Minimally Invasive Trauma Surgery: What is Minimally Invasive Trauma Surgery?
Modern medicine has seen major leaps forward, with Minimally Invasive Trauma Surgery playing a key role. This method has changed how surgeons work, bringing benefits like shorter recovery times and less scarring. Minimally Invasive Trauma Surgery stands out for its ability to treat effectively with less risk of complications. As technology advances, its role is expected to grow. This will open up new avenues for both patients and medical professionals.
The Science Behind Minimally Invasive Trauma Surgery
Grasping the science behind Minimally Invasive Trauma Surgery is key to its success. This method has revolutionized surgery, cutting down on tissue damage and speeding up recovery. It’s a game-changer in the field of trauma surgery.
Definition and Basic Principles
Minimally Invasive Trauma Surgery involves making smaller incisions to reduce tissue disruption. It relies on precise planning, specialized tools, and advanced imaging to guide the surgery. These steps help surgeons minimize the trauma of traditional open surgery.
Anatomical Considerations
Anatomical knowledge is vital for Minimally Invasive Trauma Surgery. Surgeons need to understand the patient’s anatomy to navigate the procedure’s complexities. For example, cervical, thoracic, and lumbar laminectomy require deep knowledge of spinal anatomy to prevent complications.
Advanced imaging and navigation technologies enhance the surgeon’s ability to work with the patient’s anatomy. This improves the procedure’s safety and effectiveness.
Historical Development of Minimally Invasive Approaches
Minimally Invasive Trauma Surgery has seen significant growth, driven by technological and surgical advancements. This evolution has reshaped trauma care, providing patients with less invasive options compared to traditional open surgery.
Evolution from Open Surgery
The transition from open surgery to minimally invasive methods aimed to reduce patient trauma, blood loss, and recovery time. Important milestones include:
- The introduction of laparoscopic surgery in the late 20th century
- Advances in imaging technologies, such as fluoroscopy and ultrasound
- Development of specialized instruments and equipment for minimally invasive procedures
Technological Breakthroughs
Technological advancements have been key in the growth of Minimally Invasive Trauma Surgery. Notable breakthroughs include:
- High-definition imaging systems for improved visualization
- Robotic surgical systems that enhance precision and dexterity
- Advanced energy devices for effective hemostasis and tissue sealing
These innovations have significantly enhanced the outcomes of minimally invasive trauma surgery. They have also broadened its applications, making it a viable option for more trauma cases.
Types of Trauma Amenable to Minimally Invasive Techniques
Minimally invasive surgery in trauma care is becoming more widespread. It’s used for treating different trauma types, leading to faster recovery and fewer complications. This approach is a game-changer in trauma treatment.
Blunt Abdominal Trauma
Blunt abdominal trauma often results from car accidents, falls, or assaults. Laparoscopy, a minimally invasive method, is used to diagnose and treat abdominal organ injuries. It reduces the need for big incisions, minimizing tissue damage and speeding up healing.
Penetrating Injuries
Penetrating injuries, from gunshots or stabbings, can be managed with minimally invasive methods. Thoracoscopy and laparoscopy help assess and repair internal organ damage. These methods lower the risks of traditional open surgery.
Orthopedic Trauma Applications
Orthopedic trauma, like fractures and soft tissue injuries, benefits from minimally invasive surgery. Techniques like percutaneous fixation and arthroscopy allow for stabilizing fractures and repairing soft tissues with minimal disruption. This leads to quicker recovery and less pain post-surgery.
In summary, minimally invasive techniques are versatile in trauma care, applicable to blunt abdominal trauma, penetrating injuries, and orthopedic trauma. Their advantages include less tissue damage, reduced post-operative pain, and faster recovery times.
Essential Techniques in Minimally Invasive Trauma Surgery
Minimally invasive trauma surgery is revolutionizing patient care. It significantly reduces recovery time and minimizes surgical trauma. This approach is a game-changer in the field of surgery.
Laparoscopic Approaches
Laparoscopic surgery, also known as laparoscopy, involves small incisions. A camera and surgical instruments are inserted through these incisions to perform the operation. In trauma surgery, laparoscopic methods are used to diagnose and treat internal injuries. These injuries often involve the abdominal cavity.
- Reduced postoperative pain
- Shorter hospital stays
- Less postoperative complications
Thoracoscopic Interventions
Thoracoscopic interventions use a thoracoscope to visualize the thoracic cavity. This technique is invaluable in managing thoracic trauma. It allows surgeons to inspect the lungs, diaphragm, and other structures within the chest.

