Oral Cancer: What is Oral Cancer?
Oral Cancer is a major health issue affecting millions globally. It’s vital to understand its basics to provide accurate information and raise awareness. This serious health concern requires attention due to its widespread impact on global health. As professionals, it’s critical to grasp the fundamentals. This knowledge enables us to educate our audience effectively. Exploring the importance of Oral Cancer awareness helps us understand the necessity for education and prevention strategies. This knowledge is key to combating this disease.
Oral cancer is a major health issue affecting millions globally, requiring a deep understanding of its nature and effects. It occurs in the mouth or oral cavity, encompassing the lips, tongue, cheeks, gums, and throat. Given its various forms, grasping its medical aspects is key to effective diagnosis and treatment.
Definition and Medical Overview
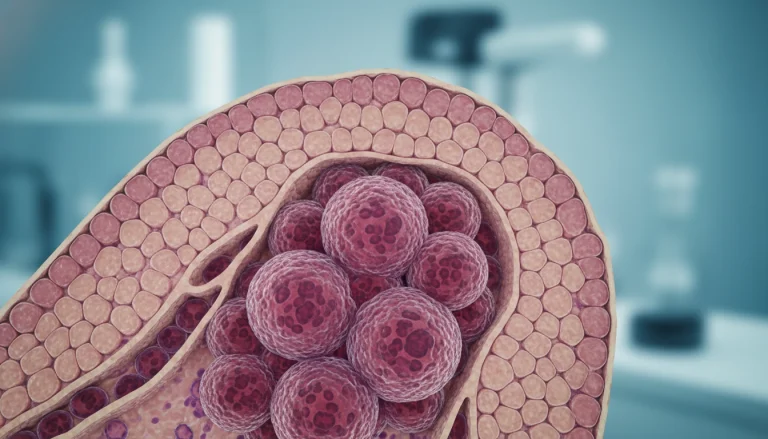
Oral cancer is a malignant tumor found in the oral cavity. The most prevalent form is squamous cell carcinoma, which starts in the squamous cells lining the mouth and throat. Other types include verrucous carcinoma and minor salivary gland carcinomas. Recognizing its pathology is vital, as it can invade nearby tissues and spread to other parts of the body.
Diagnosing oral cancer involves physical exams, imaging, and biopsies. Early detection is essential for better treatment outcomes and survival rates. The available treatments include surgery, radiation, and chemotherapy, as outlined in the medical overview.
Impact on Public Health
Oral cancer significantly affects public health, causing both morbidity and mortality. It ranks among the top ten most common cancers globally, placing a heavy burden on healthcare systems. In the United States, it is a leading cause of cancer deaths, highlighting the urgency for awareness and early detection.
The broader impact of oral cancer extends beyond individual patients, affecting families, communities, and society. Addressing risk factors like tobacco, alcohol, HPV, and poor oral hygiene is critical to reducing its public health burden.
Types of Oral Cancer
Grasping the various forms of oral cancer is vital for effective diagnosis and treatment. Oral cancer is a term that covers several malignant tumors found in the mouth. These cancers can develop in different areas, such as the lips, tongue, cheeks, gums, and throat.
Squamous Cell Carcinoma
Squamous cell carcinoma is the leading type of oral cancer, making up about 90% of cases. It starts in the squamous cells, which are flat, thin cells lining the mouth and lips. This cancer can appear anywhere in the mouth but is most common on the tongue and the floor of the mouth.
Factors increasing the risk of squamous cell carcinoma include tobacco use, alcohol consumption, and human papillomavirus (HPV) infection. Symptoms include a sore that won’t heal, a lump or thickening in the oral tissues, and trouble swallowing.
Verrucous Carcinoma
Verrucous carcinoma is a rare, slow-growing form of squamous cell carcinoma. It has a cauliflower-like appearance and often occurs in the oral cavity, mainly on the buccal mucosa or gingiva. It is commonly linked to chewing tobacco and betel nut use.
