Lung Transplantation: What is Lung Transplantation?
For those with end-stage lung disease, a complex surgery offers a second chance at life. This operation involves replacing a failing organ with a healthy one from a donor. It’s a life-saving procedure. This surgery is considered for patients who have tried all other treatments and face a poor prognosis. Understanding the conditions that require lung replacement, patient selection criteria, and the different transplant procedures available is key. It helps individuals navigate this life-changing surgery.
Advances in medical technology continue to improve lung replacement success rates. This offers new hope to those in need. Lung transplantation is a complex surgical procedure that has transformed the treatment of end-stage lung disease. It involves replacing a diseased or failing lung with a healthy one from a donor. The goal is to restore lung function and enhance the patient’s quality of life.
Definition and Medical Purpose
Lung transplantation is the surgical replacement of a diseased or failing lung with a healthy one from a donor. Its primary medical purpose is to restore lung function in patients with end-stage lung disease. This aims to improve their survival chances and overall quality of life.
The medical purpose of lung transplantation is multifaceted:
- To improve lung function and overall health
- To increase survival rates for patients with end-stage lung disease
- To enhance the quality of life for transplant recipients
Historical Development and Milestones
The history of lung transplantation began in the 1960s, with the first successful transplant in 1963. The procedure has seen significant advancements. These have been driven by improvements in surgical techniques, immunosuppressive medications, and post-operative care.
Key milestones in lung transplantation development include:
- The introduction of cyclosporine in the 1980s, which significantly improved graft survival rates
- Advances in surgical techniques and organ preservation methods
- The establishment of lung allocation systems to prioritize transplant candidates
Conditions Requiring Lung Transplantation
Lung transplantation is considered for individuals with advanced lung diseases that have not responded to other treatments. Various end-stage lung conditions may necessitate this surgical intervention to improve the quality of life and survival.

Chronic Obstructive Pulmonary Disease (COPD)
Chronic Obstructive Pulmonary Disease (COPD) is a leading indication for lung transplantation. It is characterized by airflow limitation that is not fully reversible. COPD encompasses conditions such as emphysema and chronic bronchitis. Patients with severe COPD who have not benefited from other treatments may be considered for lung transplantation.
Idiopathic Pulmonary Fibrosis (IPF)
Idiopathic Pulmonary Fibrosis (IPF) is another common condition that leads to lung transplantation. It is marked by progressive scarring of the lungs, resulting in decreased lung function and often severe shortness of breath. The prognosis for IPF is generally poor, making lung transplantation a critical treatment option for eligible patients.
Cystic Fibrosis (CF)
Cystic Fibrosis (CF) is a genetic disorder that leads to severe lung damage and is a significant indication for lung transplantation in younger patients. CF affects the respiratory, digestive, and reproductive systems by creating thick mucus that clogs the lungs and obstructs the pancreas. Lung transplantation can significantly improve the quality of life for CF patients with advanced lung disease.
Other Qualifying Conditions
Other conditions that may qualify a patient for lung transplantation include pulmonary hypertension, bronchiolitis obliterans, and lymphangioleiomyomatosis. These conditions often result in significant morbidity and mortality, and lung transplantation can be a life-saving intervention.
Patient Selection Criteria
The process of selecting candidates for lung transplantation is highly detailed. It involves examining both medical and psychological aspects. This thorough evaluation aims to ensure that those undergoing the transplant have the highest chance of success.
Medical Requirements
Patients must have severe lung disease with a poor prognosis. They should also be free from significant problems in other organs. A reasonable life expectancy post-transplant is essential. The evaluation assesses the severity of lung disease, overall health, and recovery prospects.
Psychological Considerations
Psychological evaluation is key to determining a patient’s ability to handle transplant-related stress. It looks at their mental health, social support, and capacity to manage post-transplant medication. This is vital for their recovery.
Absolute and Relative Contraindications
Absolute contraindications include active cancer, severe heart disease, and significant liver or kidney issues. Relative contraindications might include advanced age, poor nutrition, and psychosocial challenges. These factors are carefully weighed to determine if a patient is suitable for the transplant.
