Pelvic Pain and Dysfunction: Understanding Pelvic Pain and Dysfunction
Chronic Pelvic Pain affects millions globally, causing significant discomfort and daily life impairment. It’s characterized by persistent pain in the pelvic area, often with urinary or sexual dysfunction symptoms. Understanding the causes and effective management of Pelvic Dysfunction is key to improving life quality for those affected. This guide aims to provide a detailed look at the condition, its diagnosis, and available treatments.
We will explore the latest research and expert insights into this complex condition. Our goal is to offer guidance for those seeking relief from Chronic Pelvic Pain. Pelvic pain and dysfunction are complex conditions affecting millions globally. They cause significant discomfort and daily life impairment. These conditions present in various forms, making diagnosis and treatment challenging.
Definition and Prevalence
Pelvic pain is pain perceived from the pelvic region, lasting more than six months for chronic cases. Chronic pelvic pain affects about 15% to 20% of women of reproductive age. Men’s prevalence is less studied but recognized as a significant issue.
The need for greater awareness and understanding of these conditions is highlighted by their prevalence. Gynecological, urological, gastrointestinal, and musculoskeletal issues contribute to pelvic pain development.
Impact on Quality of Life
Pelvic pain and dysfunction significantly impact an individual’s quality of life. Symptoms can range from mild discomfort to severe pain, affecting daily activities and sexual function. Chronic pelvic pain can also lead to emotional distress, anxiety, and depression.
Healthcare providers must understand the multifaceted nature of pelvic pain and its quality of life impact. Treatment plans should address physical symptoms, psychological, and social implications.
Anatomy of the Pelvic Region
The pelvic region’s anatomy is complex, involving bones, muscles, nerves, and blood vessels. This complexity supports functions like locomotion, continence, and reproduction. It’s essential for the body’s overall health.
Pelvic Bones and Muscles
The pelvic bones are the foundation, made up of the ilium, ischium, and pubis bones. These bones merge to form the acetabulum and the pelvic ring. The pelvic muscles, like the levator ani and coccygeus, are key. They support pelvic organs and help maintain continence.
- The ilium is the largest bone, forming the superior part of the pelvis.
- The ischium bears the body’s weight when sitting and is vital for pelvic stability.
- The pubis bone forms the front of the pelvis, connecting the two pubic bones at the symphysis pubis.
Nerves and Blood Supply
The pelvic region is richly innervated by nerves. These nerves control functions like involuntary actions and voluntary movements. The blood supply comes from the internal iliac artery’s branches. This ensures the pelvic organs get enough oxygen and nutrients.
- The pudendal nerve is a key nerve that supplies the external genitalia and perineum.
- The autonomic nerves, including the sympathetic and parasympathetic nerves, regulate pelvic organ function.
- The internal iliac artery branches into several arteries that supply the pelvic organs.
Types of Pelvic Pain
Pelvic pain is a complex condition with various types and characteristics. It’s vital to understand these differences for accurate diagnosis and treatment. The type of pelvic pain can vary greatly among individuals. It’s influenced by factors like the cause, duration, and intensity of the pain.
Acute vs. Chronic Pelvic Pain
Pelvic pain is divided into acute and chronic types based on duration. Acute pain lasts less than three to six months, often due to injury, infection, or surgery. Chronic pain, lasting more than six months, can stem from musculoskeletal disorders, gynecological issues, or gastrointestinal problems.
It’s critical to differentiate between acute and chronic pelvic pain for the right treatment. Acute pain usually resolves with treatment of the underlying cause. Chronic pain, on the other hand, requires a more extensive management plan. This may include medication, physical therapy, and lifestyle changes.
