Hypospadias: What Is Hypospadias?
Hypospadias is a congenital condition in males where the urethra’s opening is not at the tip of the penis. This condition can vary in severity and is typically identified at birth. Understanding hypospadias is vital due to its impact on urinary and reproductive health. Early diagnosis and treatment are key to preventing complications and ensuring the best outcomes.
We will explore the causes, symptoms, and treatment options available for this condition. This will provide a detailed overview for those affected and their families. Understanding hypospadias starts with its definition and how it differs from normal urethral anatomy. It’s a congenital condition where the urethra’s opening is not at the typical location at the tip of the penis.
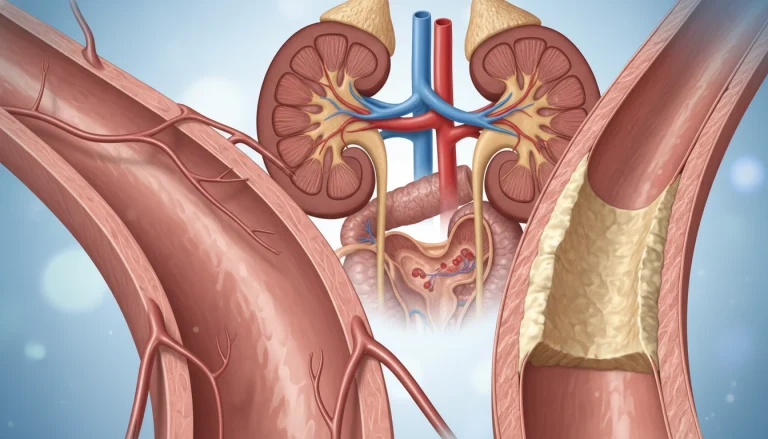
Definition and Anatomical Overview
Hypospadias involves an abnormal urethral opening, which can be located anywhere along the underside of the penis. It ranges from just below the tip to as far back as the scrotum or perineum. This condition results from incomplete development of the urethra and surrounding tissues during fetal development.
Prevalence in the United States
Hypospadias is one of the most common congenital anomalies, occurring in approximately 1 in every 200 male births in the United States. The prevalence has been observed to vary, with some studies suggesting an increase in incidence over the past few decades.
Normal Urethral Development
Normal urethral development involves the fusion of urethral folds to form a tube that extends to the tip of the penis. This process is completed by the 14th to 16th week of gestation. Disruption in this process can lead to hypospadias, highlighting the importance of understanding normal developmental pathways to comprehend the condition.
Types and Classification of Hypospadias
Hypospadias can be categorized into several types, including anterior, middle, and posterior. Each type has distinct characteristics and implications for patient care. Understanding these classifications is key to determining the best treatment approach.
Anterior (Distal) Hypospadias
Anterior hypospadias, also known as distal hypospadias, occurs when the urethral opening is near the tip of the penis. This is the most common form, making up about 70% of cases.
- Mild curvature or no curvature
- Urethral opening is typically on the underside of the penis near the head
- Often associated with a more straightforward surgical repair
Middle Hypospadias
Middle hypospadias is characterized by the urethral opening being along the shaft of the penis. This type represents a moderate form of the condition.
- More significant curvature may be present
- Surgical correction can be more complex
Posterior (Proximal) Hypospadias
Posterior or proximal hypospadias is the most severe form. The urethral opening is closer to the base of the penis or even in the perineum.
- Often associated with significant penile curvature and other genital anomalies
- Surgical repair is typically more complex and may require multiple procedures
Severity Grading Systems
The severity of hypospadias is graded using various classification systems. These systems consider the location of the urethral meatus, the degree of penile curvature, and the presence of other anomalies.
Causes and Risk Factors
The causes of Hypospadias are complex, involving both genetic predisposition and environmental exposures. Understanding these factors is key to identifying risks and managing the condition.
Genetic Predisposition
Genetics significantly influence Hypospadias development. Boys with a family history are more likely to be affected. Specific genetic mutations can disrupt normal urethra and genitalia development.
Environmental Exposures
Exposure to certain environmental factors during pregnancy increases Hypospadias risk. This includes endocrine-disrupting chemicals (EDCs) in plastics, pesticides, and personal care products.
Maternal Health Considerations
Maternal health during pregnancy is critical. Conditions like gestational diabetes and preeclampsia raise Hypospadias risk in newborns.
