Prostate cancer is a big worry for men, and radiation therapy is often used to treat it. The number of treatments needed can change based on the therapy type and the patient’s health. There are two main types of radiation therapy: external beam radiation therapy (EBRT) and brachytherapy. EBRT is given over several weeks, with treatments five days a week. Brachytherapy means tiny radioactive seeds are placed in the prostate gland.
For cancers that grow fast, doctors might use both therapies together. This is explained on Acibadem International. Knowing how many radiation treatments are best, including how many radiation treatments for prostate cancer, is key to managing prostate cancer well. The number of treatments needed depends on the cancer’s stage and the patient’s health.
Understanding Radiation Therapy for Prostate Cancer
This article will address how many radiation treatments for prostate cancer are typically recommended.
Radiation therapy is a key part of treating prostate cancer. It uses radiation to kill cancer cells. This method is non-surgical and helps control the disease.
What Radiation Therapy Involves
Radiation therapy targets the prostate gland with high-energy rays. It aims to kill cancer cells while protecting healthy tissue. This is done through precise planning and delivery.
The first step is simulation. CT scans map the prostate and nearby areas. This helps plan the treatment, setting the right angles and doses of radiation.
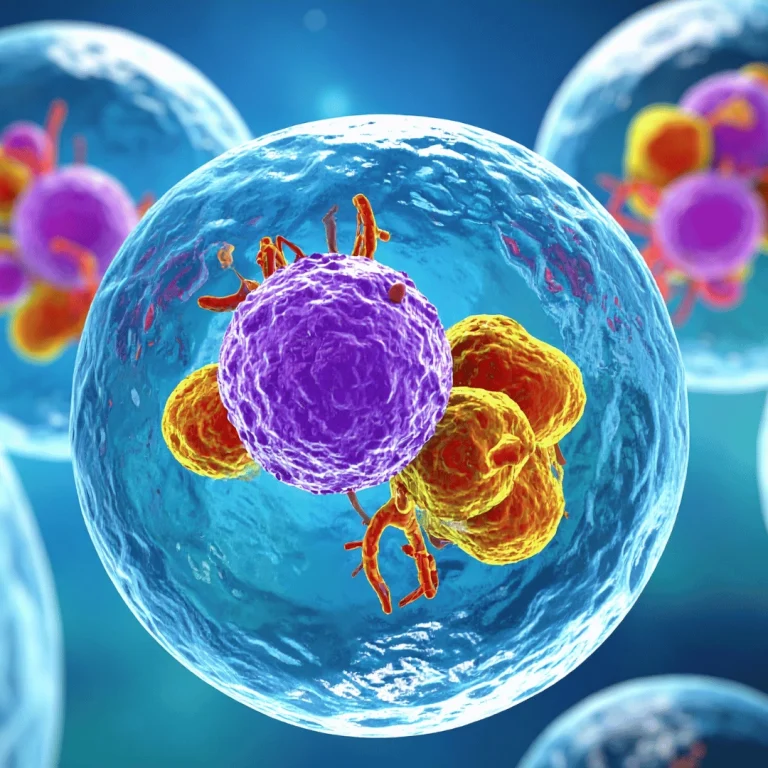
How Radiation Destroys Cancer Cells
Radiation damages cancer cells’ DNA, stopping them from growing. When exposed to radiation, cancer cells’ DNA breaks. This leads to cell death or stops cell division. Over time, the tumour size decreases, controlling the cancer.
For more details on prostate cancer treatments, including radiation, visit Acıbadem International. They offer in-depth information on various treatment options.
The Role of Radiation in Prostate Cancer Management
Radiation therapy is vital in prostate cancer management. It can be tailored to each patient’s needs. It’s used as a primary treatment for early-stage cancer or with other therapies for more advanced cases.
Choosing radiation therapy depends on several factors. These include the cancer’s stage and grade, the patient’s health, and personal preferences. Understanding radiation therapy helps patients make informed treatment decisions.
Types of Radiation Therapy Available for Prostate Cancer
Radiation therapy for prostate cancer is not a one-size-fits-all treatment. It comes in several forms, each tailored to the individual patient’s needs and the specific characteristics of their cancer.
External Beam Radiation Therapy (EBRT)
EBRT is a non-invasive treatment. It uses high-energy beams from outside the body to target and destroy cancer cells. This method has become increasingly sophisticated with advancements in technology.