Thoracoscopy is used to evacuate hemothorax, repair diaphragmatic injuries, and control bleeding within the thoracic cavity. It’s a precise method for addressing these critical issues.
Endovascular Procedures
Endovascular procedures involve minimally invasive techniques. Surgeons use catheters and other instruments inserted through blood vessels to treat vascular injuries. This approach is highly effective in managing bleeding that’s hard to control through open surgery.
- Control of hemorrhage
- Repair of vascular injuries
- Minimally invasive approach reduces recovery time
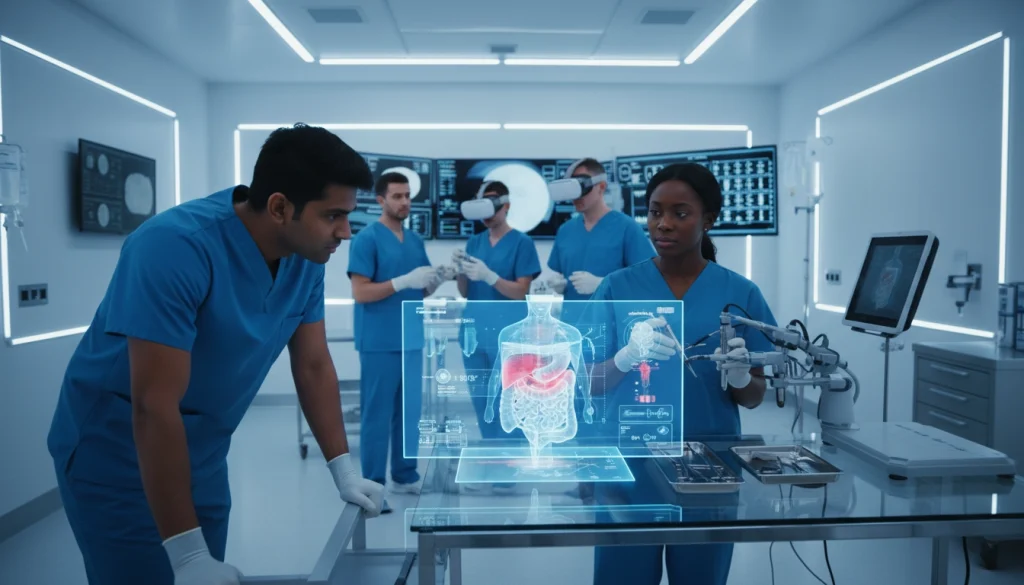
Advanced Imaging and Navigation Technologies
The integration of advanced imaging technologies has transformed minimally invasive trauma surgery. These innovations have greatly enhanced surgical precision and patient outcomes. They provide real-time data and improved visualization.
Intraoperative Imaging Systems
Intraoperative imaging systems enable surgeons to see the surgical site in real-time. This allows for more accurate and precise interventions. These systems are invaluable in complex trauma cases where anatomy may be distorted or damaged.
- Provide real-time feedback to surgeons
- Enhance visualization of critical structures
- Improve accuracy of surgical interventions
3D Visualization Tools
3D visualization tools give surgeons a detailed view of the patient’s anatomy. This facilitates more precise surgical planning and execution. They are highly beneficial in complex fracture or vascular injury cases.
- Enable detailed preoperative planning
- Enhance intraoperative navigation
- Improve overall surgical precision
Augmented Reality Applications
Augmented reality (AR) applications are becoming a powerful tool in minimally invasive trauma surgery. AR overlays digital information onto the real-world surgical site. This provides surgeons with critical information in real-time.
- Overlay digital information onto the surgical site
- Provide real-time data to surgeons
- Enhance surgical precision and outcomes
The combination of these advanced imaging and navigation technologies is revolutionizing minimally invasive trauma surgery. It offers improved patient outcomes and shorter recovery times.
Specialized Equipment and Instrumentation
Minimally invasive trauma surgery relies on a variety of specialized tools to achieve the best results. The success of these procedures heavily depends on the availability and correct use of advanced surgical equipment.