Recent Epidemiological Findings
Recent studies have provided insights into Hypospadias risk factors. Key findings include:
- An increased risk associated with assisted reproductive technology (ART)
- The impact of maternal nutrition and diet on fetal development
- The role of genetic-environmental interactions in Hypospadias etiology
Associated Conditions and Anomalies
Hypospadias often comes with other conditions that can affect treatment plans. These can make diagnosis and management more complex. A detailed evaluation is essential.
Chordee (Penile Curvature)
Chordee, or penile curvature, is a common issue with hypospadias. It can influence the severity of the condition and the surgical approach. This condition arises from abnormal tissue development around the urethra.
Cryptorchidism (Undescended Testes)
Cryptorchidism, or undescended testes, often accompanies hypospadias. It requires separate assessment and may need surgery to place the testicle in the scrotum.
Inguinal Hernia
Inguinal hernias are more prevalent in individuals with hypospadias. An inguinal hernia happens when tissue, like part of the intestine, bulges through a weak spot in the abdominal muscles.
Disorders of Sexual Development
Hypospadias may also be linked to disorders of sexual development (DSD). These involve variations in gonad, genitalia, or sex chromosome development. A thorough diagnostic process is needed to identify any DSD.
Managing hypospadias effectively requires a team effort. Pediatric urologists, endocrinologists, and other specialists play key roles in the treatment process.
- Chordee can complicate hypospadias repair.
- Cryptorchidism requires separate evaluation.
- Inguinal hernias are more common with hypospadias.
- DSD may be associated with hypospadias in some cases.
Signs and Symptoms of Hypospadias
Understanding the signs and symptoms of hypospadias is key for early diagnosis and effective management.
Physical Presentation in Newborns
Hypospadias is often identified at birth due to its distinct physical characteristics. The condition is marked by the abnormal location of the urethral meatus. This can be found along the underside of the penis, not at the tip.
Some newborns may also exhibit other physical anomalies associated with hypospadias. These include penile curvature or a hooded foreskin.
Functional Implications
The abnormal urethral opening in hypospadias can lead to functional issues. Children with hypospadias may experience a spraying or deflection of the urinary stream.
- Abnormal urinary stream direction
- Difficulty urinating in a standing position
- Increased risk of urinary tract infections
Urinary Stream Abnormalities
One of the common symptoms of hypospadias is an abnormal urinary stream. This can result in difficulties with urination. It may lead to complications if not addressed.
Impact on Development
Hypospadias can have psychological and social implications for affected individuals. This is true, in particular, during childhood and adolescence. The condition may impact self-esteem and body image.
Early correction and supportive care can mitigate these effects. This promotes healthy development and well-being.
Diagnosis Process
Diagnosing Hypospadias involves several steps, from prenatal detection to neonatal examination and sometimes imaging. Accurate diagnosis is key for effective treatment and care.
Prenatal Detection Possibilities
Identifying Hypospadias before birth is difficult and not always possible. Yet, ultrasound technology has advanced, allowing for better detection of genital issues during fetal development. Some cases might be spotted during a detailed ultrasound, mainly if there are other abnormalities present.
Neonatal Physical Examination
Hypospadias is usually diagnosed during the newborn’s physical check-up. Healthcare professionals look for signs like an abnormal urethral opening, penis curvature, and other genital issues. A detailed examination is essential to identify the condition and its severity.
Diagnostic Imaging When Needed
In some instances, imaging is necessary to fully understand the condition’s extent or to spot related issues. Ultrasound is often used due to its non-invasive nature. It offers valuable insights into the urinary tract and genital structures.
Differential Diagnosis
Differential diagnosis is about distinguishing Hypospadias from other conditions with similar symptoms. This step is vital to ensure the right care and treatment. Conditions like epispadias, penile torsion, and sex development disorders must be ruled out.
When to Seek Medical Attention
It’s vital for parents to recognize when their child needs medical help for hypospadias. Being attentive to your child’s health is key. Seek medical assistance when necessary.
Warning Signs for Parents
Parents should be alert to signs that may indicate complications or the need for medical help. These include:
- Swelling or redness around the genital area
- Signs of infection, such as fever or discharge
- Difficulty urinating
- Pain or discomfort during urination
Emergency Situations
At times, emergency medical care is required. Immediate action is needed in the following situations:
- Severe pain or bleeding
- Failure to urinate
- Signs of severe infection
Finding the Right Specialist
Children with hypospadias should see a pediatric urologist. Look for a specialist with experience in hypospadias repair. Their approach to care is also important.
Understanding Hypospadias
Grasping hypospadias demands a broad perspective, covering historical insights, current medical advancements, and the psychological and social impacts. This deep understanding is vital for healthcare professionals and families dealing with hypospadias.