Treatment for verrucous carcinoma usually involves surgical removal. Its slow growth and low metastatic risk make its prognosis generally favorable.
Minor Salivary Gland Carcinomas
Minor salivary gland carcinomas are a diverse group of cancers from the minor salivary glands throughout the oral cavity. These glands produce saliva, keeping the mouth moist and aiding digestion. The most prevalent types are adenoid cystic carcinoma and mucoepidermoid carcinoma.
Symptoms include a painless swelling or lump in the mouth, difficulty swallowing, and numbness or pain in the affected area. Treatment usually involves surgery, sometimes followed by radiation therapy.
Epidemiology and Statistics
Grasping the epidemiology and statistics of oral cancer is key to crafting effective public health strategies. Epidemiology uncovers patterns, trends, and risk factors linked to the disease. This knowledge is essential for shaping prevention and treatment policies.
Prevalence in the United States
In the United States, oral cancer poses a substantial health risk, with thousands of new cases reported each year. Data shows oral cancer makes up about 3% of all new cancer cases. The American Cancer Society reports over 50,000 new cases annually, leading to around 10,000 deaths.
Oral cancer’s prevalence varies by region and demographic within the U.S. Older adults and those with a history of tobacco use face higher risks. Identifying these trends is critical for effective interventions.
Global Statistics
Oral cancer is a significant global health issue, with approximately 350,000 new cases worldwide each year. It’s more prevalent in South Asia, where betel quid chewing is common. Globally, oral cancer ranks as the 15th most common cancer.
Incidence and mortality rates for oral cancer differ significantly across countries and regions. These disparities are influenced by tobacco use, alcohol consumption, and HPV infection rates. Recognizing these global statistics is essential for international cooperation in prevention and control efforts.
Risk Factors for Oral Cancer
Oral cancer develops from a mix of lifestyle, environmental, and genetic factors. Knowing these risk factors is key for prevention, early detection, and managing the disease.
Tobacco and Alcohol Use
Tobacco use significantly raises the risk of oral cancer. This includes smoking cigarettes, cigars, or pipes, and using smokeless tobacco products. Alcohol, when combined with tobacco, further increases this risk. The combined effect of tobacco and alcohol on oral cancer risk is well-documented.
The chemicals in tobacco products can damage DNA in oral cavity cells, leading to cancer. Alcohol can also irritate tissues, making them more susceptible to carcinogens.
HPV Infection
Human Papillomavirus (HPV) infection, mainly type 16, is a risk factor for oropharyngeal cancers, a type of oral cancer. HPV-related oral cancers have a different demographic and risk profile compared to those caused by tobacco and alcohol.
There has been a rise in HPV-related oral cancers, mainly among younger people. Vaccination against HPV is seen as a preventive measure against these cancers.
Age, Gender, and Genetic Factors
Age is a major risk factor for oral cancer, with most cases in people over 40. Men are more likely to develop oral cancer than women, though the gap is decreasing.
Genetic factors also contribute, with certain genetic syndromes increasing oral cancer risk. Family history can indicate genetic predisposition.
Dietary and Environmental Factors
Dietary habits and environmental exposures can affect oral cancer risk. A diet low in fruits and vegetables may increase risk, while a diet rich in antioxidants can protect.
Exposure to certain environmental carcinogens, like those in certain jobs (e.g., asbestos in construction or textile industries), can also raise risk.
Understanding these risk factors helps individuals take preventive steps and seek early medical attention if symptoms appear.
Signs and Symptoms of Oral Cancer
It’s vital for patients to recognize the signs and symptoms of oral cancer early. This awareness is key to seeking timely medical attention. Oral cancer can present in various ways, making it essential to know its different forms.
Early Warning Signs
Early detection of oral cancer is critical for better treatment outcomes. The early warning signs include:
- Persistent mouth sores or ulcers that do not heal
- White or red patches on the gums, tongue, or lining of the mouth
- Unexplained bleeding or pain in the mouth
These signs are often overlooked or mistaken for less serious conditions. Regular oral examinations are necessary to catch them early.
