Parkinson’s Disease: What is Parkinson’s Disease
A neurodegenerative disorder affecting millions worldwide, characterized by tremors, stiffness, and movement difficulties. Understanding this condition is key to developing effective treatments. It’s also vital for improving the quality of life for those affected. This guide aims to offer insights into symptoms, diagnosis, and treatment options. It’s designed to help individuals and caregivers navigate the complexities of the condition. To grasp Parkinson’s Disease, we must explore its definition, history, and how it progresses. It’s a chronic, progressive disorder that mainly impacts movement.
Definition and Classification
Parkinson’s Disease is marked by motor symptoms like tremors, rigidity, slow movement, and balance issues. It’s divided into stages based on symptom severity. The Hoehn and Yahr scale is a common tool for staging, ranging from stage 1 (affecting one side) to stage 5 (requiring bed or wheelchair confinement).
This classification is key for tracking the disease’s progression and planning treatment. It also helps predict the disease’s course and possible complications.

Historical Discovery and Evolution
James Parkinson first described Parkinson’s Disease in 1817 in “An Essay on the Shaking Palsy.” Our understanding of the disease has grown over time. Initially seen as a movement disorder, it’s now known as a complex neurodegenerative condition with motor and non-motor symptoms.
Medical science has made significant strides in understanding Parkinson’s Disease. We’ve learned about genetic and environmental factors in its development. The discovery of dopaminergic system dysfunction and the role of alpha-synuclein protein have been vital in grasping its neurobiology.
Epidemiology and Demographics
The study of Parkinson’s Disease epidemiology uncovers a complex pattern of prevalence and incidence across various demographics. This understanding is critical for effective public health planning and resource allocation.
Global Prevalence and Incidence Rates
Parkinson’s Disease impacts a substantial portion of the global population, with differing prevalence and incidence rates in different regions. Recent studies indicate that about 1% of individuals over 60 worldwide suffer from Parkinson’s Disease. The incidence rates also show variability, with some areas experiencing a higher number of new cases each year.
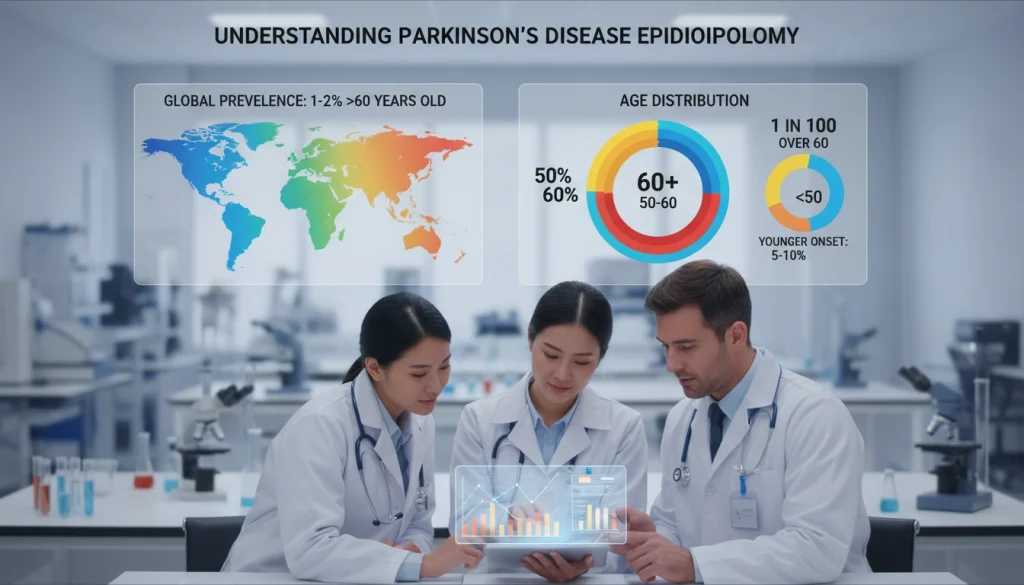
Age, Gender, and Ethnic Distribution
The disease predominantly affects older adults, with incidence rates increasing with age. Research indicates that men are more prone to developing Parkinson’s Disease than women. Also, the disease’s prevalence varies among ethnic groups, with some studies pointing to a higher incidence in specific populations.