Historical Understanding
Historically, hypospadias was often shrouded in mystery. The term “hypospadias” comes from Greek, with “hypo” meaning “under” and “spadias” referring to “a tearing or rending.” Early writings and treatments were basic and sometimes ineffective.
Over time, our comprehension and treatment of hypospadias have greatly advanced. New surgical methods and a clearer understanding of its causes have significantly improved treatment outcomes.
Modern Medical Perspectives
Modern medicine has significantly advanced in treating hypospadias. New surgical techniques, like tubularized incised plate urethroplasty, have led to better results. Also, a deeper understanding of genetic and environmental factors has improved diagnosis.

Psychological Considerations
The psychological effects of hypospadias on individuals and their families are profound. Children with hypospadias may feel anxious or self-conscious, which can intensify during adolescence. Psychological support and counseling are essential in addressing these emotional challenges.
Social Implications
Hypospadias also has significant social implications for individuals and their families. Stigma, misconceptions, and worries about fertility or sexual function can affect their well-being. Education and awareness are key to overcoming these issues, fostering understanding and acceptance.
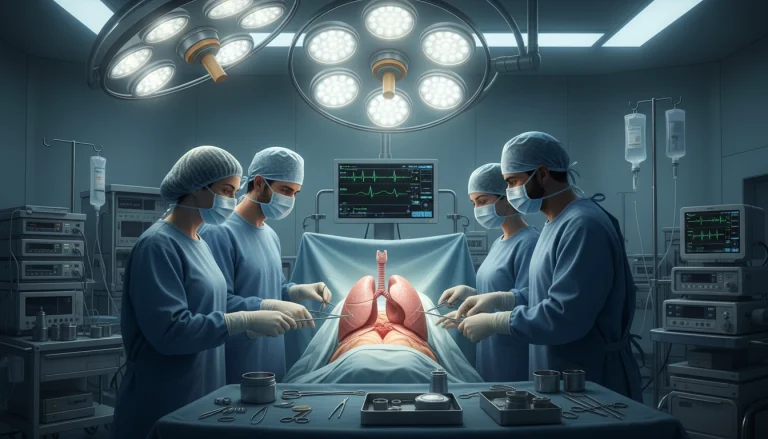
Surgical Treatment Options
Hypospadias repair surgery has seen significant advancements, presenting various treatment options. Choosing to undergo surgery is a major decision. It’s essential to understand the available choices to make an informed choice.
Optimal Timing for Surgery
The debate on the best time for hypospadias surgery among pediatric urologists is ongoing. Most agree that surgery between 6 and 18 months is ideal. This timing is chosen to repair the condition before the child becomes aware of their genital anatomy. This could help minimize the psychological impact.
Common Surgical Techniques
Advances in surgical techniques for hypospadias repair have led to better outcomes. The technique chosen depends on the severity and location of the hypospadias.
- One-stage repairs involve a single surgical procedure to correct the hypospadias.
- Two-stage repairs involve two separate surgeries, often used for more complex cases.
One-Stage Repairs
One-stage repairs are typically used for less severe hypospadias. This method can reduce the need for multiple surgeries, potentially lowering complication risks.
Two-Stage Repairs
Two-stage repairs are recommended for more complex cases. The first stage corrects the chordee (penile curvature). The second stage focuses on urethral reconstruction.
Anesthesia Considerations for Children
Anesthesia for hypospadias surgery in children requires specialized care. Pediatric anesthesiologists are key in ensuring the child’s safety and comfort during the procedure.
Hospital Stay Expectations
The length of hospital stay after hypospadias surgery varies. Modern surgical techniques often allow for outpatient surgery or a short stay. This reduces stress on the child and family.
Non-Surgical Management Approaches
While surgery is often necessary for hypospadias, there are instances where non-surgical management approaches are considered. This approach focuses on monitoring the condition and providing supportive care.
Watchful Waiting Criteria
Watchful waiting involves closely monitoring the child’s condition to determine if surgery is necessary. This approach is considered when the hypospadias is mild and not causing significant urinary or cosmetic issues.
Supportive Care Measures
Supportive care includes measures to ensure the child’s comfort and to prevent complications. This may involve regular check-ups with a pediatric urologist, advice on hygiene, and monitoring for any signs of urinary tract infections.
When Surgery May Be Deferred
Surgery may be deferred in cases where the hypospadias is not severe and not causing functional issues. The decision to defer surgery is made on a case-by-case basis. It considers factors such as the child’s overall health and the risks and benefits of surgery.