Intensity-Modulated Radiation Therapy (IMRT)
IMRT is a type of EBRT that allows for precise modulation of the radiation beam’s intensity. This precision enables doctors to deliver higher doses to the tumor while minimizing exposure to surrounding healthy tissues.
Image-Guided Radiation Therapy (IGRT)
IGRT involves the use of imaging technologies to guide the delivery of radiation therapy. This ensures accurate targeting of the tumor, even when it moves during treatment.
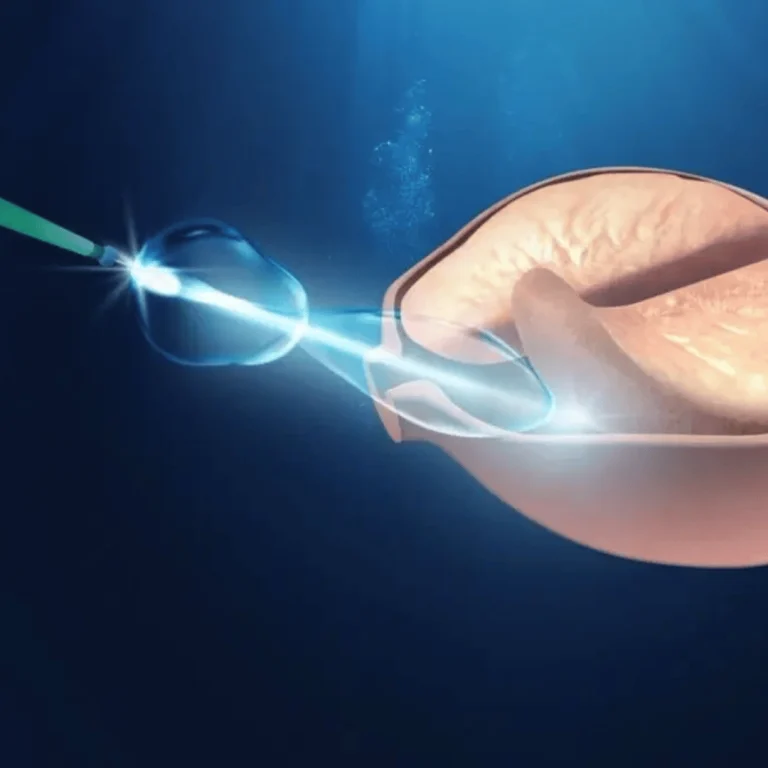
Brachytherapy (Internal Radiation)
Brachytherapy involves placing radioactive material directly inside or near the tumor. This approach allows for the delivery of high doses of radiation directly to the cancer cells.
Low-Dose Rate Brachytherapy
In low-dose rate brachytherapy, small radioactive seeds are implanted permanently in the prostate. The radiation is delivered at a low dose over a period of weeks or months.
High-Dose Rate Brachytherapy
High-dose rate brachytherapy involves temporary placement of a radioactive source near the tumor, delivering radiation at a high dose rate over a short period. This method is often used in combination with other treatments.
Stereotactic Body Radiation Therapy (SBRT)
SBRT delivers precise, high doses of radiation to the tumor in a few fractions. This approach is less invasive and can be completed more quickly than some other forms of radiation therapy.
Understanding the different types of radiation therapy available for prostate cancer is key to making informed decisions about treatment. Each method has its advantages and is suited to different patient needs and cancer characteristics.
Standard Treatment Protocols and Session Frequencies
Standardising treatment for prostate cancer involves many factors. We aim to give the right amount of radiation to the tumour. This helps avoid harming healthy tissues nearby.
Conventional Fractionation Schedules
Conventional fractionation means giving radiation in small doses, five days a week. This goes on for several weeks. It helps deliver a high dose safely. The usual schedule is 37 to 41 fractions over 7 to 8 weeks.
Hypofractionated Radiation Therapy
Hypofractionated therapy gives bigger doses less often, over a shorter time. It’s good for some patients and means fewer visits. It can be 20 fractions over 4 weeks or 5 fractions in 1 to 2 weeks.
Ultra-Hypofractionation Approaches
Ultra-hypofractionation, or SBRT, uses very high doses in just a few fractions, often 5 or less. It’s precise and can be done in 1 to 2 weeks. SBRT is gaining popularity for its benefits and convenience.
