Osteomalacia: Bone Health and Mineralization
Osteomalacia, a condition characterized by the softening of bones, affects individuals worldwide. It is caused by a deficiency in vitamin D, calcium, or phosphate. These nutrients are essential for bone mineralization. Maintaining good bone health is essential for overall well-being. The mineralization process is vital for bone strength and density. When this process is disrupted, conditions like Osteomalacia can occur.
Understanding the causes, symptoms, and treatment options for this condition is critical. It’s important for effective management and prevention. This article will provide an overview of Osteomalacia, focusing on its impact on bone health and the importance of proper mineralization.
Understanding Bone Health and Mineralization
Healthy bones are the cornerstone of a robust body, supporting our structure and enabling movement. The topic of bone health is complex, involving bone formation, mineralization, and remodeling processes.
Normal Bone Structure and Function
Bones are dynamic organs that offer structural support, protect internal organs, and enable movement by attaching to muscles. The bone structure includes a dense outer layer, cortical bone, and a spongy inner layer, trabecular bone.
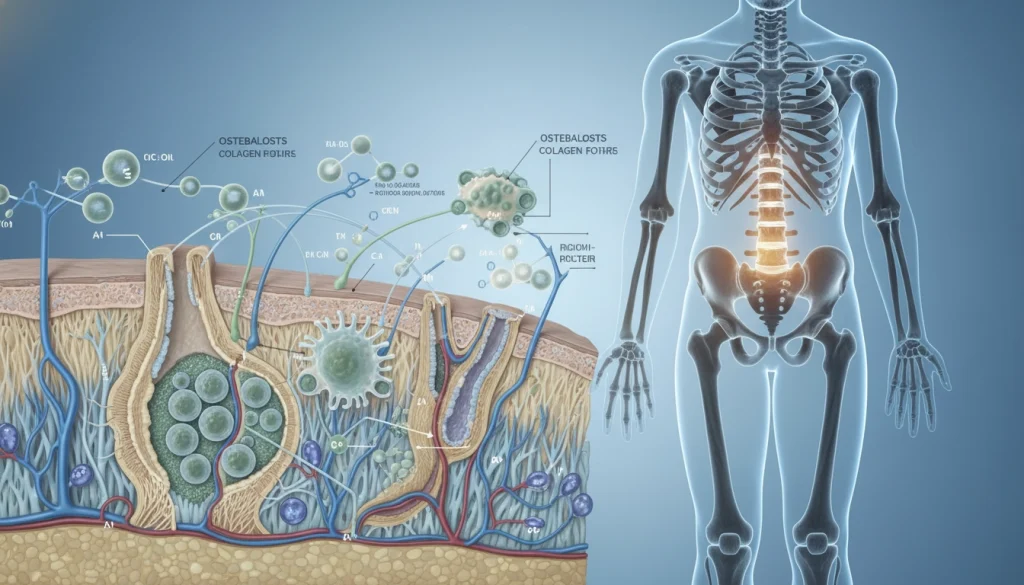
The bone’s integrity is sustained through continuous bone remodeling. This process replaces old bone tissue with new, essential for maintaining bone health. It involves the coordinated action of various cell types, including osteoblasts and osteoclasts.
The Role of Minerals in Bone Health
Minerals, mainly calcium and phosphate, are vital for bone health, contributing to bone mineralization. Calcium is essential for bone hardening, while phosphate is necessary for hydroxyapatite formation, the main bone mineral.
Adequate intake of these minerals, along with vitamin D, is critical for maintaining bone density. It helps prevent bone disorders like Osteomalacia.
Osteomalacia: Definition and Overview
Osteomalacia is a bone disorder marked by defective mineralization, causing the bones to soften.
What Distinguishes Osteomalacia from Other Bone Disorders
Osteomalacia stands out from other bone disorders because of its unique characteristic: the failure of bone mineralization. Unlike osteoporosis, which is characterized by a decrease in bone mass and density, osteomalacia affects the bone’s quality. This makes it more susceptible to deformities and fractures.
