Migraine: Common Migraine Triggers and Risk Factors
A migraine is a neurological condition marked by intense, debilitating headaches. These headaches are often accompanied by nausea, vomiting, and sensitivity to light and sound. The exact causes of migraines are not fully understood. They are believed to involve a combination of genetic, environmental, and hormonal factors.
Common symptoms include severe headache, aura, and sensitivity to light and sound. Various treatment options are available. These include medications, lifestyle changes, and alternative therapies. Understanding migraines is key to effective management and treatment. By exploring the causes, symptoms, and treatment options, individuals can better cope with this complex condition.
What Makes Migraines Different from Regular Headaches
Migraines are often seen as just severe headaches, but they have unique characteristics. It’s important to understand these differences for accurate diagnosis and treatment.
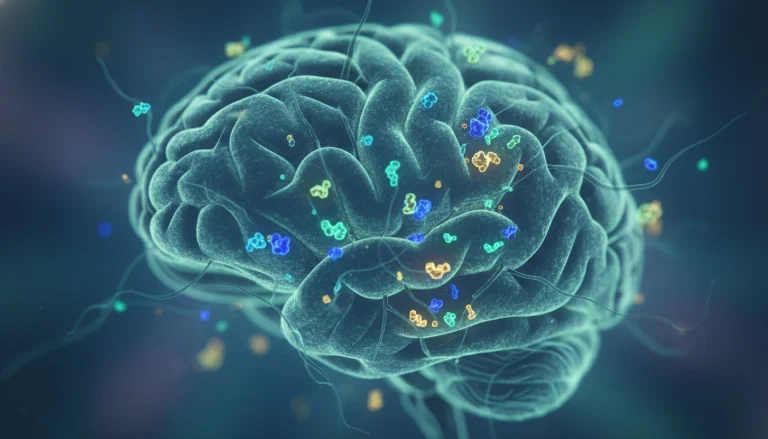
Neurological Basis of Migraine Pain
Migraine pain is more than just a headache; it’s a complex neurological condition. The pain is usually one-sided and can be accompanied by nausea, vomiting, and sensitivity to light and sound. Research indicates that migraines involve abnormal brain activity, affecting nerve signals, chemicals, and blood vessels.
The neurological basis of migraine pain involves the activation of the trigeminal nerve. This nerve releases neurotransmitters and causes blood vessels to swell. This process leads to the release of pain-producing chemicals, resulting in the throbbing pain associated with migraines.
Debunking Common Migraine Misconceptions
One common misconception is that migraines are just a type of headache. Yet, migraines are a specific neurological disorder with symptoms beyond headache pain. Another misconception is that migraines are triggered solely by stress or certain foods. In reality, triggers can vary widely among individuals.
By understanding the neurological basis of migraine pain and dispelling common misconceptions, individuals can better manage their condition. They can also seek appropriate medical care when needed.
The Prevalence and Impact of Migraines
Understanding migraines is key to tackling this debilitating condition. Migraines are more than just severe headaches; they are a complex neurological disorder. They affect millions globally, disrupting daily life and productivity significantly.
Statistical Overview in the United States
In the United States, migraines are a major issue, impacting about 39 million people. The American Migraine Foundation reports that nearly 1 in 4 U.S. households has someone with migraines. This leads to a huge economic burden from lost productivity, healthcare costs, and reduced quality of life.
Demographics and Populations Most Affected
Migraines impact various demographics, but some are more at risk. Women are three times more likely than men to suffer from migraines. The condition peaks among those aged 30 to 49. Those with a family history of migraines are also at higher risk. Socioeconomic status and geographic location can further influence who gets migraines.
Types of Migraine
Migraines are not a one-size-fits-all condition; they come in various forms, each with distinct characteristics. Understanding these differences is key to managing and treating migraines effectively.
Migraine With Aura
A migraine with aura is characterized by neurological symptoms that appear before the headache. These symptoms can include visual disturbances, such as seeing flashes of light or zigzag patterns, and sensory changes, like numbness or tingling. The aura phase can last from a few minutes to an hour and is usually followed by the headache phase.
Migraine Without Aura
Migraine without aura, also known as common migraine, is the most prevalent type. It involves migraine headache pain without the preceding neurological symptoms. The headache can be severe and is often accompanied by other symptoms like nausea and sensitivity to light and sound.