Endoscopic Instruments
Endoscopic instruments are essential in minimally invasive trauma surgery. They enable surgeons to see and work inside the body through small cuts. These tools include:
- High-definition cameras for clear visualization
- Specialized graspers and dissectors for tissue manipulation
- Electrocautery devices for hemostasis
Robotic Surgical Systems
Robotic surgical systems enhance precision and dexterity, making complex procedures easier. They offer:
- Improved visualization with 3D imaging
- Enhanced ergonomics for surgeons, reducing fatigue
- Increased precision in dissection and suturing
Energy Devices and Sealants
Energy devices and sealants are key for achieving hemostasis and tissue sealing in minimally invasive trauma surgery. Examples include:
- Electrocautery devices for cutting and coagulation
- Laser devices for precise tissue dissection
- Hemostatic agents for controlling bleeding
The use of these specialized tools in minimally invasive trauma surgery has greatly improved patient outcomes. It has reduced recovery times and enhanced the quality of care.
Patient Selection and Evaluation
Minimally invasive trauma surgery demands a careful patient evaluation to achieve the best results. This involves finding the right candidates, identifying who should not undergo the procedure, and conducting detailed preoperative assessments.
Ideal Candidates
Ideal candidates for minimally invasive trauma surgery are those whose injuries or conditions can be effectively managed through these techniques. They typically have:
- Stable vital signs
- Specific types of injuries (e.g., certain blunt or penetrating traumas)
- No significant previous abdominal surgery
These patients are considered ideal because their conditions align well with the benefits of minimally invasive procedures.
Contraindications
Contraindications for minimally invasive trauma surgery include conditions that pose risks or diminish the procedure’s benefits. These include:
- Severe hemodynamic instability
- Known extensive adhesions from previous surgeries
- Certain types of injuries that require immediate open surgery
Identifying these contraindications is vital to prevent complications and ensure patients receive the best care possible.
Preoperative Assessment Protocols
Preoperative assessment protocols for minimally invasive trauma surgery involve a thorough evaluation of the patient’s condition. This includes:
- Detailed medical history
- Imaging studies (e.g., CT scans, X-rays)
- Laboratory tests
These evaluations help in planning the surgical approach, anticipating challenges, and improving patient outcomes.
The Multidisciplinary Trauma Team Approach
Minimally invasive trauma surgery demands a team effort from a wide range of healthcare experts. This strategy guarantees patients get all-around care, from the first check-up to healing after surgery.
Team Composition and Roles
The team usually consists of trauma surgeons, anesthesiologists, radiologists, nurses, and other support staff. Each team member is essential:
- Trauma surgeons carry out the surgeries.
- Anesthesiologists manage pain and vital signs during the procedure.
- Radiologists offer diagnostic images to help make surgical decisions.
- Nurses assist during surgery and care for patients afterward.
This diverse team collaborates to enhance patient results.
Communication and Coordination
Good communication and teamwork are key to the team’s success. Strategies include:
- Pre-operative meetings to discuss patient status and surgical plans.
- Intra-operative updates to handle any issues.
- Post-operative reviews to discuss outcomes and areas for betterment.
Through seamless teamwork, the team can reduce complications and boost patient recovery.

Benefits of Minimally Invasive Trauma Surgery
Minimally invasive trauma surgery has transformed trauma care, bringing significant advantages to patients. This method reduces surgical trauma, minimizes complications, and speeds up recovery. It has been shown to improve patient outcomes dramatically.
Reduced Surgical Trauma and Blood Loss
This approach offers a major benefit: less surgical trauma and blood loss. Smaller incisions and precise techniques reduce tissue damage and bleeding risks. This results in:
- Less post-operative pain
- Reduced need for blood transfusions
- Lower risk of infection
Decreased Hospital Stay and Recovery Time
Minimally invasive trauma surgery also leads to faster recovery and shorter hospital stays. Patients experience less tissue damage and trauma. This means:
- Quicker return to normal activities
- Reduced risk of complications
- Lower healthcare costs due to shorter hospital stays
Improved Cosmetic Outcomes
Another benefit is improved cosmetic outcomes. Smaller incisions result in less scarring, a significant advantage for patients. The benefits include:
- Less noticeable scars
- Improved patient satisfaction with the surgical outcome
- Enhanced overall appearance
Potential Complications and Risk Management
Understanding the complications of minimally invasive trauma surgery is key to managing risks. This approach offers many benefits but also presents unique challenges. Surgeons must navigate these challenges effectively.
Procedure-Specific Complications
Minimally invasive trauma surgery can lead to several specific complications. These include:
- Bleeding and hemorrhage due to the limited visibility and accessibility of the surgical site.
- Organ injury from the insertion of trocars or the manipulation of surgical instruments.
- Infection, which can occur if proper sterile techniques are not followed.