- Defective mineralization process
- Softening of bones
- Increased risk of fractures and deformities
Global Prevalence and Impact
Osteomalacia is widespread globally, affecting areas with limited sunlight or poor nutrition. It not only affects an individual’s quality of life but also burdens healthcare systems.
The prevalence of osteomalacia varies worldwide. It is higher in certain groups, such as the elderly and those with dietary restrictions.
- Higher prevalence in regions with limited sunlight
- Increased risk among elderly populations
- Impact on healthcare systems due to related complications
The Pathophysiology of Osteomalacia
Osteomalacia, a condition where bones soften, stems from the disruption of bone remodeling and mineralization. It arises from a complex interplay of physiological processes gone wrong.
Bone Remodeling Process
Bone remodeling is a continuous cycle of bone breakdown and formation. It’s essential for bone health, repairing micro-fractures, and adapting to mechanical loads. In osteomalacia, this balance is disrupted.
This process is regulated by hormones, growth factors, and cytokines. Any disruption in this system can lead to abnormalities in bone remodeling, contributing to osteomalacia.
Mineralization Defects
Mineralization defects are a hallmark of osteomalacia. The condition is characterized by a failure to mineralize new bone matrix, leading to an accumulation of osteoid tissue. This is mainly due to deficiencies in calcium and phosphate, or abnormalities in vitamin D metabolism.
The mineralization process requires adequate calcium and phosphate ions. In osteomalacia, the lack of these minerals or an imbalance in their regulation impairs mineralization, resulting in soft and weakened bones.
Cellular and Molecular Mechanisms
The cellular and molecular mechanisms underlying osteomalacia involve a complex interplay of various cell types, including osteoblasts, osteoclasts, and osteocytes. Abnormalities in the expression of genes involved in mineralization, such as those regulating vitamin D and phosphate metabolism, contribute to the pathophysiology of osteomalacia.
At the molecular level, osteomalacia is associated with alterations in the signaling pathways that regulate bone cell function and mineralization. Understanding these mechanisms is key to developing targeted therapeutic strategies.
Common Causes of Osteomalacia
Understanding the common causes of osteomalacia is key to diagnosing and treating this bone disorder. It stems from a mix of factors that soften bones.
Vitamin D Deficiency
Vitamin D is vital for bone health, managing calcium levels and mineralization. A lack of vitamin D is a leading cause of osteomalacia.
Inadequate Sun Exposure
Sunlight is necessary for vitamin D production in the skin. Those with little sun exposure, like those in northern latitudes or wearing full clothing, risk vitamin D deficiency.
Dietary Insufficiency
A diet lacking vitamin D and calcium can lead to osteomalacia. Foods like fatty fish, egg yolks, and fortified dairy are rich in vitamin D.
Malabsorption Syndromes
Gastrointestinal disorders like celiac disease and Crohn’s disease can block vitamin D and calcium absorption. This leads to osteomalacia.
Phosphate Deficiency and Metabolism Disorders
Phosphate is essential for bone health. Deficiencies or disorders in phosphate metabolism can cause osteomalacia. Conditions like hypophosphatemia and renal phosphate wasting are linked to this disorder.
Medication-Induced Osteomalacia
Some medications can disrupt bone mineralization, causing osteomalacia. Anticonvulsants, certain antacids, and HIV drugs are examples.
Genetic and Hereditary Causes
Genetic mutations affecting vitamin D metabolism or phosphate regulation can cause osteomalacia. X-linked hypophosphatemia and vitamin D-dependent rickets are examples.
Risk Factors for Developing Osteomalacia
The risk of developing Osteomalacia is influenced by a combination of demographic, dietary, and medical factors. Understanding these risk factors is essential for early diagnosis and prevention.
Demographic and Geographic Factors
Demographic and geographic factors significantly impact the risk of Osteomalacia. People living in areas with limited sunlight, like during winter, face a higher risk. This is because their skin produces less vitamin D. The elderly and those with limited mobility are also more susceptible.
Dietary and Nutritional Factors
Dietary habits and nutritional deficiencies are critical risk factors for Osteomalacia. A diet lacking sufficient vitamin D and calcium can lead to impaired bone mineralization. Individuals who follow a strict vegan diet or have limited dairy consumption are at increased risk.