Referred Pain Patterns
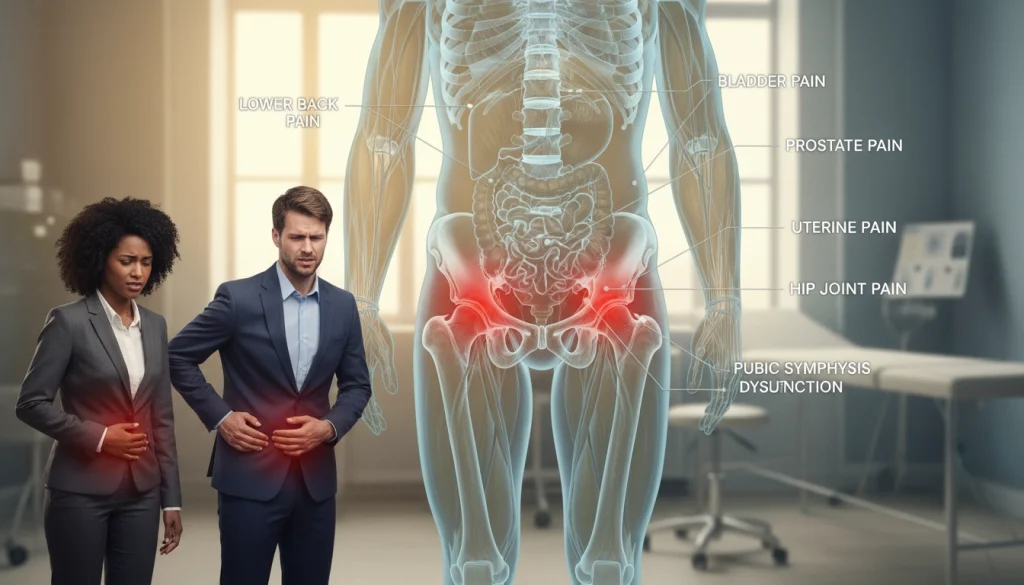
Referred pain occurs when pain is felt in a different location than the source. In pelvic pain, referred pain patterns are common due to the complex innervation of the area. For example, pain from pelvic organs can be felt in the lower back, thighs, or lower abdomen.
Understanding referred pain patterns is key to diagnosing pelvic pain’s cause. Healthcare providers must consider referred pain when diagnosing. A detailed medical history and physical examination are necessary to pinpoint the pain’s source.
Common Causes of Pelvic Pain in Women
Women dealing with pelvic pain often face a variety of causes. These can range from gynecological issues to pregnancy-related complications. It’s vital to grasp these causes for effective diagnosis and treatment.
Gynecological Conditions
Gynecological conditions are a major source of pelvic pain in women. These can vary from mild to severe. They affect the reproductive organs in different ways.
Endometriosis and Adenomyosis
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus. This leads to pain and discomfort. Adenomyosis involves endometrial tissue growing into the uterine wall, causing painful periods and pelvic pain. Both are significant causes of pelvic pain in women.
Pelvic Inflammatory Disease
Pelvic inflammatory disease (PID) is an infection of the female reproductive organs. It’s usually caused by sexually transmitted bacteria. If not treated quickly, it can lead to chronic pelvic pain. PID is a serious condition that needs immediate medical attention to prevent long-term issues.
Pregnancy-Related Pelvic Pain
Pregnancy-related pelvic pain is another common issue. It arises from changes in the pelvic structure and strain on muscles and ligaments. As the uterus expands, the pain can vary in intensity. Various treatments, including physical therapy, can help manage this pain.
Women experiencing pelvic pain should seek healthcare providers for a proper diagnosis. Understanding the underlying causes is key. This way, women can receive the right treatment, significantly improving their quality of life.
Common Causes of Pelvic Pain in Men
Understanding the common causes of pelvic pain in men is key to managing and treating it effectively. This pain can stem from infections, structural issues, or referred pain from other areas.
Prostatitis
Prostatitis is the inflammation of the prostate gland, a common source of pelvic pain in men. Symptoms include pelvic pain, difficulty urinating, and painful ejaculation. There are several types, including acute bacterial, chronic bacterial, and chronic prostatitis/chronic pelvic pain syndrome.
- Pain or burning sensation while urinating
- Frequent urination
- Pain in the pelvic area, genitals, or lower back
Testicular and Scrotal Disorders
Testicular and scrotal disorders are major causes of pelvic pain in men. Conditions like epididymitis, orchitis, and testicular torsion can cause severe pain. These often come with swelling, redness, or tenderness of the scrotum.
- Epididymitis: Inflammation of the epididymis, often due to infection
- Orchitis: Inflammation of one or both testicles, usually caused by bacterial or viral infections
- Testicular torsion: A medical emergency where the spermatic cord becomes twisted
Musculoskeletal Sources of Pelvic Dysfunction
Understanding the musculoskeletal causes of pelvic dysfunction is key to effective treatment. Issues in the musculoskeletal system can lead to pelvic pain and dysfunction. This affects many areas of an individual’s life, impacting their quality of life significantly.
Pelvic Floor Muscle Dysfunction
Pelvic floor muscle dysfunction is a common cause of pelvic pain. It involves the muscles and tissues that support the pelvic organs. This condition can arise from muscle tension, trauma, or neurological problems.
- Symptoms include pain in the pelvic region, lower back, or during intercourse.