Chronic and Episodic Migraines
Migraines can also be classified based on their frequency. Episodic migraines occur irregularly, with periods of remission in between attacks. Chronic migraines, on the other hand, occur more frequently, often 15 days or more per month over a three-month period. Chronic migraines can be more debilitating and require a more complex treatment plan.
Recognizing the type of migraine is critical for selecting the appropriate treatment strategy. Whether it’s a migraine with aura, without aura, or chronic and episodic, understanding the specific characteristics can help in managing symptoms more effectively.
The Four Distinct Phases of a Migraine Attack
Understanding the progression of a migraine is key to effective management. A migraine attack is a complex neurological event that unfolds in stages. Each stage has its own set of symptoms and characteristics.
Prodrome Phase: Early Warning Signs
The prodrome phase, experienced by up to 80% of people with migraines, can start hours or even days before the headache. Symptoms include mood changes, fatigue, and increased sensitivity to light and sound.
Aura Phase: Neurological Disturbances
Not everyone experiences an aura, but for those who do, it typically occurs before the headache. It can include visual disturbances, such as flashing lights or blind spots, and sometimes sensory or motor symptoms.

Headache Phase: Peak Pain and Symptoms
This is the most debilitating phase, characterized by intense headache pain. It is often accompanied by nausea, vomiting, and heightened sensitivity to environmental stimuli.
Postdrome Phase: The Migraine Hangover
After the headache has resolved, some people enter a postdrome phase. They feel drained, exhausted, and sometimes experience mood changes or cognitive difficulties.
Recognizing these phases can help individuals prepare for and potentially mitigate the impact of a migraine attack.
Recognizing Migraine Symptoms
Migraines are complex, involving a variety of physical and neurological symptoms. It’s critical to recognize these symptoms for effective management and treatment. Symptoms can vary greatly among individuals, making it key to understand the different types that may occur.
Primary Physical Symptoms
Primary physical symptoms include headache pain, often described as throbbing or pulsating. Other symptoms may include nausea, vomiting, and sensitivity to light and sound. Some people may also feel fatigue, dizziness, or muscle weakness.
Neurological and Sensory Symptoms
Neurological and sensory symptoms are common in migraines. These can include aura symptoms like visual disturbances (e.g., flashing lights, blind spots) and sensory changes (e.g., numbness, tingling). Difficulty speaking is also a symptom. Some individuals may experience neurological symptoms without headache pain, known as a silent migraine.
Understanding the range of migraine symptoms, both physical and neurological, is vital for proper diagnosis and treatment. Recognizing these symptoms helps individuals seek medical attention and develop effective management strategies.
Common Migraine Triggers and Risk Factors
The onset of a migraine can often be attributed to specific triggers, which can be broadly categorized into several types. Understanding these triggers is essential for individuals to manage and potentially reduce the frequency of their migraines.
Environmental Triggers
Environmental factors play a significant role in triggering migraines. Common environmental triggers include bright or flickering lights, loud noises, and strong smells. Changes in weather or altitude can also trigger migraines in some individuals.
Dietary and Consumption Triggers
Dietary habits and certain foods can trigger migraines. Common culprits include aged cheeses, processed meats, and foods containing MSG or tyramine. Caffeine and alcohol can also act as triggers for some people.
Stress and Sleep-Related Triggers
Stress is a well-known migraine trigger. Changes in sleep patterns, such as oversleeping or undersleeping, can also trigger migraines. Stress management techniques and maintaining a consistent sleep schedule can help mitigate these triggers.
Hormonal and Genetic Predispositions
Hormonal fluctuations, such as changes in estrogen levels, can trigger migraines in some individuals. Genetic predisposition also plays a role, with individuals having a family history of migraines being more likely to experience them.