Medical Conditions and Medications
Certain medical conditions and medications can increase the risk of developing Osteomalacia. Conditions such as celiac disease, Crohn’s disease, and kidney disorders can impair nutrient absorption. Medications like anticonvulsants and certain antacids can also interfere with vitamin D and calcium metabolism.
Clinical Symptoms and Signs of Osteomalacia
Osteomalacia, a condition where bones soften, shows various symptoms important for early detection.
The symptoms of osteomalacia include bone-related issues, muscle weakness, and sometimes neurological signs.
Bone Pain and Tenderness
Bone pain is a key symptom of osteomalacia, often described as deep and aching. This pain can affect the hips, back, or legs.
- Pain worsens with physical activity or pressure on the bones.
- Tenderness to touch is common, showing bone pathology.
- In severe cases, pain can limit mobility and daily activities.
Muscle Weakness and Fatigue
Muscle weakness and fatigue are common symptoms. This weakness often affects muscles near the body’s center.
Patients may struggle with tasks needing strength, like climbing stairs or getting up from a chair.
Skeletal Deformities and Fractures
In severe cases, osteomalacia can cause skeletal deformities and a higher risk of fractures. These deformities come from softening and malformation of bones.
- Bowing of the legs is a common deformity, seen in children with rickets.
- Fractures can happen with little trauma due to weak bones.
- Vertebral compression fractures can cause loss of height and kyphosis.
Neurological and Other Systemic Manifestations
Osteomalacia can also lead to neurological and systemic symptoms. These include numbness or tingling in the hands and feet.
Low calcium levels can cause tetany, marked by muscle cramps, spasms, or convulsions.
It’s vital to recognize these symptoms for timely diagnosis and treatment. This improves patient outcomes and quality of life.
Diagnostic Approaches for Osteomalacia
Diagnosing osteomalacia requires a detailed approach. It involves assessing patient history, conducting laboratory tests, and using imaging techniques. Accurate diagnosis is key for effective treatment and management.
Clinical Evaluation and History Taking
Clinical evaluation and history taking are the first steps in diagnosing osteomalacia. Healthcare providers look for symptoms like bone pain, muscle weakness, and difficulty walking. They also examine the patient’s medical history to identify risk factors.
Risk factors include nutritional deficiencies, gastrointestinal disorders, or medication use that may lead to osteomalacia.
Laboratory Tests and Biomarkers
Laboratory tests are vital in diagnosing osteomalacia. Key biomarkers include:
- Vitamin D levels
- Calcium and phosphate measurements
- Alkaline phosphatase and other markers
Vitamin D Levels
Measuring vitamin D levels is essential. Vitamin D deficiency is a common cause of osteomalacia. Serum 25-hydroxyvitamin D is the most reliable indicator of vitamin D status.
Calcium and Phosphate Measurements
Serum calcium and phosphate levels are also critical. Low levels of either can indicate osteomalacia, often with elevated alkaline phosphatase.
Alkaline Phosphatase and Other Markers
Alkaline phosphatase is often elevated in osteomalacia due to increased bone turnover. Other markers, such as parathyroid hormone (PTH), may also be assessed to understand the underlying pathology.
Imaging Studies and Radiological Findings
Imaging studies, including X-rays and bone densitometry, help identify characteristic changes associated with osteomalacia. These include Looser’s zones (pseudofractures) and osteopenia.
Bone Biopsy and Histological Examination
In some cases, a bone biopsy may be performed to confirm the diagnosis. Histological examination typically reveals defective mineralization and an accumulation of osteoid tissue.
By integrating findings from clinical evaluation, laboratory tests, and imaging studies, healthcare providers can accurately diagnose osteomalacia. This allows for the development of an effective treatment plan.
Differential Diagnosis of Osteomalacia
Differential diagnosis is key in identifying Osteomalacia, as its symptoms can mimic other metabolic bone diseases. Accurate diagnosis is essential for effective treatment and management.