Advanced Symptoms
As oral cancer progresses, symptoms become more apparent. They can include:
- Difficulty swallowing or speaking
- Numbness or pain in the mouth, tongue, or lips
- Loose teeth or dentures that no longer fit properly
Advanced symptoms can severely affect a patient’s quality of life. Timely intervention is essential.
Knowing the signs and symptoms of oral cancer helps individuals seek medical help early. This can significantly improve their prognosis. Regular dental check-ups and self-examinations are vital for early detection.
Diagnostic Procedures
Oral cancer diagnosis combines clinical evaluation, laboratory tests, and advanced imaging. Accurate diagnosis is key for effective treatment. The process involves several critical steps.
Physical Examination
A thorough physical examination is the initial step in diagnosing oral cancer. A healthcare professional inspects the oral cavity for abnormalities. They look for lumps, sores, or discolored areas. The professional also assesses the patient’s overall health and medical history.
Biopsy Techniques
If suspicious lesions are found, a biopsy may be performed. This is to check for cancer cells. There are various biopsy techniques, including incisional, excisional, and fine-needle aspiration biopsies. The choice depends on the lesion’s size and location.

Imaging Studies
Imaging studies, like X-rays and CT scans, help determine cancer extent. They check if the cancer has spread. These tests are vital for staging and treatment planning.
Laboratory Tests
Laboratory tests, including blood tests and tissue samples, detect cancer cells. They identify specific genetic markers. These tests help in understanding the cancer’s nature and planning treatment.
These diagnostic procedures enable accurate oral cancer diagnosis. They help determine the best treatment approach.
Staging and Grading of Oral Cancer
Understanding the stage and grade of oral cancer is vital for choosing the right treatment. Staging determines the cancer’s extent, including size and spread to other areas. Grading evaluates cancer cells to see how much they resemble normal cells.
TNM Classification System
The TNM Classification System is a key method for staging oral cancer. It looks at three main aspects: T (tumor size and extent), N (lymph node metastasis presence or absence), and M (distant metastasis presence or absence). These scores help determine the cancer’s overall stage, ranging from Stage I (early) to Stage IV (advanced).
This system offers a standardized way to describe oral cancer extent. It aids in communication among healthcare providers and guides treatment decisions.
Histological Grading
Histological grading is critical in evaluating oral cancer. It involves examining cancer cells under a microscope to assess their differentiation and aggressiveness. The cancer is graded as well-differentiated (low grade), moderately differentiated (intermediate grade), or poorly differentiated (high grade).
The cancer’s grade offers insights into its behavior and treatment response. Combining stage and grade provides a detailed understanding of the disease. This allows healthcare providers to create a tailored treatment plan for each patient.
Treatment Approaches
Managing oral cancer effectively requires a detailed treatment plan. This plan combines various therapeutic methods. The choice of treatment hinges on several factors. These include the cancer’s stage, location, and the patient’s health status.
Surgery
Surgery is a primary treatment for oral cancer. It aims to remove the tumor and affected tissues. Surgical methods range from simple excisions to complex procedures like neck dissections.
The surgery’s goal is to remove the cancer while preserving as much normal tissue and function as possible. Advances in surgical techniques, including reconstructive surgery, have significantly improved patient outcomes.
Radiation Therapy
Radiation therapy employs high-energy beams to kill or slow cancer cell growth. It can be used alone or in combination with surgery or chemotherapy.
Different radiation therapy types exist, including external beam radiation therapy and brachytherapy. The choice depends on the cancer’s stage and location.

Chemotherapy
Chemotherapy uses drugs to kill cancer cells. It can be used alone or with other treatments like surgery or radiation therapy.
Chemotherapy is often used for advanced oral cancers or when cancer has spread. The choice of chemotherapy drugs is based on several factors, including cancer type and stage.
Targeted Therapy and Immunotherapy
Targeted therapy and immunotherapy are newer treatments for oral cancer. Targeted therapy uses drugs that target cancer cells, minimizing harm to normal cells.