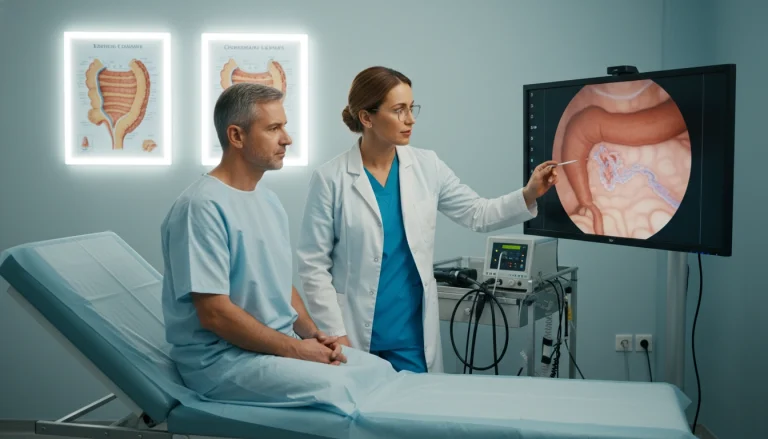
How Migraines Are Diagnosed
The process of diagnosing migraines involves a detailed medical history, physical examination, and adherence to specific diagnostic criteria. Accurate diagnosis is key for effective management and treatment.
Medical History and Physical Examination
Understanding a patient’s medical history is critical in diagnosing migraines. Healthcare professionals will inquire about the frequency, duration, and characteristics of headache episodes. They also ask about any associated symptoms, such as nausea or sensitivity to light. A physical examination is conducted to rule out other headache causes.
The physical examination may include a neurological examination to check for any abnormalities in brain function. This thorough assessment aids healthcare providers in understanding the patient’s condition.
Diagnostic Tests and Clinical Criteria
Though there are no specific tests for migraines, diagnostic tests like MRI or CT scans may be used to rule out other causes. The diagnosis of migraines is mainly based on clinical criteria, including headache characteristics and associated symptoms.
Healthcare professionals rely on guidelines from the International Headache Society for diagnosing migraines. These guidelines outline specific criteria that must be met for a migraine diagnosis.
Prescription Medications for Acute Migraine Relief
Prescription medications are key in managing acute migraine attacks, providing much-needed relief. These medications are designed to alleviate symptoms and reduce the severity of migraine episodes.
The range of prescription medications available for acute migraine relief includes several classes of drugs. Each class has its unique mechanism of action and benefits.
Triptans and Ergotamines
Triptans work by constricting blood vessels and blocking pain pathways in the brain. They are available in various forms, including oral tablets, nasal sprays, and injections. Ergotamines, another older class of migraine medications, also constrict blood vessels but are less commonly used today. This is due to their side effects and the availability of more effective and safer alternatives like triptans.
Anti-Nausea and Pain Medications
In addition to triptans and ergotamines, anti-nausea medications and pain relievers are often prescribed. These medications help manage associated symptoms of migraines. Anti-nausea medications alleviate nausea and vomiting, while pain relievers reduce headache pain.
New Acute Treatments: Gepants and Ditans
Recently, newer classes of medications have been developed for acute migraine treatment. Gepants work by blocking the calcitonin gene-related peptide (CGRP) receptor, involved in migraine pain transmission. Ditans, similar to triptans, target serotonin receptors but with a different mechanism. This offers an alternative for those who do not respond to triptans.
It’s essential for patients to work closely with their healthcare provider. This is to determine the most appropriate treatment plan. Individual responses to these medications can vary.

Preventive Medication Strategies
Understanding preventive medication options is key to managing migraine frequency and severity. These medications are designed to reduce migraine occurrence. They are recommended for those experiencing frequent or severe attacks.
Traditional Preventive Medications
Traditional preventive medications include various drug classes. These include beta-blockers, anticonvulsants, and antidepressants. They have been used for years to manage migraines by reducing their frequency and severity.
For example, beta-blockers like propranolol are commonly prescribed for migraine prevention.
CGRP Monoclonal Antibodies
CGRP monoclonal antibodies represent a newer class of preventive medications. They target the calcitonin gene-related peptide (CGRP) pathway, believed to play a significant role in migraine development. Medications such as erenumab and fremanezumab have shown efficacy in reducing migraine frequency.
Botox and Other Injectable Treatments
Botox (onabotulinumtoxinA) is an injectable treatment approved for chronic migraine prevention. It is administered every 12 weeks and has been shown to reduce migraine frequency. Other injectable treatments may also be considered based on individual patient needs.
By understanding these preventive medication strategies, individuals suffering from migraines can work with their healthcare providers. Together, they can develop a personalized treatment plan. This plan aims to reduce the impact of migraines on daily life.