Osteoporosis vs. Osteomalacia
Osteoporosis and Osteomalacia are distinct bone disorders. Osteoporosis is marked by a decrease in bone mass and density, increasing fracture risk. On the other hand, Osteomalacia involves softening of bones due to defective mineralization. Both conditions can cause bone pain and increased fracture risk but have different causes and treatments.
Fibromyalgia and Chronic Pain Syndromes
Fibromyalgia, a chronic condition with widespread muscle pain, can be mistaken for Osteomalacia. Despite similar symptoms like bone pain and fatigue, fibromyalgia lacks the bone mineralization defects of Osteomalacia. A detailed clinical evaluation and diagnostic tests are needed to distinguish between the two.
Other Metabolic Bone Diseases
Osteomalacia must be differentiated from other metabolic bone diseases, such as Paget’s disease and renal osteodystrophy. These conditions have unique causes and require specific treatments. Laboratory tests and imaging studies are vital for accurate diagnosis.
Comprehensive Treatment Options for Osteomalacia
Treating osteomalacia requires a multi-faceted approach. This includes supplementation, lifestyle changes, and sometimes surgery. Understanding the condition’s causes is key to effective treatment.

Vitamin D Supplementation Protocols
Vitamin D supplements are essential for treating osteomalacia, mainly when it’s caused by a deficiency.
Loading Doses
High doses of vitamin D are given first to quickly fix the deficiency. This is vital for those with severe osteomalacia.
Maintenance Therapy
Once the deficiency is corrected, lower doses of vitamin D are used for maintenance. Regular supplements help keep levels normal.
Monitoring Response
It’s important to regularly check vitamin D levels and bone health markers. This helps adjust the treatment plan as needed.
Calcium and Phosphate Management
Managing calcium and phosphate levels is also critical. This might involve changing diets or using supplements to meet needs.
Addressing Underlying Causes and Conditions
Treating osteomalacia also means tackling any underlying issues. This includes conditions like gastrointestinal disorders or renal phosphate wasting.
Surgical Interventions for Complications
Surgery may be needed for severe bone deformities or fractures caused by osteomalacia. It aims to improve the patient’s quality of life.
Complications of Untreated Osteomalacia
If left untreated, Osteomalacia can lead to severe complications that significantly impact an individual’s quality of life. These issues can be debilitating, affecting not just the skeletal system but overall health and well-being.
Fractures and Progressive Bone Deformities
Untreated Osteomalacia increases the risk of fractures. Weakened bones are more prone to breaks. In severe cases, this can lead to progressive bone deformities. These deformities can cause chronic pain and limited mobility, complicating the patient’s condition further.
Chronic Pain and Disability
Chronic pain is a common complication of Osteomalacia, stemming from bone pain and muscle weakness. This pain can be debilitating, affecting an individual’s ability to perform daily activities and maintain independence. The chronic nature of this pain can also lead to disability, impacting both physical and mental health.
Psychological Impact and Reduced Quality of Life
The psychological impact of untreated Osteomalacia should not be underestimated. Chronic pain and disability can lead to depression, anxiety, and a reduced quality of life. The limitations imposed by the condition can affect social interactions, work, and overall well-being. This highlights the need for timely and effective treatment.
Prevention Strategies for Osteomalacia
To prevent osteomalacia, a multi-faceted approach is necessary. This includes dietary adjustments, lifestyle changes, and the right supplements. Understanding risk factors and taking preventive steps can greatly lower the chance of getting this condition.
Dietary Recommendations and Nutritional Planning
A diet rich in calcium, vitamin D, and phosphate is key to bone health and preventing osteomalacia. Include dairy, leafy greens, and fortified cereals in your meals for these nutrients.
- Add calcium-rich foods like milk, cheese, and yogurt to your diet.
- Eat foods high in vitamin D, such as fatty fish, egg yolks, and fortified dairy.
- Make sure to include phosphate-rich foods like meat, fish, and eggs in your meals.
Creating a diet plan that covers these essential nutrients can help prevent osteomalacia, mainly in those at higher risk.
Lifestyle Modifications and Sun Exposure
Lifestyle changes are vital in preventing osteomalacia. One of the best ways to increase vitamin D is through regular sun exposure.
- Spending time outdoors, mainly during peak sun hours, boosts vitamin D production.