These demographic differences underscore the necessity for targeted research and healthcare strategies. They aim to meet the unique needs of different populations affected by Parkinson’s Disease.
Causes and Risk Factors
The exact cause of Parkinson’s Disease is not yet known. Yet, research has identified several risk factors. Grasping these factors is key to creating effective prevention and treatment plans.
Genetic Predisposition
Genetics significantly influence Parkinson’s Disease development. Specific genetic mutations raise the risk of getting the disease. For example, mutations in the SNCA, PARK2, and LRRK2 genes are linked to a higher risk.
Families with a history of Parkinson’s are more likely to see its occurrence. This underlines the role of genetics in the disease.
Environmental Exposures
Environmental factors also play a part in Parkinson’s risk. Exposure to pesticides, herbicides, and industrial chemicals increases the risk. For instance, studies link pesticide exposure to a higher risk of Parkinson’s.
Other Contributing Factors
Other factors may also contribute to Parkinson’s. These include head trauma, certain medications, and lifestyle choices. Severe head injuries and some medications, like antipsychotics, can lead to Parkinsonian symptoms.
Understanding these causes and risk factors is essential. It helps researchers and clinicians develop more effective prevention and treatment strategies for Parkinson’s Disease.
The Neurobiology of Parkinson’s Disease
Parkinson’s Disease’s progression is deeply rooted in brain neurobiology, with a focus on the dopaminergic system. Grasping these changes is key to understanding the disease’s symptoms and progression.
Dopaminergic System Dysfunction
Parkinson’s Disease is marked by the degeneration of dopaminergic neurons in the substantia nigra. This area is vital for movement control. The loss of these neurons significantly reduces dopamine production, leading to symptoms like tremors, stiffness, and slow movement.
The dopaminergic system’s complexity extends beyond dopamine production. It involves regulation and signaling within the brain. Dysfunction here disrupts motor function, driving the disease’s progression.
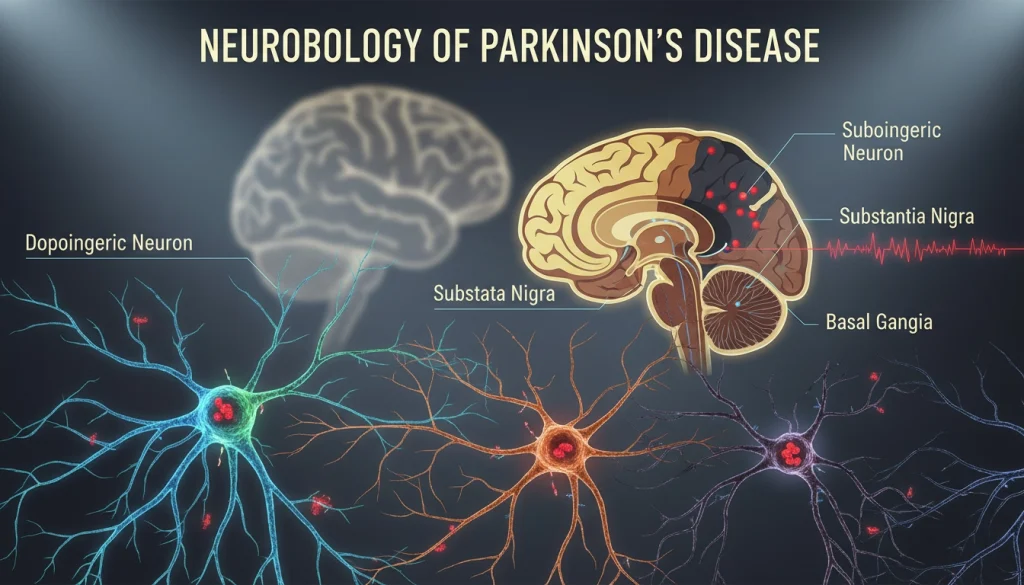
Alpha-Synuclein and Lewy Bodies
Alpha-synuclein protein accumulation and Lewy body formation are critical in Parkinson’s Disease neurobiology. Abnormal alpha-synuclein aggregation forms Lewy bodies, hallmark pathological features of the disease.
