia. These risks are managed with proper medical care.
- Infection at the surgical site
- Bleeding or hemorrhage
- Adverse reactions to anesthesia
- Respiratory complications
Long-Term Complications
Long-term issues can include bowel obstruction, hernias, and internal bleeding. Regular check-ups with healthcare providers can help catch and manage these problems early.
- Bowel obstruction
- Hernias
- Internal bleeding
- Gastrointestinal issues
Nutritional Deficiencies
Nutritional deficiencies are a major concern after Gastric Bypass surgery. This is because the digestive system changes.
Common Vitamin Deficiencies
Patients often face deficiencies in vitamins like B12 and D. Supplements are usually needed.
Mineral Deficiencies
Minerals like iron and calcium can also be lacking. Regular monitoring and supplements can help prevent these deficiencies.
Ideal Candidates for Gastric Bypass
Identifying the perfect candidate for Gastric Bypass surgery requires a thorough evaluation. This surgery is a major decision, necessitating a deep look into a patient’s health and suitability. It’s a step that demands careful thought.
BMI Requirements
The Body Mass Index (BMI) is a key factor in determining candidacy. Typically, those with a BMI of 40 or higher are considered. Or, a BMI of 35 or higher with obesity-related health issues also qualify. For more insights on common misconceptions about bariatric surgery, visit this resource.
Health Conditions
Certain health conditions can also qualify a patient. These include type 2 diabetes, high blood pressure, and sleep apnea. The evaluation process examines how these conditions might affect the surgery and recovery.
Psychological Readiness
Psychological readiness is essential for Gastric Bypass surgery. Candidates must show they understand the lifestyle changes needed after surgery.
Previous Weight Loss Attempts
Previous weight loss efforts are also considered. Candidates usually have a history of unsuccessful weight loss through diet and exercise alone.
Key factors for the ideal candidate include:
- High BMI with or without related health conditions
- Presence of obesity-related health issues
- Psychological stability and readiness for lifestyle changes
- History of failed weight loss attempts
The Gastric Bypass Evaluation Process
The evaluation for Gastric Bypass surgery is detailed, covering medical, psychological, and nutritional aspects. It aims to confirm if a candidate is right for the procedure.
Medical Assessment
A detailed medical check-up is conducted. It looks at the patient’s overall health and identifies any risks.
Required Tests and Screenings
Patients must undergo several tests. These include blood work, imaging, and cardiac evaluations. They help assess the patient’s health status.
Specialist Consultations
Consultations with specialists like cardiologists and pulmonologists are necessary. They evaluate and manage any existing health conditions.
Psychological Evaluation
A psychological evaluation assesses the patient’s mental readiness for surgery. It also checks their ability to adapt to lifestyle changes post-surgery.
Nutritional Counseling
Nutritional counseling is provided. It teaches patients about dietary changes post-surgery. This ensures they get the right nutrition and achieve weight loss.
The thorough evaluation process prepares patients for Gastric Bypass surgery. It also readies them for the lifestyle adjustments that come with it.
Preparing for Gastric Bypass Surgery
Gastric bypass surgery demands careful preparation for a successful outcome. As the surgery date nears, patients must adjust their diet, lifestyle, and medical care. This ensures a smooth transition into the post-surgical phase.
Pre-Surgery Diet
A pre-surgery diet is essential for reducing liver size and body fat. This makes the surgery easier. Patients are usually advised to follow a very low-calorie diet for 1-2 weeks before the surgery. This diet minimizes surgical risks and complications.

Lifestyle Changes
Lifestyle adjustments are key to the success of gastric bypass surgery. Patients are urged to quit smoking, avoid alcohol, and start a gentle exercise routine. These steps improve overall health and lower the risk of complications after surgery.
Medical Preparations
Medical preparations include various tests and evaluations to confirm the patient’s fitness for surgery. This includes blood tests, imaging studies, and a detailed review of the patient’s medical history. Patients are also instructed to adjust their medications as advised by their healthcare provider.