Determining the Optimal Protocol for You
The right radiation therapy depends on several things. These include the cancer’s stage, your health, and what you prefer. Your oncologist will look at these to suggest the best plan. It’s key to talk to your doctor about your options and worries.
How Many Radiation Treatments For Prostate Cancer Are Typically Required
Knowing how many radiation treatments you’ll need for prostate cancer helps you get ready. The number of sessions depends on the type of radiation and your personal health.
External Beam Radiation Therapy Treatment Numbers
External Beam Radiation Therapy (EBRT) is a common treatment for prostate cancer. The number of sessions can change based on the treatment plan.
Conventional EBRT: 40 to 45 Sessions
Conventional EBRT usually means 40 to 45 sessions. These are given daily, Monday to Friday, over eight to nine weeks.
Moderate Hypofractionation: 20 to 28 Sessions
Moderate hypofractionation has fewer sessions, from 20 to 28. It uses higher doses of radiation in each session.
Stereotactic Body Radiation Therapy Session Requirements
Stereotactic Body Radiation Therapy (SBRT) is precise and needs fewer sessions.
Five-Session SBRT Protocols
Some SBRT plans include five sessions. These are given every other day, finishing in a week or two.
Single-Session Options
In some cases, SBRT can be done in a single session. But this is rare and depends on your health and the cancer.
Brachytherapy Procedure Frequency
Brachytherapy, or internal radiation, puts radioactive material in the prostate. The number of procedures can vary.
The number of radiation treatments for prostate cancer depends on the type of therapy and your health. This includes the cancer’s stage and your overall health.
Factors That Determine Your Treatment Frequency
Choosing the right frequency for radiation treatment is complex. It depends on many factors. Each patient’s treatment plan is made just for them, based on their unique situation.
Cancer Stage and Risk Classification
The stage and risk of prostate cancer are key in setting treatment frequency. These factors help doctors decide how intense the treatment should be.
Low-Risk Prostate Cancer
Patients with low-risk prostate cancer might have less intense treatment. They could get radiation therapy with fewer sessions. This approach aims to reduce side effects while controlling the cancer.
Intermediate-Risk Prostate Cancer
Those with intermediate-risk prostate cancer might need more frequent radiation. The goal is to find a balance between treating the cancer and managing side effects.
High-Risk and Locally Advanced Disease
High-risk or locally advanced prostate cancer often needs a stronger treatment plan. This might include a mix of therapies, like radiation, with a specific schedule to boost effectiveness.
Patient Health Status and Age Considerations
A patient’s health and age are very important in planning radiation therapy. Older patients or those with health issues might need a treatment schedule that’s easier to handle.
Treatment Goals and Oncologist Recommendations
The main aim of radiation therapy is to control or cure cancer with minimal side effects. Oncologists look at many things, like the patient’s health and wishes, when setting treatment frequency. The Radiation Therapy Protocol for Prostate Cancer is tailored to meet each patient’s needs.
Understanding these factors helps patients see why their Prostate Cancer Radiation Dose Schedule is set the way it is. It makes them appreciate the thought behind their treatment frequency.
Duration and Timeline of Radiation Treatment Programmes
The time needed for radiation therapy for prostate cancer is important for both patients and doctors. Treatment plans aim to be effective while keeping the patient’s quality of life good.
Weekly Treatment Schedules Explained
How often you get radiation therapy can change based on the type and the plan. Treatments usually happen from Monday to Friday. Some plans might need you to have sessions every day.
External Beam Radiation Therapy (EBRT) is given Monday to Friday. Each session is short, lasting just a few minutes. The exact time can vary, depending on the method used, like Intensity-Modulated Radiation Therapy (IMRT).
Total Treatment Duration by Type
The length of radiation treatment changes based on the type used.
Conventional EBRT Timeline: 8 to 9 Weeks
Conventional EBRT lasts 8 to 9 weeks. This long time helps spread out the radiation dose. It helps protect the healthy tissues around the prostate.
Hypofractionated EBRT Timeline: 4 to 6 Weeks
Hypofractionated EBRT is faster, lasting 4 to 6 weeks. It gives more radiation in each session. This means fewer sessions overall.
SBRT Timeline: 1 to 2 Weeks
Stereotactic Body Radiation Therapy (SBRT) is very precise. It can be done in just 1 to 2 weeks. SBRT gives high doses in each session, making it good for those with tight schedules.