Choosing a Pediatric Urologist in the US
Finding the right pediatric urologist is critical for treating hypospadias. This choice greatly affects the treatment’s success and the family’s experience.
Board Certification and Specialization
Ensure the urologist is board-certified by the American Board of Urology (ABU). This certification confirms their training and expertise in pediatric urology.
Experience with Hypospadias Repair
Experience is key in hypospadias repair. Seek a surgeon with a successful history of surgeries.
Questions to Ask Pediatric Urologists
Prepare questions for surgeons, such as their experience with hypospadias, complication rates, and post-operative care.
Insurance and Healthcare Coverage Considerations
Understanding insurance coverage is essential. Make sure the chosen pediatric urologist is in your network to avoid high costs.
Preparing for Hypospadias Surgery
Preparing your child for hypospadias surgery requires several steps to ensure a smooth and successful experience. It’s vital to grasp the process and what to anticipate to ease any worries you or your child might have.
Preoperative Consultations
Preoperative consultations are a key part of the surgical journey. During these meetings, you’ll discuss the surgery with a pediatric urologist. Topics include the surgical method, expected outcomes, and possible risks or complications.
- Discuss the surgical plan and expected results
- Understand the risks and possible complications
- Address any questions or concerns you may have
What to Expect Before Surgery
In the days before surgery, you’ll receive specific instructions on preparing your child. These may cover eating and drinking, managing medications, and other preoperative care details.

Psychological Preparation for Child and Family
Psychological preparation is as critical as physical preparation for your child. Explaining the surgery in terms your child can understand can help reduce anxiety and fear.
- Use age-appropriate language to explain the surgery
- Reassure your child that they will be cared for
- Encourage your child to express their feelings
Packing for the Hospital Stay
Packing the right items for your child’s hospital stay can enhance their comfort. Essentials include comfortable clothing, favorite toys or blankets, and necessary medical records or insurance information.
- Comfortable clothing and personal items
- Medical records and insurance cards
- Snacks and entertainment for the waiting period
Post-Surgical Care and Recovery
The postoperative period is critical for healing and minimizing complications in hypospadias repair. Proper care during this time can significantly impact the overall success of the surgery.
Immediate Postoperative Management
In the immediate aftermath of surgery, monitoring for any signs of complications is critical. This includes watching for bleeding, infection, or issues with urination.
- Monitor the dressing for any signs of bleeding or wetness.
- Observe for signs of infection, such as fever or redness.
- Ensure the child is urinating normally.
Pain Control Strategies
Effective pain management is essential for the child’s comfort and recovery. This may involve a combination of medication and other comfort measures.
Common pain control strategies include:
- Administering pain medication as directed by the healthcare provider.
- Using non-pharmacological methods, such as a warm bath, to soothe the child.
Home Care Instructions
Upon discharge, parents should receive clear instructions on how to care for their child at home. This includes wound care, medication administration, and monitoring for complications.
Activity Restrictions
To prevent complications and promote healing, certain activities may need to be restricted. This can include avoiding strenuous activities or certain positions that could put pressure on the surgical site.
- Avoid heavy lifting or bending.
- Limit bath time to avoid soaking the surgical site.
Follow-up Appointment Schedule
A follow-up appointment schedule will be provided to monitor the healing process and address any concerns or complications that may arise.
Typically, follow-up appointments are scheduled within a few weeks after surgery, with additional visits as necessary based on the child’s recovery.
Potential Complications and Outcomes
Hypospadias repair is often successful but can lead to complications and outcomes. It’s vital for patients to understand these possibilities. This knowledge helps manage expectations and make informed care decisions.
Short-term Complications
Short-term issues after hypospadias surgery include bleeding, infection, and swelling. These are common and usually managed well with proper postoperative care.
Long-term Complications
Long-term problems might involve urethral stricture, fistula formation, or persistent chordee. Regular follow-ups are key to catch and treat these issues early.
Success Rates by Type
The success of hypospadias repair varies by type and severity. Generally, repairs for distal hypospadias have higher success rates than those for more proximal cases.
Reoperation Statistics
Some patients need reoperation due to complications or incomplete initial repair. The need for reoperation varies, highlighting the importance of choosing an experienced surgeon.
Quality of Life Outcomes
Many patients with hypospadias achieve good quality of life after successful repair. They often experience normal urinary and sexual function. Long-term follow-up is necessary to ensure these outcomes.