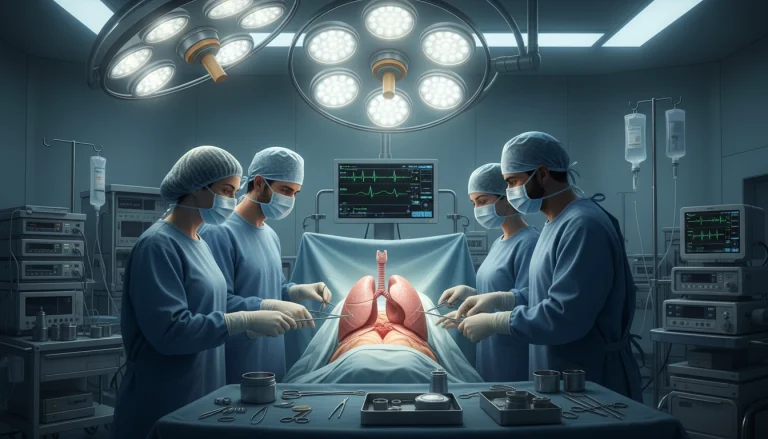
Gastric Bypass Surgery
Gastric Bypass Surgery is a complex procedure aimed at weight loss. It’s for those who haven’t lost weight through other methods. The surgery involves several steps to reshape the stomach and intestines.
Laparoscopic vs. Open Surgery
There are two ways to perform Gastric Bypass: laparoscopically or as open surgery. Laparoscopic surgery uses smaller incisions, leading to a quicker recovery. Open surgery, with its larger incision, may require a longer recovery time.
Step-by-Step Surgical Process
The process starts with the patient under general anesthesia. The surgeon then creates a small stomach pouch, often using a laparoscopic method. Next, the small intestine is rearranged to bypass part of the digestive tract.
This rearrangement reduces food absorption, promoting weight loss. The procedure demands precision and skill to ensure the stomach pouch is the right size and the intestinal rearrangement is accurate.
Duration and Hospital Stay
Gastric Bypass Surgery typically lasts 2-4 hours. Patients usually spend 1-3 days in the hospital for observation and initial recovery.
Recovery After Gastric Bypass
A successful recovery after gastric bypass surgery requires a detailed plan. This includes post-op care and a gradual return to normal activities. The recovery process is key to achieving the surgery’s goals and transitioning to a healthier lifestyle.
Immediate Post-Op Period
Right after surgery, patients are watched closely for any issues. They usually stay in the hospital for a few days. During this time, they are given clear liquids to aid in stomach healing. Pain management is also a focus, with medication to reduce discomfort.
First Few Weeks
In the initial weeks, patients move from a liquid diet to pureed foods. It’s vital to stick to the dietary advice from healthcare professionals to avoid problems. They are also encouraged to start with short walks and gradually increase their physical activity.
Return to Normal Activities
As recovery advances, patients can begin to return to their usual activities. This includes both physical activity and getting back into work and social life.
Physical Activity Guidelines
Patients should begin with gentle exercises like walking and then move to more intense activities. It’s important to listen to the body and avoid overexertion, which can cause complications.
Work and Social Reintegration
The time frame for returning to work varies based on the job and individual recovery. Most people can go back to work in 2-6 weeks. Social reintegration should also be gradual, allowing the body to adjust to new dietary and physical demands.
Post-Gastric Bypass Diet Progression
The post-gastric bypass diet is a gradual progression that aids the stomach in healing and adapting to its new anatomy. This dietary journey is essential for recovery and long-term success after gastric bypass surgery.
Liquid Phase
The initial phase post-surgery involves a liquid diet, lasting one to two weeks. This phase is critical for allowing the stomach to heal without being strained by solid foods. Patients are advised to consume clear broths, electrolyte-rich beverages, and sugar-free gelatin.
Pureed Foods Phase
After the liquid phase, patients progress to pureed foods, which are easier to digest than solid foods but provide more texture than liquids. This phase usually lasts for a few weeks and includes foods like pureed vegetables, fruits, and lean proteins.