- Complications related to the creation of pneumoperitoneum, such as gas embolism or respiratory acidosis.
Surgeons must be aware of these complications and take steps to mitigate them. This includes using appropriate imaging techniques and maintaining a high level of situational awareness during the procedure.
Conversion to Open Surgery: When and Why
Deciding when to convert to open surgery is a critical decision in minimally invasive trauma surgery. This decision is typically made when:
- The patient’s condition becomes unstable, and more invasive monitoring or intervention is required.
- There is significant bleeding that cannot be controlled through minimally invasive means.
- The surgeon encounters anatomical complexities that make it difficult to safely proceed with the minimally invasive approach.
Conversion to open surgery is not a failure but a prudent decision to ensure the patient’s safety. Surgeons should be prepared to make this transition when necessary.
Post-Operative Care and Recovery
The success of minimally invasive trauma surgery heavily relies on thorough post-operative care and recovery strategies. Effective management during this critical period is essential. It minimizes complications, reduces recovery time, and improves patient outcomes.
Immediate Post-Surgical Management
Immediate post-surgical care involves close monitoring of the patient’s vital signs and overall condition. This includes managing any post-operative pain, monitoring for signs of infection or complications, and ensuring the patient is recovering as expected. Advanced monitoring systems and protocols are often employed to provide high-quality care.
Pain Control Strategies
Effective pain management is a critical component of post-operative care. Strategies may include the use of analgesic medications, regional anesthesia techniques, and non-pharmacological interventions such as breathing exercises and relaxation techniques. Personalized pain management plans are developed based on the patient’s specific needs and medical history.
Rehabilitation Protocols
Rehabilitation protocols are tailored to the individual patient’s needs and the type of surgery performed. These may include physical therapy, occupational therapy, and other interventions aimed at restoring function and promoting recovery. Early mobilization and rehabilitation can significantly improve outcomes by reducing the risk of complications and improving the patient’s quality of life.
Training Requirements for Trauma Surgeons
Effective training programs are essential for equipping trauma surgeons with the necessary skills for success in minimally invasive trauma surgery. These programs must be all-encompassing, covering both the theoretical and practical aspects of this complex field.
Educational Pathways
The educational journey for trauma surgeons involves a mix of formal education, clinical training, and ongoing professional development. They start with a solid base in general surgery, then move to specialized training in trauma surgery. This often includes fellowship programs that concentrate on minimally invasive methods.
Key components of these educational pathways include:
- Residency programs in general surgery
- Fellowship programs in trauma or surgical critical care
- Workshops and courses on minimally invasive surgery techniques
Simulation and Skills Development
Simulation is a critical part of trauma surgeon training, allowing them to refine their skills in a controlled setting. It includes virtual reality, synthetic models, and live animal models, each with its own advantages for skill enhancement.
Simulation-based training boosts surgeons’ proficiency in minimally invasive trauma surgery, leading to better patient outcomes. Continuous skills development is also vital, ensuring surgeons stay current with new techniques and technologies.
Clinical Outcomes and Evidence Base
A growing body of evidence supports the use of minimally invasive surgery in trauma care. It highlights its benefits over traditional methods. This evidence is key to understanding the clinical outcomes of minimally invasive trauma surgery.
Comparative Studies with Traditional Approaches
Many studies have compared minimally invasive trauma surgery with traditional open surgery. These studies show that minimally invasive techniques cause less tissue damage and blood loss. They also lead to fewer complications.
For example, a study in the Journal of Trauma and Acute Care Surgery found benefits. Patients who had laparoscopic surgery for abdominal trauma had shorter hospital stays and fewer complications than those with open surgery.
Long-Term Patient Outcomes
The long-term outcomes of minimally invasive trauma surgery are also important. Research shows these patients often have faster recovery times and less chronic pain. They also have better cosmetic outcomes than those treated traditionally.
A study in the Annals of Surgery found significant benefits. Patients who had minimally invasive trauma surgery had better functional outcomes and quality of life scores than those with conventional surgery.
Economic Considerations in Trauma Care
Healthcare costs are skyrocketing, making the economic aspects of trauma care more pressing. The financial impact on patients and healthcare systems is immense. It’s essential to assess the costs and benefits of various treatment methods.
Cost-Benefit Analysis
Conducting a thorough cost-benefit analysis is vital. It helps compare the economic merits of minimally invasive trauma surgery versus traditional open surgery. Key factors include equipment costs, hospital stay duration, and recovery time. These elements are critical in determining a treatment’s cost-effectiveness.