Over-the-Counter Options for Migraine Management
Migraine management often starts with over-the-counter options. These treatments provide relief without a prescription. They are effective for those with mild to moderate symptoms.
NSAIDs and Their Effectiveness
Nonsteroidal anti-inflammatory drugs (NSAIDs) are a popular choice for managing migraine pain. They reduce inflammation and block pain pathways in the brain. Examples include ibuprofen (Advil, Motrin) and naproxen (Aleve). These are available over-the-counter and can be taken at the onset of symptoms.
Studies have shown NSAIDs to be effective in treating migraines. They significantly reduce pain and improve quality of life for sufferers.
Combination Medications and Supplements
Combination medications and supplements also aid in migraine management. These products mix pain relievers like acetaminophen, aspirin, and caffeine. Excedrin Migraine is an example, combining these to target migraine pain and symptoms.
Some people find relief in supplements like magnesium, feverfew, and riboflavin (B2). These have been studied for their ability to reduce migraine frequency and severity.
Non-Pharmacological Treatment Approaches
Non-pharmacological methods offer a promising way to manage migraines without medication. These approaches focus on treating migraines through alternative techniques, avoiding pharmaceuticals.
The following non-pharmacological treatments have shown promise in reducing migraine symptoms:
Neuromodulation Devices
Neuromodulation devices aim to stimulate the nervous system to prevent or alleviate migraine pain. Examples include transcutaneous supraorbital nerve stimulation (tSNS) and non-invasive vagus nerve stimulation (nVNS).
Biofeedback and Relaxation Techniques
Biofeedback trains patients to recognize and control physiological responses to stress, which can trigger migraines. Techniques include relaxation training, thermal biofeedback, and electromyographic biofeedback.
Acupuncture and Manual Therapies
Acupuncture involves inserting thin needles into specific points on the body to stimulate healing and pain relief. Manual therapies, such as massage and physical therapy, can also help reduce migraine frequency and severity.
Cognitive Behavioral Therapy for Migraine
Cognitive behavioral therapy (CBT) is a psychological approach that helps patients identify and change negative thought patterns and behaviors that may contribute to migraines. CBT can be used in conjunction with other treatments to enhance their effectiveness.
Some benefits of non-pharmacological approaches include:
- Reduced reliance on medication
- Potential for fewer side effects
- Holistic approach to health and wellness
- Can be used in conjunction with traditional treatments
By incorporating these non-pharmacological methods into a treatment plan, individuals with migraines may see improved symptom management and quality of life.
Lifestyle Modifications for Migraine Prevention
Making simple changes in your daily life can greatly help in managing and preventing migraines. By adjusting your routine, you can significantly lessen the number and intensity of migraine attacks.
Sleep Hygiene and Regulation
Keeping a regular sleep schedule is key to preventing migraines. This means going to bed and waking up at the same time each day, including weekends. A cool, dark, and quiet bedroom environment can also enhance sleep quality. It’s wise to avoid caffeine and electronic devices before bedtime.
Stress Management Techniques
Stress is a major migraine trigger, making stress management vital. Techniques like meditation, deep breathing, and yoga can help lower stress levels. Regular exercise and a balanced work-life schedule are also important for stress management.
Exercise, Hydration, and Routine
Regular physical activity, such as walking or swimming, can reduce migraine frequency by boosting health and lowering stress. Drinking plenty of water daily is also essential, as dehydration often triggers migraines. A consistent daily routine that includes relaxation and leisure can also help prevent migraines.

Dietary Approaches to Reduce Migraine Frequency
Changing your diet can be a key step in managing migraines. Understanding how different foods affect you can help you make better choices. This can lead to fewer migraine attacks.
Common Food Triggers to Avoid
Some foods can trigger migraines in certain people. Aged cheeses, processed meats, and foods with artificial additives are common culprits.
- Aged cheeses like cheddar and parmesan
- Processed meats such as bacon and salami
- Foods with artificial sweeteners and preservatives
Anti-Inflammatory and Migraine-Friendly Diets
An anti-inflammatory diet can help reduce migraine symptoms. It should include lots of fruits, vegetables, and omega-3 fatty acids. Foods high in antioxidants and fiber are also beneficial.
Adding foods like leafy greens, berries, and fatty fish to your diet can improve your overall health. It may also help reduce the number of migraines you experience.
