Pancreas: Pancreatic Enzymes and Digestive Processes
The human body is home to many vital organs, each with its own role in our health. This article focuses on one such organ. This organ is key for digestion and managing blood sugar levels. It produces enzymes and hormones that help with these tasks. Knowing its functions and the disorders it can face is essential for understanding its role in our health. Issues with this organ can have serious health effects. It’s important to grasp its significance and how to keep it healthy.
The Anatomy and Structure of the Pancreas
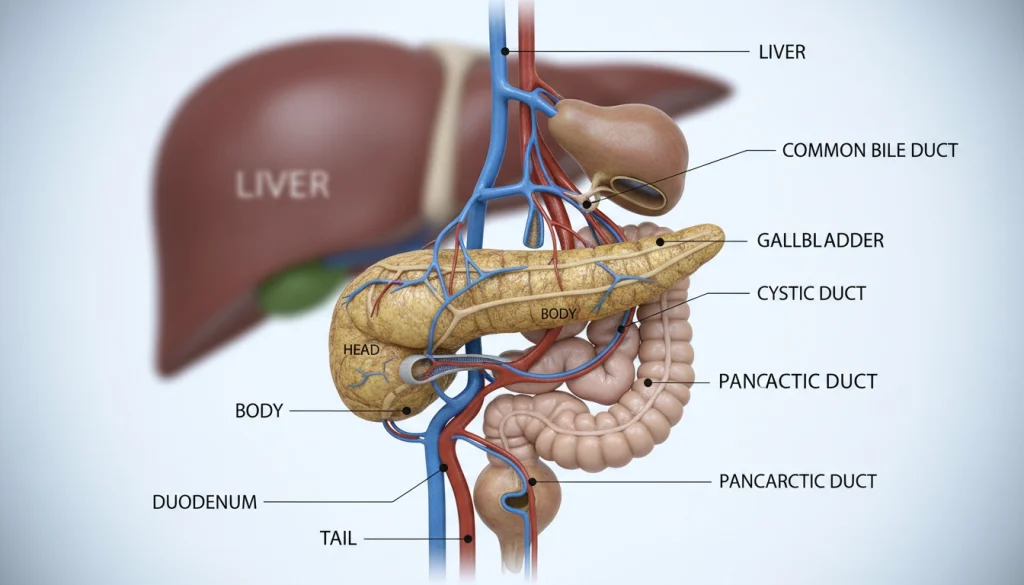
The pancreas, an organ integral to the digestive system, boasts a complex structure. It resides behind the stomach in the abdominal cavity. It is nestled between the duodenum and the spleen.
Location Within the Digestive System
The pancreas is strategically positioned within the digestive system. This location enables it to play a vital role in digestion. It is closely associated with the duodenum, the first part of the small intestine, through which it secretes digestive enzymes.
The pancreas is divided into the head, body, and tail. The head is near the duodenum, while the tail extends towards the spleen. This arrangement allows the pancreas to effectively discharge its digestive enzymes into the intestine.
Microscopic Structure and Tissue Types
Microscopically, the pancreas is composed of two main tissue types: exocrine and endocrine. The exocrine component, making up the majority of the pancreas, is responsible for producing digestive enzymes. These enzymes are secreted into the ductal system and eventually into the duodenum to facilitate nutrient breakdown.
The endocrine component, comprising the islets of Langerhans, produces hormones such as insulin and glucagon. These hormones are essential for regulating blood glucose levels.
Blood Supply and Innervation
The pancreas receives its blood supply from several arteries, including the splenic artery and the superior and inferior pancreaticoduodenal arteries. The venous drainage is mainly through the splenic vein and the superior mesenteric vein.
The pancreas is innervated by both the sympathetic and parasympathetic nervous systems. These systems regulate its secretory functions. The sympathetic innervation inhibits pancreatic secretion, while the parasympathetic innervation stimulates it.
Essential Functions of the Pancreas
The pancreas plays a unique role in our body, balancing hormones and digestive enzymes. It’s vital for metabolic health and nutrient digestion.