Research indicates that, despite higher initial costs for minimally invasive procedures, they can be more cost-effective. This is due to shorter hospital stays and reduced post-operative care needs.
Healthcare System Implications
Implementing minimally invasive trauma surgery on a broader scale has significant implications for healthcare systems. It can lead to cost savings and improve patient outcomes. It also helps alleviate the strain on healthcare resources.
Investing in surgeon training and acquiring necessary technology is key. This enables healthcare systems to deliver high-quality, affordable care to trauma patients.
Future Innovations in Minimally Invasive Trauma Surgery
Looking ahead, minimally invasive trauma surgery will be transformed by new technologies and clinical trials. The field is rapidly advancing, with several innovations on the horizon. These promise to improve patient outcomes and make surgical procedures more efficient.
Emerging Technologies
Several emerging technologies are poised to revolutionize minimally invasive trauma surgery. These include:
- Advanced robotic systems that offer enhanced precision and dexterity
- Artificial intelligence (AI) and machine learning algorithms that can assist in decision-making and predict patient outcomes
- 3D printing and bioprinting technologies that enable the creation of customized surgical models and implants
Research Directions and Clinical Trials
Ongoing research and clinical trials are essential for advancing minimally invasive trauma surgery. Current research focuses on:
- Investigating the efficacy of new energy devices and sealants in reducing bleeding and promoting healing
- Exploring the use of augmented reality and virtual reality to enhance surgical visualization and training
- Evaluating the safety and effectiveness of novel endoscopic instruments and techniques
These advancements are expected to significantly improve patient care. They will also expand the scope of minimally invasive trauma surgery, opening up new possibilities for treatment and recovery.
Making Informed Decisions About Surgical Approaches for Trauma Patients
Choosing the right surgical approach for trauma patients is a complex decision. It requires careful consideration of multiple factors. Minimally invasive trauma surgery has emerged as a valuable tool in treating various traumatic injuries.
Healthcare providers must weigh the benefits and risks of different techniques. They consider the patient’s specific condition, the injury’s severity, and the risk of complications. This careful evaluation is essential.
Advanced imaging and navigation technologies, specialized equipment, and a multidisciplinary team approach contribute to optimal outcomes. By considering these factors and staying updated with the latest research, healthcare providers can make informed decisions. These decisions improve patient care and outcomes.
The ultimate goal is to provide trauma patients with the most effective and least invasive treatment. This approach minimizes recovery time and improves their overall quality of life.
FAQ
Q: What is Minimally Invasive Trauma Surgery?
A: Minimally Invasive Trauma Surgery employs techniques that minimize incisions, reducing tissue damage and speeding up recovery. It treats various traumas, like blunt abdominal injuries, penetrating wounds, and orthopedic issues.
Q: What are the benefits of Minimally Invasive Trauma Surgery?
A: This surgery reduces trauma and blood loss, shortens hospital stays, and improves cosmetic results. These advantages lead to better patient outcomes and higher satisfaction.
Q: What types of trauma can be treated with Minimally Invasive Trauma Surgery?
A: It addresses blunt abdominal trauma, penetrating injuries, and orthopedic trauma. The chosen technique varies based on the injury’s nature and severity.
Q: What are the possible complications of Minimally Invasive Trauma Surgery?
A: Complications include bleeding, organ damage, and the need for open surgery. Careful patient selection and risk management strategies can mitigate these risks.
Q: How is patient selection and evaluation done for Minimally Invasive Trauma Surgery?
A: Identifying ideal candidates, assessing contraindications, and following preoperative protocols are key. This meticulous evaluation is vital for successful outcomes.
Q: What is the role of advanced imaging and navigation technologies in Minimally Invasive Trauma Surgery?
A: Technologies like intraoperative imaging, 3D visualization, and augmented reality enhance precision and outcomes. They are integral to the success of Minimally Invasive Trauma Surgery.
Q: What specialized equipment and instrumentation are used in Minimally Invasive Trauma Surgery?
A: The field employs endoscopic tools, robotic systems, and energy devices. These instruments facilitate precise interventions and improve patient results.
Q: How is post-operative care and recovery managed for patients undergoing Minimally Invasive Trauma Surgery?
A: Post-operative care includes immediate management, pain control, and rehabilitation. A thorough approach to post-operative care is critical for optimal recovery.