Immunotherapy boosts the body’s immune system to fight cancer more effectively. These therapies offer promising options for patients with advanced oral cancer.
Ongoing research aims to explore these therapies’ full potentials in treating oral cancer.
Rehabilitation and Recovery
Rehabilitation is key for oral cancer patients to regain their quality of life post-treatment. It involves a detailed approach to tackle physical and emotional hurdles. This ensures patients can overcome their challenges effectively.
Speech and Swallowing Therapy
Speech and swallowing therapy are essential for oral cancer patients. Treatment can harm the muscles and nerves for speaking and swallowing, causing issues. Speech-language pathologists help patients improve speech clarity and swallowing through specific exercises and techniques.
Patients may need to relearn safe swallowing to avoid aspiration and enhance communication. This therapy is customized to meet each patient’s needs, significantly impacting their recovery.
Dental and Facial Reconstruction
Dental and facial reconstruction are often needed to restore the mouth and face’s appearance and function after oral cancer treatment. This may include dental implants, prosthetics, and reconstructive surgery to repair damaged tissues.
These interventions not only enhance aesthetic outcomes but also restore chewing and speaking abilities. This significantly improves the patient’s quality of life.
Nutritional Support
Nutritional support is critical during the rehabilitation phase. Oral cancer patients may face challenges with eating and digesting food due to treatment effects. A dietitian can offer guidance on maintaining adequate nutrition, which may involve dietary adjustments or supplements.
Proper nutrition supports the healing process, maintains strength, and aids in recovery. Patients are advised to collaborate with their healthcare team to create a personalized nutrition plan.
Prevention Strategies
Reducing the risk of oral cancer involves lifestyle changes and regular health screenings. Understanding and applying these preventive steps can greatly lower oral cancer rates.
Lifestyle Modifications
Lifestyle changes are key in preventing oral cancer. Tobacco use, including smoking and chewing, is a major risk factor. Quitting tobacco significantly lowers the risk. Excessive alcohol consumption also increases the risk of oral cancer. A diet rich in fruits and vegetables provides essential nutrients and antioxidants, aiding in cancer prevention.
- Avoid tobacco products
- Limit alcohol consumption
- Eat a balanced diet rich in fruits and vegetables
Regular Screening and Self-Examination
Regular screenings by healthcare professionals are essential for oral cancer prevention. Dentists and healthcare providers can spot early signs during routine checks. Self-examination also plays a role in early detection. It’s important to know the normal look and feel of your mouth. Report any unusual lumps, sores, or discoloration to your healthcare provider.

HPV Vaccination
HPV is a known risk factor for certain oral cancers. Vaccination against HPV can prevent some oral cancer cases. The HPV vaccine is usually given to adolescents but can be given to adults in some cases. Discussing the HPV vaccine with a healthcare provider can help understand its benefits and risks.
Combining lifestyle changes, regular screenings, and HPV vaccination can greatly reduce oral cancer risk. These strategies are vital in the battle against oral cancer.
Living with Oral Cancer
Living with oral cancer is more than just treatment; it’s about coping with the psychological impact and finding support. Patients face numerous challenges that affect their quality of life.
Psychological Impact
Oral cancer diagnosis can deeply affect patients psychologically. Anxiety, depression, and fear of the unknown are common. The emotional burden of facing a potentially life-threatening illness can be overwhelming, impacting mental health and overall well-being.
It’s vital for patients to receive care that meets both physical and emotional needs. Head and neck cancers, including oral cancer, require a multidisciplinary approach to treatment and support.
Support Systems and Resources
Support systems are key in helping patients cope with oral cancer. Family, friends, and support groups offer emotional support, practical help, and a sense of community. Resources like counseling services, rehabilitation programs, and online forums are also invaluable.