Living with Hypospadias
Understanding hypospadias involves grasping its psychological, physical, and long-term effects. This condition affects the urethra and penis development, necessitating ongoing care and support. It’s a lifelong journey.
Psychological Impact Through Development
The psychological effects of hypospadias can be profound, hitting hard during childhood and adolescence. Kids with hypospadias might feel anxious or self-conscious, impacting their self-esteem. Knowing the best time for treatment can ease these worries by tackling the physical issues early.
Discussing the Condition with Your Child
Parents must engage in open, honest talks with their children about hypospadias. Explaining it in terms a child can understand helps them deal with their situation better.
Sexual Function in Adulthood
Adults with hypospadias often worry about their sexual function. Research indicates that many men with hypospadias can enjoy normal sexual lives after proper surgery. Yet, the degree of sexual function varies based on condition severity and surgery success.
Fertility Considerations
Fertility is a critical aspect for those with hypospadias. Despite its possible impact, many men with hypospadias can conceive. The success of surgery and any related conditions play a role in fertility outcomes.
Support Resources for Families
Support resources are vital for families facing hypospadias challenges. They offer emotional support, educational materials, and financial aid. This helps families cope with the condition.
National Support Organizations
Many national organizations focus on hypospadias support. They provide detailed information, counseling, and links to local groups. This support is invaluable for families.
Online Communities
Online forums and communities are key for families seeking support. They allow families to share their stories and connect with others. This connection is essential for emotional support.

Educational Materials
Educational materials are essential for understanding hypospadias and its treatments. Organizations offer brochures, videos, and online content. This knowledge empowers families.
Financial Assistance Programs
Financial aid programs ease the financial strain of hypospadias treatment. Some organizations provide grants and financial assistance. This support is critical for families.
Accessing these resources helps families manage hypospadias better. It ensures they receive the necessary support.
Advancing Hypospadias Care
The management and treatment of hypospadias are evolving rapidly. This is due to advancements in surgical techniques and a deeper understanding of the condition. There’s also a growing focus on patient-centered care. Future directions in hypospadias care will likely be influenced by ongoing research into its genetic and environmental factors.
As we gain more insight into hypospadias, our treatment options are becoming more effective. New surgical techniques and the refinement of existing ones are expected to enhance outcomes. The increasing specialization of healthcare professionals and advances in pediatric urology are also contributing to better care.
Multidisciplinary care teams, including pediatric urologists, geneticists, and psychologists, are vital. They play a key role in improving the quality of life for those with hypospadias. Advancing hypospadias care involves exploring new approaches to enhance health and well-being.
FAQ
Q: What is Hypospadias?
A: Hypospadias is a congenital condition where the urethra’s opening is not at the tip of the penis but somewhere on the underside.
Q: How common is Hypospadias?
A: Hypospadias occurs in about 1 in every 200 to 300 male births, making it one of the most common congenital anomalies.
Q: What are the different types of Hypospadias?
A: The condition is classified into anterior (distal), middle, and posterior (proximal) Hypospadias based on the location of the urethral opening.
Q: What causes Hypospadias?
A: The exact cause is often unknown, but it involves a combination of genetic, hormonal, and environmental factors during fetal development.
Q: How is Hypospadias diagnosed?
A: Diagnosis is typically made at birth or during early infancy through a physical examination by a healthcare provider.
Q: Can Hypospadias be detected prenatally?
A: While some cases might be suspected during prenatal ultrasounds, a definitive diagnosis is usually made after birth.
Q: What are the associated conditions with Hypospadias?
A: Conditions like Chordee (penile curvature), Cryptorchidism (undescended testes), and Inguinal Hernia are sometimes associated with Hypospadias.
Q: What is the treatment for Hypospadias?
A: Surgical repair is the primary treatment, with the goal of correcting the urethral opening, improving the appearance of the penis, and ensuring normal urinary and sexual functions.
Q: When is the best time for Hypospadias surgery?
A: The optimal timing for surgery is typically between 6 to 18 months of age, depending on the complexity of the case and the child’s overall health.
Q: What are the possible complications of Hypospadias surgery?
A: Complications can include infection, bleeding, urethral stricture, fistula formation, and the need for additional surgeries.
Q: How can families cope with Hypospadias?
A: Support from healthcare providers, national organizations, online communities, and educational resources can help families manage the condition and its treatment.
Q: What is the long-term outlook for individuals with Hypospadias?
A: With successful surgical repair, most individuals can expect normal urinary and sexual functions, though some may require ongoing medical care or additional surgeries.