Endocrine Role in Hormone Production
The pancreas’ endocrine part is key in hormone production. It mainly produces insulin and glucagon, which control blood sugar levels. Insulin helps cells absorb glucose, while glucagon releases glucose from the liver.
These hormones come from the islets of Langerhans, special cells in the pancreas. The balance between insulin and glucagon is essential for glucose stability.
Exocrine Role in Digestive Enzyme Secretion
The exocrine part of the pancreas makes digestive enzymes. These enzymes go to the small intestine to break down food into nutrients. Amylase, lipase, and trypsin are key for digesting carbs, fats, and proteins.
The pancreas controls enzyme secretion to match food intake. This ensures efficient digestion.
Regulatory Mechanisms
The pancreas works under strict control. Hormonal and neural signals regulate its functions. These signals come from the gut and nervous system.
For example, insulin release is triggered by blood sugar and gut hormones. Digestive enzyme secretion is also controlled by food presence in the intestine.
Pancreatic Enzymes and Digestive Processes
The pancreas is vital for producing enzymes that aid in nutrient absorption. These enzymes are key in breaking down food into smaller molecules. These molecules are then used by the body for energy and other essential functions.

Types of Digestive Enzymes Produced
The pancreas creates various digestive enzymes, such as amylase, lipase, and trypsin. Amylase breaks down carbohydrates into simple sugars. Lipase is responsible for converting fats into fatty acids and glycerol. Trypsin, involved in protein digestion, breaks proteins into smaller peptides and amino acids.
Activation Pathways
The activation of pancreatic enzymes is a complex process. Some enzymes, like trypsin, are produced as inactive precursors (trypsinogen) to prevent premature activation. Once released into the duodenum, trypsinogen is activated to trypsin by enterokinase. This enzyme is produced by the intestinal tract’s cells.
Role in Nutrient Breakdown and Absorption
Pancreatic enzymes are critical for efficient nutrient breakdown and absorption. Without enough enzyme production, the body cannot absorb necessary nutrients. This leads to malnutrition and various health problems. The enzymes work with bile and other digestive juices to break down carbohydrates, proteins, and fats into absorbable components.
Hormonal Regulation and Metabolic Control
The pancreas is vital for metabolic control through hormonal regulation. It achieves this by secreting various hormones. These hormones play key roles in metabolism.
Insulin: Production, Release, and Function
Insulin is produced by the beta cells of the pancreatic islets. It is released when blood glucose levels rise. Insulin helps cells absorb glucose, lowering blood glucose.
Insulin’s role in glucose metabolism is critical. Its dysfunction is closely tied to diabetes mellitus.
Glucagon and Glucose Homeostasis
Glucagon, produced by the alpha cells, has the opposite effect of insulin. It increases blood glucose levels by stimulating glycogenolysis and gluconeogenesis.
The balance between insulin and glucagon is essential for glucose homeostasis. It ensures blood glucose levels stay within a healthy range.
Somatostatin and Other Regulatory Hormones
Somatostatin, produced by the delta cells, regulates the secretion of other hormones. This includes insulin and glucagon.
It acts as a modulator, ensuring hormonal balance. This balance is vital for proper metabolic function.
Pancreatic Polypeptide Functions
Pancreatic polypeptide is secreted by the PP cells. It regulates pancreatic exocrine function.
It also plays a role in glucose metabolism. The exact mechanisms are under study.
The complex balance of these hormones highlights the complexity of metabolic control. The pancreas plays a critical role in maintaining homeostasis.
Acute Pancreatitis: Causes, Symptoms, and Management
Acute pancreatitis is a serious condition where the pancreas quickly inflames. This usually happens due to gallstones or too much alcohol. The sudden inflammation can cause severe abdominal pain and serious complications if not treated quickly.
Gallstone-Induced vs. Alcoholic Pancreatitis
There are two main types of acute pancreatitis: gallstone-induced and alcoholic. Gallstones blocking the pancreatic duct can start an inflammatory response. Excessive alcohol, on the other hand, can directly harm the pancreas.
Knowing the cause is key to choosing the right treatment. It helps in creating a plan to avoid future episodes.