Soft Foods Phase
Once patients can tolerate pureed foods, they can start introducing soft foods into their diet. This includes foods that are soft in texture, such as cooked vegetables, soft fruits, and tender meats. This phase helps patients gradually adjust to eating more solid foods.
Regular Diet Adaptation
The final phase involves adapting to a regular diet, which should be balanced and nutritious. Patients are advised to eat smaller, more frequent meals and to chew their food thoroughly. It’s also important to prioritize protein-rich foods and to avoid high-calorie or high-sugar foods.
Throughout these phases, it’s vital for patients to follow the specific dietary guidelines provided by their healthcare team. This ensures a smooth recovery and optimal weight loss outcomes.
Long-Term Lifestyle Changes
Success after Gastric Bypass surgery depends on lasting changes in diet and exercise. These changes are key for both weight loss and better health.
Dietary Guidelines
Following specific dietary guidelines is critical for patients after Gastric Bypass. It’s important to be mindful of portion sizes and choose foods wisely.
Portion Control
Controlling portion sizes is essential to prevent overeating. This can cause discomfort and complications. Patients should use smaller plates and stick to serving sizes recommended by their healthcare provider.
Food Choices and Meal Planning
Healthy food choices and meal planning are vital for a balanced diet. Focus on nutrient-dense foods like lean proteins, vegetables, and whole grains.
Exercise Recommendations
Regular exercise is vital for weight management and health. Patients should aim for a mix of cardio, strength training, and flexibility exercises.
Vitamin and Mineral Supplementation
Due to Gastric Bypass surgery’s malabsorptive nature, patients may need vitamin and mineral supplements. Regular monitoring and adjustments to supplements are necessary based on lab results and healthcare provider advice.
Follow-Up Care and Monitoring
Follow-up care is a critical part of the gastric bypass journey. It helps patients overcome challenges and achieve lasting success. After surgery, patients need ongoing monitoring to ensure their health and address any complications.
Regular Check-Ups
Regular visits with healthcare providers are key to monitoring progress and addressing concerns. These visits are scheduled at intervals like weekly, monthly, or quarterly, based on the patient’s needs.
- Monitoring weight loss progress
- Assessing nutritional deficiencies
- Addressing any complications or concerns
Lab Work and Testing
Lab work and testing are essential for follow-up care. They help healthcare providers check nutritional status, watch for complications, and adjust treatment plans as needed.
Common lab tests include:
- Complete blood count (CBC)
- Nutritional deficiency screening
- Liver function tests
Support Groups
Joining support groups is highly recommended for gastric bypass patients. It offers a space to share experiences, get guidance, and connect with others who have gone through similar journeys.
Gastric Bypass vs. Other Weight Loss Surgeries
Gastric Bypass is among several surgical weight loss options. It’s important to understand its differences from other surgeries. As obesity rates climb, the need for effective weight loss solutions has grown. This has led to the development of various surgical options.
Each weight loss surgery has its own benefits and drawbacks. Here’s a comparison of Gastric Bypass with other popular weight loss surgeries:
Gastric Sleeve Comparison
Gastric Sleeve surgery removes a large portion of the stomach, leaving a narrow sleeve-like stomach. It’s less invasive than Gastric Bypass and doesn’t involve rerouting the intestines.
- Gastric Sleeve is associated with fewer nutritional deficiencies.
- Gastric Bypass often results in greater weight loss.
- Both procedures are effective for weight loss, but the choice depends on individual health needs.
Gastric Band Comparison
Gastric Banding involves placing an adjustable band around the upper part of the stomach to create a small pouch. Unlike Gastric Bypass, it doesn’t involve cutting or stapling the stomach.
- Gastric Banding is reversible, whereas Gastric Bypass is not.
- Gastric Bypass generally leads to more significant weight loss.
- Gastric Banding requires more frequent follow-up visits for band adjustments.
Duodenal Switch Comparison
Duodenal Switch is a more complex procedure that involves removing a large portion of the stomach and rerouting the intestines.
- Duodenal Switch can result in more significant weight loss than Gastric Bypass.
- It carries a higher risk of nutritional deficiencies due to the malabsorptive component.
- Both procedures require lifelong vitamin and mineral supplementation.