Types of Lung Transplant Procedures
There are various lung transplant procedures, each tailored to different medical needs. The choice of procedure depends on the patient’s specific condition and needs. This ensures the best possible outcome for each individual.
Single Lung Transplantation
Single lung transplantation involves replacing one diseased lung with a healthy one. It’s often chosen for patients with certain lung diseases, where the other lung is functioning well.
- Typically considered for patients with restrictive or obstructive lung disease.
- Less complex compared to bilateral lung transplantation.
- May be preferred for patients with less severe pulmonary hypertension.
Bilateral Lung Transplantation
Bilateral lung transplantation replaces both lungs. It’s often the preferred option for patients with cystic fibrosis or other conditions affecting both lungs.
- Commonly performed in younger patients or those with suppurative lung disease.
- Requires a more extensive surgical procedure compared to single lung transplantation.
- Can offer better long-term outcomes for certain patient populations.
Heart-Lung Transplantation
Heart-lung transplantation involves replacing both the lungs and heart. This complex procedure is typically reserved for patients with severe cardiac and pulmonary disease.
- Performed on patients with Eisenmenger’s syndrome or other combined heart and lung conditions.
- Requires a high level of surgical expertise.
- Can be an effective treatment for patients with complex cardiopulmonary disease.
Living Donor Lobar Transplantation
Living donor lobar transplantation is a less common procedure. Two living donors each donate a lobe, which are then implanted into the recipient.
- Typically considered for patients who are unlikely to receive a transplant from a deceased donor in time.
- Involves complex surgical planning and coordination.
- Can be a viable option for certain patients, such as children or those with rapidly deteriorating lung function.
Each procedure has its own indications, benefits, and risks. The decision on which type of lung transplant to perform is made after a thorough evaluation of the patient’s condition and needs.
The Comprehensive Evaluation Process
Before lung transplantation, patients undergo a detailed evaluation. This checks their health and if they’re a good fit for the surgery. The process includes medical tests, a team of experts, and looking at financial and insurance matters.
Required Medical Testing
The medical tests aim to check the patient’s health and spot any risks for lung transplant. Tests include lung function checks, heart evaluations, CT scans, and blood tests. These help understand the patient’s blood chemistry and immune system.
Multidisciplinary Team Assessment
A team of doctors and experts reviews the patient’s medical, mental, and social health for transplant. This team includes lung doctors, heart specialists, surgeons, psychologists, and social workers. They look at the patient’s health, recovery chances, and ability to follow post-transplant care.
Financial and Insurance Considerations
Lung transplant costs are high, so the evaluation looks at the patient’s finances and insurance. It makes sure the patient can afford the transplant, care after surgery, and ongoing medication. Financial advisors help patients understand their insurance and find financial help.
The Organ Allocation System
The lung allocation system aims to transplant available lungs to the most urgent candidates quickly. It evaluates patients based on their medical condition, waiting time, and other key factors. This ensures a balance between the urgency of transplantation and the availability of donor organs.
How the Waiting List Works
Patients waiting for lung transplants are listed on a waiting list by the United Network for Organ Sharing (UNOS). The list changes as patients are added or removed based on their health status. It’s not a simple first-come, first-served system. Instead, it prioritizes patients based on their medical urgency.
Lung Allocation Score (LAS)
Each patient on the waiting list gets a Lung Allocation Score (LAS), ranging from 0 to 100. The LAS is calculated from factors like lung function, diagnosis, and waiting time. A higher score means a greater medical need for a transplant.
Regional Differences in Wait Times
Lung transplant wait times vary by region due to donor availability, population density, and healthcare infrastructure. These differences affect transplant timing and waiting list management. Understanding these variations is key to managing patient expectations and optimizing organ allocation.
Preparing for Lung Transplantation
The journey to lung transplantation requires a detailed plan to boost both physical and emotional health. This thorough approach is key to achieving the best results. It ensures patients are ready for the hurdles that come with lung transplant surgery.