Clinical Presentation and Diagnosis
The symptoms of acute pancreatitis include severe abdominal pain, nausea, and vomiting. Doctors use lab tests to check for high pancreatic enzymes and CT scans to see how much inflammation there is.
Getting a diagnosis early is vital for starting the right treatment and lowering the risk of complications. The severity of pancreatitis can vary, from mild to life-threatening.
Treatment Approaches and Complications
Managing acute pancreatitis involves supportive care like fluids, pain relief, and nutrition. In severe cases, intensive care may be needed to handle complications like necrosis or organ failure.
Complications can include infections, pseudocysts, and long-term pancreatic issues. Quick and proper management is key to reducing these risks and improving patient outcomes.
Chronic Pancreatitis and Long-Term Implications
Chronic pancreatitis is a persistent inflammatory condition of the pancreas, leading to irreversible damage. It is marked by recurring episodes of pancreatitis, causing progressive fibrosis. This damage impairs both the exocrine and endocrine functions of the pancreas.
Pathophysiology and Risk Factors
The pathophysiology of chronic pancreatitis involves complex interactions between genetic predisposition, environmental factors, and immune responses. Risk factors include chronic alcohol consumption, genetic mutations, and certain metabolic disorders. Understanding these factors is key for early diagnosis and intervention.
Progressive Symptoms and Quality of Life Impact
Patients with chronic pancreatitis face progressive symptoms, including persistent abdominal pain, malabsorption, and diabetes mellitus. These symptoms severely impact their quality of life. Aiming for a better quality of life, management strategies are essential to alleviate suffering and improve functional status.
Management Strategies and Pain Control
Managing chronic pancreatitis requires a multidisciplinary approach, focusing on pain control, nutritional support, and managing exocrine and endocrine insufficiencies. Pain management includes pharmacological interventions, endoscopic procedures, and surgical options. Pancreatic enzyme replacement therapy is also vital for managing malabsorption.
Effective management of chronic pancreatitis demands a tailored approach, considering each patient’s specific needs and condition severity. By addressing these complex needs, healthcare providers can significantly improve patients’ quality of life. This approach helps mitigate the long-term implications of this debilitating condition.
Pancreatic Cancer: The Silent Disease
Pancreatic cancer is a formidable foe in the field of oncology, with a high mortality rate. It demands early detection and effective treatment strategies. The disease often lacks symptoms in its early stages, making diagnosis difficult until it has advanced.
Epidemiology and Risk Assessment
Pancreatic cancer is a significant global health concern, with varying incidence rates. Risk factors include smoking, obesity, family history of pancreatic cancer, and certain genetic syndromes.
- Smoking: A major risk factor, contributing to approximately 20-30% of pancreatic cancer cases.
- Obesity: Being overweight or obese is linked with an increased risk of developing pancreatic cancer.
- Genetic Predisposition: Individuals with a family history or certain genetic mutations are at higher risk.
Early Detection Challenges
Early detection of pancreatic cancer is challenging due to its non-specific symptoms and the lack of effective screening tests for the general population. Symptoms often appear when the disease is advanced, complicating treatment efforts.
Staging and Prognosis Factors
The staging of pancreatic cancer is critical for determining prognosis and treatment planning. Factors influencing prognosis include the stage at diagnosis, tumor size, and the presence of metastasis.
- Stage I: Cancer is localized within the pancreas.
- Stage IV: Cancer has spread to distant parts of the body, indicating a poor prognosis.
Current Treatment Modalities
Treatment for pancreatic cancer depends on the stage and location of the tumor, as well as the patient’s overall health. Current modalities include surgery, chemotherapy, radiation therapy, and targeted therapy.
- Surgery: Offers the only chance for a cure in localized pancreatic cancer.
- Chemotherapy: Used before or after surgery, or as palliative care.
- Radiation Therapy: Can be used in combination with chemotherapy.
Diabetes Mellitus and Pancreatic Dysfunction
It’s vital to grasp the connection between diabetes mellitus and pancreatic issues for better disease management. Diabetes mellitus is a metabolic disorder group, marked by high blood sugar levels. This happens due to problems with insulin production or action.
The pancreas is key in managing blood sugar levels by making insulin and glucagon. When the pancreas doesn’t work right, different types of diabetes can occur. Each type has its own set of symptoms and causes.