- Support groups for patients and their families
- Counseling services to address psychological needs
- Rehabilitation programs to aid in recovery
Long-term Follow-up Care
Long-term follow-up care is essential for oral cancer patients. Regular check-ups help monitor for recurrence and manage treatment side effects. Follow-up care also includes rehabilitation efforts to improve speech, swallowing, and overall quality of life.
Understanding the challenges of living with oral cancer and accessing the right support and care can help patients navigate their journey better. This can improve their outcomes significantly.
Recent Advances in Oral Cancer Research
New breakthroughs in oral cancer research are reshaping how we diagnose and treat this disease. In recent years, there has been a significant leap in understanding oral cancer’s complexities. This has led to better diagnostic tools and treatment plans.
Emerging Treatments
Targeted therapy and immunotherapy are emerging as effective treatments for oral cancer. These methods have shown great promise in clinical trials. Targeted therapy uses drugs that attack cancer cells directly, minimizing damage to healthy tissues.

These innovative treatments are being studied in numerous research projects. They offer new hope for those battling oral cancer. The rise of personalized medicine is also expected to be a game-changer in oral cancer treatment.
Biomarkers and Early Detection
The search for biomarkers for oral cancer is a major focus of research. Biomarkers are biological molecules in blood, body fluids, or tissues that signal disease presence. Finding these biomarkers is key to early detection and diagnosis.
Scientists are looking into various biomarkers, including genetic and proteomic ones. Their goal is to create non-invasive tests for oral cancer. Early detection through biomarker screening can greatly enhance survival rates and quality of life for patients.
Conclusion
Oral Cancer is a major public health issue, affecting millions globally. It’s vital to grasp its causes, risk factors, and symptoms for early detection and effective treatment.
Different types of Oral Cancer, like Squamous Cell Carcinoma, demand specific diagnostic and treatment strategies. Medical advancements have improved these methods, leading to better patient results.
Prevention is key, with lifestyle changes and HPV vaccination helping to lower Oral Cancer rates. Ongoing research and awareness campaigns are critical in fighting this disease.
Through education, research support, and preventive actions, we can lessen Oral Cancer’s impact. This effort benefits both individuals and communities.
FAQ
Q: What is oral cancer?
A: Oral cancer is an uncontrolled growth of abnormal cells in the mouth, lips, tongue, or throat. It often appears as a persistent sore, lump, or lesion that won’t heal.
Q: What are the risk factors for oral cancer?
A: Several factors increase the risk of oral cancer. These include tobacco and alcohol use, HPV infection, age, gender, and genetic predisposition. Diet and environmental factors also play a role.
Q: What are the symptoms of oral cancer?
A: Symptoms of oral cancer include a persistent sore or lump in the mouth. Difficulty swallowing, numbness or pain in the mouth or lips, and voice changes are also common.
Q: How is oral cancer diagnosed?
A: Diagnosing oral cancer involves a physical exam, biopsy, imaging studies, and lab tests. This combination helps identify the disease accurately.
Q: What are the treatment options for oral cancer?
A: Treatment for oral cancer includes surgery, radiation, chemotherapy, targeted therapy, and immunotherapy. Each option is chosen based on the cancer’s stage and location.
Q: Can oral cancer be prevented?
A: Yes, preventing oral cancer is possible. Lifestyle changes like quitting tobacco and alcohol, getting HPV vaccinated, and maintaining good oral hygiene can reduce risk.
Q: What is the importance of early detection in oral cancer?
A: Early detection of oral cancer is vital. It improves treatment outcomes and survival rates. Regular screenings and self-exams are key to catching the disease early.
Q: What is the role of HPV vaccination in preventing oral cancer?
A: HPV vaccination can prevent certain types of oral cancer caused by the human papillomavirus. It’s an effective preventive measure.
Q: How does oral cancer affect quality of life?
A: Oral cancer and its treatment significantly impact quality of life. They affect eating, speaking, and swallowing abilities, as well as overall well-being.
Q: What support is available for people living with oral cancer?
A: Those living with oral cancer have access to various support systems. Counseling, support groups, and resources help manage the disease’s physical and psychological challenges.