Pulmonary Rehabilitation
Pulmonary rehabilitation is a cornerstone for those waiting for a lung transplant. It focuses on improving lung function and fitness. Through a mix of exercise, education, and support, patients learn to manage symptoms and get in better shape.
Nutritional Optimization
Good nutrition is vital for patients to be strong enough for surgery. A diet that meets their unique needs can boost health and lower the risk of complications. It’s all about being well-nourished for the transplant process.
Mental Preparation and Support Systems
Emotional readiness is just as important as physical health. Counseling and support groups offer the necessary tools to face transplant challenges. They provide the emotional support needed to navigate the transplant journey.
The Surgical Procedure of Lung Transplantation
Lung transplantation surgery is a complex process. It involves several critical steps, from the procurement of donor lungs to the immediate post-surgical care of the recipient.
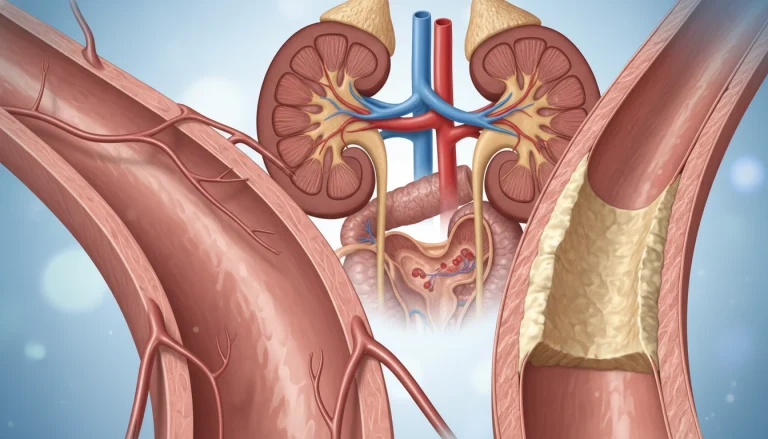
Donor Organ Procurement and Preservation
The process starts with the procurement of donor lungs. These lungs are carefully evaluated to ensure they are suitable for transplantation. This evaluation includes assessing the lungs’ function, checking for any infections or diseases, and matching the donor’s blood type and lung size to the recipient.
- Donor lungs are evaluated through a series of tests, including chest X-rays and blood gas analysis.
- Preservation techniques, such as cooling the lungs to a low temperature, are used to maintain their viability.
- The donor lungs are then transported to the recipient’s hospital, where they are prepared for transplantation.
The Transplant Operation
The transplant operation involves replacing the diseased lung(s) with the donor lung(s). This requires precise surgical technique and careful patient management to ensure a successful outcome.

The surgical team must be highly skilled and experienced in performing lung transplantation surgery. The operation can be performed as a single lung transplant or a bilateral lung transplant, depending on the recipient’s condition.
- The recipient is given general anesthesia to ensure they remain pain-free during the operation.
- The surgical team makes an incision in the chest to access the lungs.
- The diseased lung(s) are removed and replaced with the donor lung(s), which are then connected to the recipient’s airways and blood vessels.
Immediate Post-Surgical Care
Immediate post-surgical care is critical to ensure the patient’s stability and monitor for any complications. The recipient is closely monitored in the intensive care unit (ICU) for signs of rejection or other issues.
- The recipient is given immunosuppressive medications to prevent rejection.
- Close monitoring of the recipient’s vital signs and lung function is performed.
- Any complications, such as bleeding or infection, are promptly addressed.
Recovery and Rehabilitation
Recovery and rehabilitation are key after a lung transplant. This period is essential for patients to regain strength and adjust to their new lungs. It also helps them return to their usual activities.
Hospital Recovery Phase
In the hospital, patients are watched closely for any issues or rejection signs. The medical team manages pain and adjusts medications as needed. They also provide respiratory therapy to ease breathing.
Early Outpatient Management
After leaving the hospital, patients start the early outpatient phase. Here, they receive ongoing care from their transplant team. This includes regular check-ups, medication adjustments, and monitoring for complications.