Type 1 Diabetes: Autoimmune Destruction
Type 1 diabetes is an autoimmune disease. In it, the immune system attacks and destroys the insulin-making beta cells in the pancreas. This leads to a lack of insulin, forcing people to take insulin shots to control their blood sugar.
Type 2 Diabetes: Insulin Resistance and Secretory Defects
Type 2 diabetes is caused by insulin resistance and poor insulin production. At first, the pancreas tries to keep up by making more insulin. But eventually, it can’t keep up, causing high blood sugar levels.
Pancreatic Diabetes (Type 3c)
Pancreatic diabetes, or type 3c diabetes, happens when the pancreas’s exocrine part is damaged. This can be due to pancreatitis, surgery, or cancer. It’s often missed and needs a detailed treatment plan.
Gestational Diabetes and Pancreatic Adaptation
Gestational diabetes mellitus (GDM) happens during pregnancy, usually in the second or third trimester. It’s caused by insulin resistance and pancreatic beta-cell problems. Managing GDM is critical to avoid risks for both the mother and the baby.
In summary, diabetes mellitus is a diverse group of conditions closely tied to pancreatic issues. Knowing the different types of diabetes and their causes is key to finding effective treatments.
Advanced Diagnostic Techniques for Pancreatic Disorders
Diagnosing pancreatic disorders demands a multi-faceted approach. Advanced diagnostic techniques are essential for accurately identifying and managing these conditions. They range from pancreatitis to pancreatic cancer.
Laboratory Biomarkers and Blood Tests
Laboratory biomarkers are vital in diagnosing pancreatic disorders. Blood tests can detect elevated levels of pancreatic enzymes like amylase and lipase. These are signs of pancreatitis. Biomarkers like CA 19-9 are used for diagnosing and monitoring pancreatic cancer.
- Amylase and lipase levels for pancreatitis
- CA 19-9 for pancreatic cancer
- Other relevant biomarkers for specific conditions
Imaging Modalities: CT, MRI, and Endoscopic Ultrasound
Imaging modalities are key for visualizing the pancreas and diagnosing disorders. CT scans offer detailed cross-sectional images, useful for spotting tumors and pancreatitis. MRI provides high-resolution images of pancreatic tissue and ducts. Endoscopic ultrasound (EUS) is excellent for detailed examination of the pancreas and surrounding tissues.

- CT scans for overall pancreatic assessment
- MRI for detailed tissue and duct evaluation
- EUS for precise examination of the pancreas and surrounding structures
Functional Testing and Genetic Screening
Functional testing, like pancreatic function tests, evaluates the pancreas’s exocrine function. Genetic screening is also critical. It helps identify mutations that increase the risk of pancreatic cancer or other disorders.
By using these advanced diagnostic techniques, healthcare providers can accurately diagnose and manage pancreatic disorders. This improves patient outcomes significantly.
Surgical Interventions for Pancreatic Conditions
Surgical interventions are key in managing pancreatic conditions. The choice of surgery depends on the condition’s nature and extent.
Pancreaticoduodenectomy (Whipple Procedure)
The Whipple procedure, or pancreaticoduodenectomy, is a complex surgery. It removes a pancreatic tumor or diseased part of the pancreas. The surgery takes out the head of the pancreas, the duodenum, and sometimes other tissues.
This procedure is often used for pancreatic cancer in the head of the pancreas. It can help alleviate symptoms and potentially improve survival rates.
Distal Pancreatectomy and Total Pancreatectomy
Distal pancreatectomy removes the body and tail of the pancreas. It’s used for tumors or diseases in these areas.
Total pancreatectomy removes the entire pancreas. It’s a more extensive surgery, but sometimes necessary for widespread disease.
Minimally Invasive Approaches
Minimally invasive techniques, like laparoscopic and robotic-assisted surgery, are becoming more common. They offer benefits like shorter recovery times and less pain post-surgery.
Post-Surgical Management and Complications
Post-surgical management is vital for the best outcomes and to avoid complications. It includes monitoring for infection, managing pain, and nutritional support.