The choice between Gastric Bypass and other weight loss surgeries depends on individual factors. These include health status, weight loss goals, and personal preferences. Consulting with a healthcare professional is essential to determine the most suitable option.
Cost and Insurance Coverage for Gastric Bypass
Deciding on gastric bypass surgery often involves understanding the costs and insurance coverage. The financial aspects are complex, covering surgery, pre-op evaluations, post-op care, and possible complications.
Average Costs in the United States
In the United States, gastric bypass surgery costs range from $15,000 to $25,000. Costs vary based on the surgeon’s fee, hospital charges, location, and complications.
Insurance Requirements
Insurance coverage for gastric bypass surgery varies widely. It depends on the provider and policy specifics. Most insurers require a documented obesity history, failed weight loss attempts, and a team evaluation for approval.
Financing Options
For those without adequate insurance, financing options exist. Many surgical centers offer payment plans or financing programs. It’s vital for candidates to explore these options and discuss them with their healthcare provider.
Taking the Next Step: Making an Informed Decision
Choosing to have Gastric Bypass surgery is a major life choice that demands thorough thought. It’s about grasping the procedure, its advantages, and possible downsides. This knowledge is key to making a well-informed choice about Gastric Bypass.
Seeking advice from healthcare experts is vital. They offer tailored advice, considering your unique health situation and needs. This ensures you’re well-suited for Gastric Bypass and ready for the lifestyle adjustments it brings.
Collaborating with a healthcare team provides a full picture of what surgery entails. This includes what happens before, during, and after the procedure. Such teamwork helps individuals make choices that match their health aspirations, leading to better overall health.
FAQ About Gastric Bypass
Q: What is Gastric Bypass surgery?
A: Gastric Bypass surgery, also known as Roux-en-Y Gastric Bypass, is a surgical procedure. It creates a small stomach pouch. The intestine is then rerouted to promote weight loss.
Q: How does Gastric Bypass surgery work?
A: This surgery combines a restrictive component and a malabsorptive component. The restrictive part limits food intake. The malabsorptive part reduces nutrient absorption, leading to significant weight loss.
Q: What are the benefits of Gastric Bypass surgery?
A: Gastric Bypass surgery offers significant weight loss. It also improves or resolves obesity-related health conditions like Type 2 diabetes. It positively impacts cardiovascular health and overall quality of life.
Q: What are the risks and possible complications of Gastric Bypass surgery?
A: Risks and complications include short-term surgical risks and long-term complications. Nutritional deficiencies are also a concern. Proper post-surgical care is essential.
Q: Who is an ideal candidate for Gastric Bypass surgery?
A: Ideal candidates have a high BMI and have tried other weight loss methods. They must meet specific health criteria, including certain health conditions and psychological readiness.
Q: What does the Gastric Bypass evaluation process involve?
A: The evaluation process includes medical, psychological, and nutritional assessments. It determines candidacy and prepares patients for the procedure.
Q: How should I prepare for Gastric Bypass surgery?
A: Preparation involves dietary changes and lifestyle adjustments. Medical preparations include a pre-surgery diet and necessary medical tests.
Q: What is the recovery process like after Gastric Bypass surgery?
A: Recovery involves a gradual return to normal activities. Dietary adjustments and follow-up care are necessary for a smooth recovery.
Q: What dietary changes are required after Gastric Bypass surgery?
A: Patients progress through different dietary phases. These include liquid, pureed, soft, and regular foods. Long-term dietary adjustments and nutritional supplementation are required.
Q: How does Gastric Bypass compare to other weight loss surgeries?
A: Gastric Bypass surgery is compared to Gastric Sleeve and Gastric Band. Differences exist in procedure, benefits, and complications.
Q: What are the costs associated with Gastric Bypass surgery, and what are the insurance coverage options?
A: Costs vary by location and insurance provider. Different insurance requirements and financing options are available to help cover costs.
Q: Why is follow-up care important after Gastric Bypass surgery?
A: Follow-up care is essential for monitoring health and addressing complications. Regular check-ups, lab work, and support group participation are necessary for long-term success.