Tracking and Managing Your Migraine Patterns
Understanding and managing migraine patterns is key to reducing their frequency and impact. By tracking when migraines occur and identifying triggers, individuals can craft a more effective management plan.
Migraine Diaries and Digital Tracking Tools
Migraine diaries and digital tracking tools are essential for monitoring patterns. These tools help record the date, time, and severity of each migraine. They also track possible triggers like food, stress, or environmental factors.
- Migraine diary apps like Migraine Buddy or DayCounter enable users to track migraines and identify patterns.
- Digital tools can also provide reminders to take medication and offer insights into migraine triggers.
- Some apps integrate with wearable devices, providing additional data on physiological responses during a migraine.
Identifying and Addressing Personal Triggers
Once data is collected through tracking, the next step is to identify personal triggers. Common triggers include certain foods, hormonal changes, and stress. Understanding what triggers migraines allows individuals to take steps to avoid or mitigate these factors.
Some strategies for addressing personal triggers include:
- Avoiding trigger foods or substances.
- Practicing stress-reduction techniques such as meditation or yoga.
- Maintaining a consistent sleep schedule.
When to Seek Immediate Medical Attention
Recognizing the signs of a migraine emergency is critical. While most migraines are not urgent, some symptoms may indicate a serious condition. It’s vital to know when to seek immediate medical help.
Red Flags and Warning Signs
Some migraine symptoms are red flags, signaling a possible medical emergency. These include:
- Sudden, severe headache
- Confusion or difficulty speaking
- Weakness or numbness in the face or extremities
- Vision changes, such as double vision or loss of vision
Finding the Right Headache Specialist
If you’re dealing with frequent or severe migraines, finding a headache specialist is key. Seek a doctor with a proven track record in migraine treatment. Ask about their methods and success rates to ensure you’re in good hands.
Creating Your Personalized Migraine Management Plan
Creating a tailored approach to managing migraines is essential for effective relief. By using insights from previous sections, individuals can craft a migraine management plan that meets their unique needs.
A personalized plan requires identifying and avoiding triggers. It also involves adopting lifestyle modifications and using appropriate treatments. This includes dietary changes and stress management techniques.
To begin, review common migraine triggers and risk factors. Consider various treatment options, such as prescription medications and non-pharmacological approaches. This will help in developing a well-rounded plan.
By combining this knowledge and tracking individual migraine patterns, a flexible plan can be created. This plan allows for adjustments as needed to ensure optimal migraine management.
In the end, a well-crafted migraine management plan empowers individuals. It helps them take control of their condition. This reduces the frequency and severity of migraine attacks, improving overall quality of life.
FAQ
Q: What is a migraine?
A: A migraine is a neurological condition marked by intense, debilitating headaches. These headaches are often accompanied by nausea, vomiting, and sensitivity to light and sound.
Q: What are the different types of migraines?
A: There are several types of migraines. These include migraines with aura, migraines without aura, chronic migraines, and episodic migraines.
Q: What are the symptoms of a migraine?
A: Symptoms of a migraine can include headache pain, nausea, vomiting, and sensitivity to light and sound. They can also include neurological disturbances such as aura.
Q: What triggers migraines?
A: Common migraine triggers include environmental factors, dietary factors, stress, hormonal changes, and genetic predispositions.
Q: How are migraines diagnosed?
A: Migraines are diagnosed based on medical history, physical examination, and diagnostic tests. They are also diagnosed based on clinical criteria, such as those outlined in the International Classification of Headache Disorders.
Q: What are the treatment options for migraines?
A: Treatment options for migraines include prescription medications, over-the-counter medications, non-pharmacological approaches, and lifestyle modifications.
Q: Can migraines be prevented?
A: Yes, migraines can be prevented. This can be done through preventive medications, lifestyle changes, and avoiding triggers.
Q: What are some common preventive medications for migraines?
A: Common preventive medications for migraines include traditional medications, CGRP monoclonal antibodies, and Botox.
Q: How can I track and manage my migraines?
A: You can track and manage your migraines using a migraine diary or digital tracking tool. Identifying and addressing personal triggers is also important. Working with a healthcare professional to develop a personalized management plan is key.
Q: When should I seek immediate medical attention for a migraine?
A: Seek immediate medical attention if you experience severe or unusual migraine symptoms. This includes a sudden severe headache, confusion, or weakness.