Breaks and Interruptions in Treatment
Even though treatment is usually continuous, breaks can happen. These might be for machine checks, side effects, or health issues.
Talking to your radiation oncologist about any worries about breaks is key. They can explain how it might affect your treatment.
What Happens During Each Radiation Treatment Session
Radiation therapy for prostate cancer is a series of precise sessions. Knowing what happens in each session can ease worries and prepare patients.
Pre-Treatment Preparation and Positioning
Before treatment starts, patients prepare and position themselves. They lie on a couch, usually on their back. This ensures the radiation beams hit the prostate accurately. Immobilisation devices help keep the right position.
The Actual Treatment Process
The radiation therapist leaves the room, and the machine delivers the radiation. The machine moves around the patient to hit the prostate from different angles. This process is painless and short, lasting a few minutes.
Duration of Each Individual Session
Each session’s length varies, but most are short, lasting 15 to 30 minutes. The actual radiation part is just a few minutes.
Post-Session Monitoring and Immediate Aftercare
After treatment, patients are watched for any immediate side effects. Usually, they can go back to normal activities soon after. For more on radiation treatments for other cancers, like breast cancer, visit Acibadem International.
While the treatment itself is simple, the prep and planning are key to its success. Patients should follow their radiation oncologist’s advice closely for the best results.
Comparing Different Radiation Treatment Regimens
It’s key for prostate cancer patients to know about the various radiation treatments. The right choice depends on the cancer stage, health, and personal wishes.
Efficacy Rates Across Treatment Types
Each radiation therapy has its own success rate. External Beam Radiation Therapy (EBRT) and Stereotactic Body Radiation Therapy (SBRT) are often used. They show high success rates for early cancer. Brachytherapy, or internal radiation, also works well but has different side effects.
Time Commitment and Convenience Factors
The time and frequency of treatments differ a lot. EBRT needs daily visits, Monday to Friday, for weeks. SBRT, on the other hand, has fewer sessions, 5 to 7, over a shorter time. Brachytherapy might be one session or more, depending on the method.
Advantages and Disadvantages of Each Approach
Every radiation treatment has its good and bad sides. SBRT, for instance, is great because it’s quicker. This is good for those with tight schedules or far from treatment centers.
Benefits of Fewer Sessions
Having fewer sessions, like in SBRT, means less time in treatment. It also might lead to fewer side effects because of its precise delivery.
Potential Drawbacks of Accelerated Treatment
But, SBRT might not fit all, like those with advanced cancer. It could lead to more side effects or need for more treatments. This should be thought over carefully.
In summary, picking a radiation treatment for prostate cancer means looking at success rates, time needed, and each treatment’s pros and cons. Patients should talk to their doctor to find the best option for them.
Side Effects and How They Relate to Treatment Frequency
The frequency of radiation treatment for prostate cancer can affect the side effects patients experience. Radiation therapy uses high-energy rays to kill cancer cells. It can cause side effects during and after treatment.
Acute Side Effects During Treatment
Patients may face several side effects during radiation therapy. These can change based on the treatment’s dose and frequency.
Urinary Symptoms
Urinary symptoms are common during treatment. These include frequency, urgency, and discomfort while urinating. More frequent treatments might make symptoms worse.
Bowel Changes
Bowel changes, like diarrhoea or constipation, can happen. Radiation can affect bowel habits. The treatment’s frequency and dose can influence how severe these changes are.
Fatigue and General Weakness
Fatigue is a big side effect of radiation therapy. Many patients feel weak and tired. Treatment duration and frequency can make fatigue worse, affecting daily life.
Late Side Effects Following Treatment Completion
After treatment, some side effects may go away, while others can stay or appear. These late side effects can greatly affect a patient’s quality of life.
Long-Term Urinary Issues
Long-term urinary issues, like incontinence or persistent frequency, can happen after treatment. The risk depends on the total dose and frequency of radiation.
Erectile Dysfunction
Erectile dysfunction is a possible late side effect. The risk can be influenced by the treatment’s dose and duration. For more information, visit https://acibademinternational.com/chemotherapy-side-effects/.
Rectal Complications
Rectal complications, such as rectal bleeding or pain, can occur as late side effects. The risk depends on the treatment’s frequency and dose.