Potential complications include pancreatic fistula, infection, and diabetes. A team approach is essential for managing these and ensuring the best outcomes.
Living with Pancreatic Exocrine Insufficiency
Managing pancreatic exocrine insufficiency requires a detailed approach. It involves enzyme replacement, nutritional planning, and continuous health monitoring. This condition, where the pancreas fails to produce enough digestive enzymes, necessitates careful management. It’s essential to avoid malnutrition and its complications.
Enzyme Replacement Therapy Protocols
At the heart of managing pancreatic exocrine insufficiency is enzyme replacement therapy (ERT). ERT involves taking supplements with meals to enhance nutrient absorption. The specific dosage and type of supplement depend on the individual’s health and response to treatment.
- Initial dosing is typically based on the fat content of meals.
- Dosage adjustments are made according to the patient’s clinical response.
- Monitoring for signs of malabsorption, such as steatorrhea, is critical.
Nutritional Management and Dietary Considerations
Nutritional management is vital for those with pancreatic exocrine insufficiency. A diet rich in nutrients, tailored to individual needs, helps manage symptoms and prevent complications.
- A high-calorie, high-protein diet may be recommended.
- Fat-soluble vitamin supplements are often necessary.
- Avoiding foods that exacerbate symptoms can help manage the condition.
Monitoring and Adjusting Treatment
Continuous monitoring is essential for adjusting treatment plans. Regular check-ups with healthcare providers are vital. They help assess the effectiveness of enzyme replacement therapy and make necessary adjustments.
With a thorough management plan, individuals with pancreatic exocrine insufficiency can live fulfilling lives. Regular monitoring and treatment adjustments are critical for maintaining optimal health.
The Pancreas and Its Relationship to Other Organ Systems
Understanding the pancreas’ connection to other organ systems is key to grasping its functions and disorders. It doesn’t work alone; it’s deeply tied to various systems, affecting health and disease broadly.
Hepatobiliary Connections
The pancreas is closely tied to the hepatobiliary system, which includes the liver and gallbladder. This connection is vital for digestion, as bile from the liver and gallbladder helps with fat digestion. It works alongside pancreatic enzymes.
- The release of bile into the duodenum is coordinated with pancreatic enzyme secretion.
- Diseases affecting the hepatobiliary system, such as gallstones, can impact pancreatic function.
- The shared ductal system between the pancreas and bile duct can be a pathway for disease transmission.
Gut-Pancreas Axis
The gut-pancreas axis is about the communication between the pancreas and the gastrointestinal tract. This axis is essential for digestive health and metabolic balance.
- The pancreas secretes digestive enzymes into the gut to facilitate nutrient breakdown.
- Gut hormones, such as secretin and cholecystokinin, regulate pancreatic secretion.
- Dysregulation in the gut-pancreas axis can lead to conditions like pancreatitis or malabsorption.
Endocrine System Interactions
The pancreas is a vital part of the endocrine system, mainly through insulin and glucagon production. These hormones are critical for glucose homeostasis, working with other glands to keep metabolism in check.
- Insulin and glucagon have opposing effects on blood glucose levels.
- The pancreas interacts with other endocrine organs, such as the adrenal glands and thyroid, to regulate metabolism.
- Diseases like diabetes mellitus result from dysfunction in the pancreas’ endocrine role.
Preventive Strategies for Optimal Pancreatic Health
Maintaining optimal pancreatic health is vital for overall well-being. Preventive strategies are key to achieving this goal. A holistic approach includes dietary changes, lifestyle adjustments, and regular screenings. These steps can significantly lower the risk of pancreatic disorders.
Dietary Approaches and Nutritional Support
A diet rich in fruits, vegetables, and whole grains is beneficial for pancreatic health. Foods high in antioxidants and fiber help reduce inflammation and support digestive health. It’s wise to limit processed foods and those with high sugar and unhealthy fats.
Lifestyle Modifications and Risk Reduction
Lifestyle choices greatly affect pancreatic health. Avoiding excessive alcohol and quitting smoking are critical to prevent pancreatitis and pancreatic cancer. Regular exercise also boosts overall health and helps manage weight, reducing type 2 diabetes risk.