Lewy bodies serve as diagnostic markers and are thought to contribute to disease progression. They may disrupt cellular function and contribute to neurodegeneration.
Neuroinflammation and Oxidative Stress
Neuroinflammation and oxidative stress are significant in Parkinson’s Disease neurobiology. Neuroinflammation activates brain immune cells, releasing substances that worsen neuronal damage.
Oxidative stress results from an imbalance between reactive oxygen species (ROS) production and detoxification. This imbalance causes cellular damage. Both neuroinflammation and oxidative stress contribute to dopaminergic neuron degeneration, impairing motor function.
Early Warning Signs
Recognizing the early warning signs of Parkinson’s Disease is key to managing it effectively. Early detection leads to timely intervention, which can slow the disease’s progression. It’s important for individuals to be aware of the subtle indicators that may signal Parkinson’s onset.
Subtle Motor Symptoms
Subtle motor symptoms are among the first signs of Parkinson’s Disease. These include slight tremors, stiffness, or rigidity in the limbs, and a decrease in facial expressions. Changes in gait, such as a slower pace or smaller steps, are also common. If you or a loved one suspects these symptoms, seeking a specialist’s opinion is wise. Medical attention can offer clarity and treatment options.
Non-Motor Prodromal Signs
Non-motor prodromal signs also precede Parkinson’s Disease diagnosis by years. These include constipation, loss of smell (anosmia), and sleep disturbances like REM sleep behavior disorder. Recognizing these non-motor symptoms early can lead to earlier medical evaluation and diagnosis.
Understanding and recognizing these early warning signs are vital for managing Parkinson’s Disease. Being vigilant about both subtle motor symptoms and non-motor prodromal signs allows individuals to take proactive steps towards their health.
Clinical Manifestations of Parkinson’s Disease
Parkinson’s Disease shows a wide range of symptoms in different people. Motor symptoms like bradykinesia, tremors, and postural instability are common. These symptoms are key to identifying the disease.
Non-motor symptoms, including cognitive decline, mood disorders, and autonomic dysfunction, also impact the disease’s progression. It’s vital to understand all symptoms to offer the best care to patients.
Managing Parkinson’s Disease effectively requires a team effort. Healthcare providers must address both motor and non-motor symptoms. Recognizing the variety of symptoms helps in creating tailored treatment plans. This approach improves the quality of life for those with Parkinson’s Disease.
FAQ
Q: What is Parkinson’s Disease?
A: Parkinson’s Disease is a chronic, progressive disorder that mainly affects movement. It is characterized by tremors, stiffness, and difficulty in movement.
Q: What are the early warning signs of Parkinson’s Disease?
A: Early signs include subtle motor symptoms like tremors and rigidity. Non-motor signs include constipation, loss of smell, and sleep disturbances.
Q: What causes Parkinson’s Disease?
A: The exact cause is unknown, but several risk factors have been identified. These include genetic predisposition, environmental exposures, and head trauma. Certain medications also play a role.
Q: How is Parkinson’s Disease diagnosed?
A: Diagnosis involves evaluating motor and non-motor symptoms, medical history, and physical examination. There is no single definitive test.
Q: What are the treatment options for Parkinson’s Disease?
A: Treatments include medications like levodopa and dopamine agonists, deep brain stimulation, physical therapy, and lifestyle changes. These aim to manage symptoms and improve quality of life.
Q: Can Parkinson’s Disease be cured?
A: There is no cure, but treatments and therapies can manage symptoms and slow progression.
Q: How does Parkinson’s Disease affect daily life?
A: It significantly impacts mobility, balance, and cognitive function. It also causes non-motor symptoms like depression and anxiety.
Q: What is the role of dopamine in Parkinson’s Disease?
A: Dopamine is essential for movement control. Its depletion leads to motor symptoms in Parkinson’s Disease.
Q: Are there any ongoing research or clinical trials for Parkinson’s Disease?
A: Yes, research includes gene therapy, stem cell therapy, and immunotherapy. These aim to slow or halt disease progression.