Managing Side Effects Throughout Your Treatment Course
Managing side effects well is key to maintaining quality of life during and after treatment. This can involve medications, lifestyle changes, and supportive care measures. Knowing about side effects and how treatment frequency affects them helps patients and healthcare providers make better decisions.
Radiation Dose Calculations and Safety Protocols
Effective radiation therapy for prostate cancer needs a good grasp of dose calculations and safety rules. Radiation oncologists must plan and deliver the right dose. This dose should kill cancer cells but not harm healthy tissue.
How Radiation Doses Are Measured and Prescribed
Radiation doses are measured in Gray (Gy). One Gy is the energy absorbed by one kilogram of matter. The dose is split into fractions. This allows for precise radiation to the tumour while healthy tissue recovers.
Understanding Gray (Gy) Units
The Gray unit is a key measure in radiation therapy. It helps quantify the dose a patient receives. Accurate dosing is critical for effective treatment and to avoid side effects.
Total Dose vs Dose Per Fraction
The total dose and dose per fraction are key to treatment success and safety. A higher total dose might be more effective but raises side effect risks. A lower dose per fraction can lower side effects but might affect treatment success.
Safety Standards and Quality Assurance in the United States
The United States has strict safety and quality standards for radiation therapy. These include regular equipment checks, training for staff, and following treatment protocols.
Protecting Surrounding Healthy Tissue
Keeping healthy tissue safe is a top priority in radiation therapy. Techniques like intensity-modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT) help target the tumour. This reduces harm to nearby healthy tissues.
Understanding radiation dose calculations and following strict safety protocols helps healthcare providers. They can offer effective treatments for prostate cancer patients. This improves outcomes and quality of life.
Success Rates and Treatment Outcomes by Protocol
It’s important to know how well different radiation therapy plans work. This helps patients make better choices. Radiation therapy is a top choice for treating prostate cancer, with different plans showing different results.
Five-Year and Ten-Year Survival Rates
Looking at survival rates helps us see how well radiation therapy works. Five-year and ten-year survival rates are very good for those who get radiation therapy. For example, some studies show that over 90% of patients stay cancer-free for five years with certain treatments.
These rates depend on the cancer’s stage, the patient’s health, and the treatment used. For instance, SBRT is popular because it’s effective and easy to do. It works well for early-stage prostate cancer.
Biochemical Recurrence-Free Survival
Biochemical recurrence-free survival (bRFS) is another key measure. It shows how many patients stay cancer-free without a rise in PSA levels. A higher bRFS rate means the treatment is working well.
Brachytherapy, where radioactive material is placed in the prostate, has high bRFS rates. This is true for patients with low-risk cancer.
Factors Affecting Treatment Success
Many things can affect how well radiation therapy works. These include the cancer’s stage and grade, the patient’s health and age, and the tumour’s characteristics.
The type of radiation therapy also matters a lot. Things like the radiation dose, how many times it’s given, and if it’s used with other treatments can all affect the outcome.
Follow-Up Care and PSA Monitoring
After radiation therapy, regular check-ups are key. These help catch any signs of cancer coming back and manage side effects. Keeping an eye on PSA levels is a big part of this.
Patients usually have regular PSA tests after treatment. How often depends on their risk and treatment details.
Combining Radiation with Other Prostate Cancer Treatments
Prostate cancer treatment often uses a mix of methods. This includes radiation therapy with other treatments. This approach aims to make treatment more effective and better for patients.

Radiation Therapy Plus Androgen Deprivation Therapy
Androgen deprivation therapy (ADT) is often used with radiation for prostate cancer. ADT lowers male hormones that help cancer grow.
Duration of Hormone Therapy
How long ADT lasts depends on the cancer’s stage and the patient’s health. It usually lasts from a few months to a few years.
Benefits of Combined Treatment
Using radiation and ADT together helps more with prostate cancer. It leads to better control of the disease and sometimes longer life.
Adjuvant or Salvage Radiation After Surgery
Radiation therapy can be used after surgery. It can kill any cancer cells left behind or treat cancer that comes back.
Adjuvant radiation is for patients with certain cancer features. Salvage radiation is for those with cancer that comes back after surgery.
Multimodal Treatment Approaches for Advanced Disease
For advanced prostate cancer, treatments are combined. This includes radiation with chemotherapy or new hormone therapies.