Screening Recommendations for High-Risk Individuals
Those with a family history of pancreatic cancer or genetic syndromes should consider screening. Early detection through CT scans or MRI can improve outcomes. It’s important for high-risk individuals to consult with a healthcare provider about screening schedules.
Emerging Therapies and Research Frontiers
Emerging therapies are transforming the treatment of pancreatic diseases. Recent breakthroughs in medical research have unveiled new paths for tackling pancreatic disorders. These advancements aim to enhance patient outcomes and improve quality of life.
Regenerative Medicine and Stem Cell Applications
Regenerative medicine, with a focus on stem cell therapy, shows great promise. Scientists are delving into the possibility of stem cells regenerating insulin-producing beta cells. This could potentially cure diabetes.
Artificial Pancreas Development
The creation of an artificial pancreas is a major research focus. This technology seeks to automate insulin delivery, mirroring the pancreas’s natural function. It aims to better manage glucose levels for those with diabetes.
Targeted Molecular Therapies
Targeted molecular therapies are being developed to tackle specific molecular causes of pancreatic diseases. These treatments aim to offer more effective solutions with fewer side effects.
Immunotherapy Approaches
Immunotherapy is being explored for its role in treating pancreatic cancer and autoimmune diabetes. By adjusting the immune system’s response, researchers aim to create more effective treatments. This could lead to better patient outcomes.
The future of pancreatic care looks bright, thanks to these emerging therapies and research areas. Continued research and development are essential. They will help bring these innovations to the clinical setting.
The Future of Pancreatic Care and Patient Outcomes
The field of pancreatic care is rapidly evolving, thanks to breakthroughs in research and treatment methods. New therapies and management strategies are on the horizon, promising better patient outcomes. Innovations like regenerative medicine and targeted molecular therapies are set to improve life quality for those with pancreatic disorders.
For pancreatic care to see improved patient outcomes, continued research investment is critical. Healthcare providers must harness advanced technologies and deepen their understanding of pancreatic diseases. This will enable more personalized and effective care, leading to better management of conditions and enhanced patient well-being.
As pancreatic care advances, prioritizing patient-centered approaches is vital. This focus addresses the complex needs of those with pancreatic diseases. By doing so, we can optimize care and significantly improve patient well-being.
FAQ
Q: What is the primary function of the pancreas?
A: The pancreas plays a vital role with two main functions. It produces hormones like insulin and glucagon, which regulate blood sugar levels. It also secretes digestive enzymes, aiding in digestion.
Q: What are the main causes of acute pancreatitis?
A: Acute pancreatitis is often triggered by gallstones or excessive alcohol consumption. These factors can lead to inflammation of the pancreas.
Q: How is pancreatic cancer diagnosed?
A: Diagnosing pancreatic cancer is complex. It involves imaging techniques like CT, MRI, and endoscopic ultrasound. Blood tests and biomarkers also play a role in detection.
Q: What is pancreatic exocrine insufficiency, and how is it managed?
A: Pancreatic exocrine insufficiency occurs when the pancreas fails to produce enough digestive enzymes. Treatment includes enzyme replacement therapy and adjusting one’s diet.
Q: What are the different types of diabetes related to pancreatic dysfunction?
A: Pancreatic dysfunction can lead to several types of diabetes. Type 1 diabetes results from autoimmune destruction. Type 2 diabetes is caused by insulin resistance and secretory defects. Pancreatic Diabetes, or Type 3c, is a distinct form.
Q: What surgical procedures are used to treat pancreatic conditions?
A: Surgical options for pancreatic conditions include the Whipple procedure, distal pancreatectomy, and total pancreatectomy. These procedures aim to remove affected parts of the pancreas.
Q: How can pancreatic health be maintained or improved?
A: To maintain pancreatic health, adopting a balanced diet and making lifestyle changes are essential. Regular screenings are also recommended for those at high risk.
Q: What emerging therapies are being explored for pancreatic disorders?
A: New treatments for pancreatic disorders include regenerative medicine and artificial pancreas development. Other promising areas are targeted molecular therapies and immunotherapy.