- Use sunscreen wisely, as it can block vitamin D production.
- Regular physical activity helps maintain bone density and overall health.
Preventive Supplementation Guidelines
At times, diet and lifestyle changes alone may not be enough to prevent osteomalacia. In such cases, supplements may be needed.
- Discuss vitamin D and calcium supplements with a healthcare provider.
- Follow the recommended dosage to avoid toxicity.
- Keep an eye on nutrient levels and adjust supplements as necessary.
Combining dietary advice, lifestyle changes, and supplements can effectively lower osteomalacia risk. It’s critical to work with healthcare professionals to create a prevention plan that fits your needs.
Special Populations and Osteomalacia Considerations
Children, pregnant women, and the elderly face unique challenges with osteomalacia. Each group has specific risk factors and symptoms, requiring personalized diagnosis, treatment, and prevention strategies.
Pediatric Osteomalacia (Rickets)
Rickets, or osteomalacia in children, hampers bone development, causing soft and deformed bones. It’s mainly caused by a lack of vitamin D, stemming from poor diet, insufficient sun exposure, or genetic issues affecting vitamin D processing.
Signs include bowed legs, stunted growth, and bone pain. Prompt treatment with vitamin D and calcium can avert lasting skeletal issues.
Osteomalacia During Pregnancy and Lactation
Pregnancy and breastfeeding heighten the need for calcium and vitamin D, making these women more prone to osteomalacia. This condition can pose risks to both mother and child, including a higher fracture risk and impaired fetal development.
It’s vital to monitor vitamin D levels and ensure proper nutrition during these periods to prevent osteomalacia.
Geriatric Patients and Age-Related Factors
The elderly are more susceptible to osteomalacia due to reduced sun exposure, lower dietary intake of vitamin D and calcium, and declining kidney function with age. This condition can worsen osteoporosis, raising the risk of fractures.
Regular vitamin D deficiency screening and supplementation are key to preventing osteomalacia in older adults.

Advances in Osteomalacia Research and Future Treatments
Recent years have brought significant breakthroughs in Osteomalacia research. These advancements have illuminated the condition’s pathophysiology and opened up new avenues for treatment. The emerging evidence points to a deeper understanding of Osteomalacia’s molecular mechanisms. This understanding is key to developing targeted treatments.
Future treatments for Osteomalacia may include novel vitamin D analogs and phosphate-binding agents. These interventions aim to enhance bone mineralization and density. Researchers are also looking into gene therapy to address genetic causes of Osteomalacia.
The evolving understanding of Osteomalacia is transforming clinical practice. Healthcare providers can now diagnose and manage the condition more effectively. As research progresses, patients with Osteomalacia will have access to improved treatment options and better outcomes.
Advances in Osteomalacia research are set to drive innovation in treatment approaches. This offers new hope for those affected by this debilitating condition. Healthcare professionals can provide the best care by staying updated with these developments.
FAQ
Q: What is Osteomalacia?
A: Osteomalacia is a condition where bones become soft due to a lack of vitamin D, calcium, or phosphate.
Q: What are the common causes of Osteomalacia?
A: Common causes include vitamin D deficiency, phosphate deficiency, and effects from certain medications. Genetic factors also play a role.
Q: How is Osteomalacia diagnosed?
A: Diagnosing Osteomalacia involves clinical evaluation, lab tests, imaging, and sometimes a bone biopsy.
Q: What are the symptoms of Osteomalacia?
A: Symptoms include bone pain, muscle weakness, and skeletal deformities. Neurological issues can also occur.
Q: How is Osteomalacia treated?
A: Treatment involves vitamin D supplements, managing calcium and phosphate, and addressing underlying causes. Surgery may be needed for complications.
Q: Can Osteomalacia be prevented?
A: Yes, prevention is possible through diet, lifestyle changes, and supplements.
Q: What are the complications of untreated Osteomalacia?
A: Untreated Osteomalacia can lead to fractures, chronic pain, and psychological effects.
Q: How does Osteomalacia affect different populations?
A: It affects various groups, like children (Rickets), pregnant women, and the elderly. Each group requires specific care.