This plan aims to control the disease, ease symptoms, and improve life quality for those with advanced cancer.
Making an Informed Decision About Your Treatment Plan
Choosing the right radiation treatment for prostate cancer can be tricky. But with the right info, you can make a smart choice. It’s important to know how different treatments affect your life.
Essential Questions to Ask Your Radiation Oncologist
When you talk to your radiation oncologist, ask important questions. Find out about the type of radiation therapy they suggest. Also, ask about the frequency and duration of treatment sessions and possible side effects.
For example, you might ask, “What’s the difference between External Beam Radiation Therapy (EBRT) and Brachytherapy?” or “How will my treatment change if I have bad side effects?” These questions help you make a better choice.
Evaluating Your Personal Circumstances
Your personal life affects your treatment choice. Think about your work, family, travel, and money. All these things matter.
Work and Family Commitments
How your treatment fits into your work and family life is key. For instance, External Beam Radiation Therapy means daily visits. This can mess with your work and family plans.
Travel Distance to Treatment Centre
How far you have to travel to treatment is important. It might mean moving temporarily or daily trips. Knowing this helps with planning.
Financial and Insurance Considerations
Money matters too. Know what your insurance covers and what you’ll pay yourself. Talk to your doctor and insurance about this.
Seeking Second Opinions and Treatment Selection
Getting a second opinion can give you more info. It can change your treatment plan. It’s a good way to be sure you’re making the right choice.
In short, choosing your prostate cancer treatment needs careful thought. Understand your options, think about your life, and might get a second opinion. Being informed helps you face radiation therapy with confidence.
Conclusion
Understanding radiation therapy for prostate cancer is key to making good treatment choices. The number of treatments needed changes a lot. It depends on the type of therapy, the cancer’s stage, and the patient’s health.
The time needed for radiation therapy varies a lot between patients. It can be a few sessions or several weeks. Each type of therapy, like EBRT, Brachytherapy, and SBRT, has its own schedule.
Doctors look at many things to decide how many treatments you’ll need. They consider the cancer’s stage, your health, and what you want to achieve. Talking to your doctor helps you understand your options and plan your treatment.
The main aim of radiation therapy is to control prostate cancer well. It aims to do this with as few side effects as possible. By being well-informed and working with your team, you can get the best results from your treatment.
FAQ
Q: How many radiation treatments are typically required for prostate cancer?
A: The number of treatments for prostate cancer varies. It depends on the type of therapy and the patient’s condition. For External Beam Radiation Therapy (EBRT), it’s usually 20 to 45 sessions. Stereotactic Body Radiation Therapy (SBRT) needs 5 sessions. Brachytherapy might be one session or more.
Q: What is the difference between conventional fractionation and hypofractionation in radiation therapy for prostate cancer?
A: Conventional fractionation gives smaller doses over a longer time, 40 to 45 sessions. Hypofractionation uses higher doses in fewer sessions. It’s 20 to 28 sessions for moderate hypofractionation and 5 sessions for ultra-hypofractionation or SBRT.
Q: How is the optimal radiation treatment protocol determined for prostate cancer patients?
A: The best treatment plan depends on several factors. These include the cancer’s stage and risk, the patient’s health and age, and treatment goals. The radiation oncologist will consider these to suggest the best option.
Q: What are the common side effects of radiation therapy for prostate cancer, and how are they managed?
A: Side effects include urinary issues, bowel changes, and fatigue. These can be managed with medication, lifestyle changes, and follow-up care with the oncologist.
Q: How does radiation dose calculation impact the treatment outcome for prostate cancer?
A: Calculating the radiation dose is key to treatment success. The dose is measured in Gray (Gy) units. The total dose and dose per fraction are planned to kill cancer cells while protecting healthy tissue.
Q: Can radiation therapy be combined with other treatments for prostate cancer?
A: Yes, radiation can be combined with treatments like androgen deprivation therapy (ADT) or surgery. The choice depends on the patient’s condition and treatment goals.
Q: What should I consider when making an informed decision about my radiation treatment plan?
A: Consider your health, cancer stage and risk, treatment goals, and personal life. Think about work, family, travel to the treatment centre, and finances.
Q: How often are follow-up appointments required after completing radiation therapy for prostate cancer?
A: Follow-ups are needed to check the treatment’s success and for any signs of cancer return. The frequency depends on individual needs.