Physical Therapy and Exercise Protocols
Physical therapy and exercise are vital for recovery. They help patients regain strength, improve lung function, and boost overall health. A personalized exercise plan is recommended, covering aerobic exercises, strength training, and flexibility.
Returning to Normal Activities
As recovery advances, patients can slowly return to their normal lives. This includes going back to work, social events, and hobbies. It’s important to follow their healthcare team’s advice for a safe and successful transition.
Immunosuppression and Medication Management
The success of lung transplantation heavily relies on immunosuppression and careful medication management. Immunosuppression is a critical component of post-transplant care. It prevents the body’s immune system from rejecting the transplanted lung.
Induction Therapy
Induction therapy is administered at the time of transplantation to reduce the risk of acute rejection. This initial immunosuppressive regimen typically involves potent immunosuppressive agents. These include monoclonal antibodies or polyclonal antibodies, to deplete or modulate the immune cells.
Maintenance Immunosuppression
Following induction therapy, maintenance immunosuppression is critical for long-term graft survival. This involves a combination of immunosuppressive medications. These often include calcineurin inhibitors, antiproliferative agents, and corticosteroids, tailored to the individual patient’s needs and response.

Side Effects and Complications
While immunosuppressive therapy is essential, it is not without risks. Common side effects and complications include nephrotoxicity, hypertension, hyperlipidemia, and an increased susceptibility to infections. Monitoring and managing these side effects is critical to maintaining the patient’s quality of life.
Medication Adherence Strategies
Adherence to the prescribed immunosuppressive regimen is vital for preventing rejection and ensuring graft longevity. Strategies to enhance medication adherence include patient education, simplification of the medication regimen, and regular follow-up appointments with the healthcare team.
Effective immunosuppression and medication management require a multidisciplinary approach. This involves transplant pulmonologists, surgeons, pharmacists, and other healthcare professionals. By carefully balancing the benefits and risks of immunosuppressive therapy, patients can achieve optimal outcomes after lung transplantation.
Monitoring and Managing Complications
Complications after lung transplantation are significant, requiring constant monitoring and effective management. Patients face various risks that can affect the procedure’s success and their quality of life.
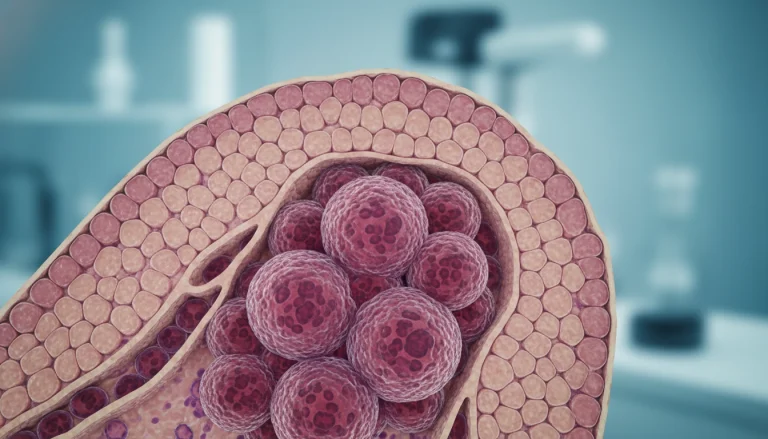
Acute and Chronic Rejection
Acute rejection is a major complication in the early stages post-transplant. It involves an immune response against the lung, causing inflammation and damage. Chronic rejection, or bronchiolitis obliterans syndrome (BOS), leads to a gradual decline in lung function over time.
It’s critical to monitor for rejection signs. Treatment usually involves immunosuppressive drugs to dampen the immune response.
Infection Prevention and Treatment
Infections are a significant risk due to the patient’s immunosuppressed state. Preventive measures include prophylactic antibiotics and antiviral medications. Patients should also avoid exposure to infection sources.
When infections occur, prompt treatment with the right antimicrobial therapy is key to preventing severe complications.
Long-term Complications
Long-term complications include BOS and other issues like osteoporosis, diabetes, and kidney dysfunction. Regular monitoring and management are essential to keep lung transplant recipients healthy.
Warning Signs to Report
Patients are taught to recognize warning signs to report to their healthcare provider. These include shortness of breath, fever, and lung function changes. Reporting these symptoms early can lead to timely intervention and prevent severe complications.
Outcomes and Quality of Life After Lung Transplantation
Lung transplantation outcomes have seen significant advancements, leading to better survival and quality of life for recipients. These improvements are due to better surgical techniques, more effective immunosuppressive therapies, and enhanced post-transplant care.
Survival Statistics
Recent data show a notable increase in survival rates post-lung transplant. The one-year survival rate is now about 80%, and the five-year rate is around 50%. These figures highlight a positive trend in the long-term success of lung transplant patients.
Functional Improvements
Lung transplantation brings about significant functional enhancements. Patients often see better lung function and exercise capacity. This allows them to resume normal activities and significantly improve their quality of life. 
Psychological Adjustment and Well-being
Psychological adjustment is a key part of post-transplant care. Many patients report enhanced emotional well-being and a higher quality of life. Yet, the psychological effects of transplantation can vary. Ongoing support is vital to address any mental health issues.
In summary, lung transplantation outcomes have greatly improved. There are encouraging survival statistics, significant functional enhancements, and positive psychological adjustments for many patients.
Conclusion
Lung transplantation is a complex and life-saving procedure that offers hope to patients with end-stage lung disease. The journey to transplantation involves a thorough evaluation, careful patient selection, and meticulous post-operative care. Understanding the various aspects of lung transplantation helps patients and their families navigate this complex process.
Advancements in surgical techniques, immunosuppressive medications, and post-operative care have improved outcomes for lung transplant recipients. This offers a brighter future for those affected by lung disease. For more information on organ transplantation, visit Acibadem International. They provide valuable insights into various transplantation procedures.
In conclusion, lung transplantation is a viable treatment option for patients with severe lung disease. Its success relies on a multidisciplinary approach. As medical technology and techniques continue to evolve, the prospects for lung transplant patients are becoming increasingly promising.
FAQ
Q: What is the primary purpose of lung transplantation?
A: Lung transplantation aims to restore lung function in those with severe lung disease. It improves their quality of life and survival chances.
Q: What conditions are typically considered for lung transplantation?
A: Conditions like Chronic Obstructive Pulmonary Disease (COPD), Idiopathic Pulmonary Fibrosis (IPF), and Cystic Fibrosis (CF) are considered. Also, pulmonary hypertension, bronchiolitis obliterans, and lymphangioleiomyomatosis are considered.
Q: What are the different types of lung transplant procedures?
A: There are several types of lung transplant procedures. These include Single Lung Transplantation, Bilateral Lung Transplantation, Heart-Lung Transplantation, and Living Donor Lobar Transplantation.
Q: How are candidates selected for lung transplantation?
A: Candidates undergo a thorough evaluation. This includes assessing their medical suitability, psychological stability, and social support.
Q: What is the Lung Allocation Score (LAS) and how is it used?
A: The Lung Allocation Score (LAS) ranks candidates for lung transplantation. It considers their likelihood of benefiting from the transplant, based on lung function, diagnosis, and waiting time.
Q: What is involved in preparing for lung transplantation?
A: Preparing for lung transplantation involves several steps. These include pulmonary rehabilitation, nutritional optimization, and mental preparation and support systems.
Q: What are the key components of post-transplant care?
A: Post-transplant care includes managing immunosuppression and medications. It also involves monitoring and managing complications, and ongoing follow-up with the transplant team.
Q: What are the possible complications after lung transplantation?
A: Complications can include acute and chronic rejection, infections, and long-term issues like bronchiolitis obliterans syndrome. Side effects of immunosuppressive medications are also possible.
Q: What are the outcomes and quality of life after lung transplantation?
A: Lung transplantation outcomes have significantly improved. Survival statistics are encouraging, with functional improvements and better psychological adjustment and well-being.