- Pelvic floor physical therapy is a common treatment approach, focusing on relaxation and strengthening exercises.
- Behavioral modifications, such as dietary changes and stress management, can also be beneficial.
Pelvic floor muscle dysfunction can be associated with various factors, including:
- Chronic constipation or straining during bowel movements.
- Pregnancy and childbirth.
- Surgical interventions in the pelvic region.
Sacroiliac Joint Dysfunction
Sacroiliac joint dysfunction is another significant musculoskeletal source of pelvic pain. The sacroiliac joint connects the sacrum to the ilium bones, playing a critical role in weight transfer and stability.
Dysfunction in this joint can cause pain in the lower back and buttocks, potentially radiating down the legs. Common causes include:
- Trauma or injury to the joint.
- Arthritis or degenerative changes.
- Asymmetrical movement patterns or biomechanical issues.
Treatment for sacroiliac joint dysfunction may involve:
- Manual therapy techniques, such as joint mobilization.
- Strengthening exercises for the surrounding muscles.
- Supportive devices or orthotics to improve joint stability.
Gastrointestinal and Urological Causes
Understanding the causes of pelvic pain in the gastrointestinal and urological systems is key. Conditions like Irritable Bowel Syndrome (IBS) and Interstitial Cystitis (IC) often lead to this pain. These disorders affect the body’s ability to function properly.
Irritable Bowel Syndrome
Irritable Bowel Syndrome (IBS) is a chronic condition affecting the gut. It causes persistent abdominal pain, discomfort, and irregular bowel movements. Symptoms can vary but often include bloating, gas, diarrhea, or constipation.
The exact cause of IBS is not known. Yet, changes in gut bacteria, nervous system issues, and early life stress are thought to play a role. IBS can greatly reduce a person’s quality of life, leading to pelvic pain and discomfort.
Managing IBS involves making dietary changes, managing stress, and sometimes using medication. These strategies aim to alleviate symptoms and improve overall well-being.
Interstitial Cystitis
Interstitial Cystitis (IC), also known as painful bladder syndrome, causes bladder pressure and pain. Symptoms can range from mild to severe, affecting the pelvic area. The exact cause of IC is not fully understood, but it’s believed to involve a defect in the bladder’s protective lining.
Treatment for IC includes lifestyle changes, physical therapy, and medications. These interventions aim to reduce symptoms and improve bladder health. The goal is to alleviate pain and discomfort.
Diagnosis of Pelvic Pain and Dysfunction
To accurately diagnose pelvic pain and dysfunction, healthcare providers must employ a multifaceted strategy. This includes medical history, physical examination, and various diagnostic tests. This approach is essential for identifying the underlying causes of pelvic pain and developing an effective treatment plan.
Medical History and Physical Examination
The initial step in diagnosing pelvic pain involves taking a detailed medical history. This includes questioning the patient about the onset, duration, and characteristics of their pain. It also involves asking about any factors that exacerbate or relieve it. A thorough physical examination is also essential, involving both a general examination and a focused pelvic examination to assess for any abnormalities or tenderness.
The physical examination may include a musculoskeletal assessment. This evaluates the pelvic floor muscles, sacroiliac joints, and lower back. It helps identify any musculoskeletal sources of pain or dysfunction.
Imaging and Laboratory Tests
Imaging tests play a critical role in the diagnosis of pelvic pain and dysfunction. Techniques such as ultrasound, MRI, and CT scans can help identify structural abnormalities. These include endometriosis, ovarian cysts, or pelvic organ prolapse. Laboratory tests, including blood work and urinalysis, can help diagnose infections, inflammatory conditions, or other underlying causes of pelvic pain.
Specialized Diagnostic Procedures
In some cases, specialized diagnostic procedures may be necessary. These include laparoscopy, a minimally invasive surgical procedure that allows direct visualization of the pelvic organs. Cystoscopy, which involves examining the inside of the bladder, is also used. These procedures can help diagnose conditions such as endometriosis, adhesions, or interstitial cystitis.
By combining information from the medical history, physical examination, imaging and laboratory tests, and specialized diagnostic procedures, healthcare providers can develop a complete understanding of the patient’s condition. They can then create an effective treatment plan.
Medical Treatment Approaches
Medical treatments for pelvic pain and dysfunction vary, aiming to reduce symptoms and enhance life quality. The treatment choice hinges on the cause, severity, and how the condition affects the patient’s life.
Pharmacological Interventions
Pharmacological treatments are often the initial approach for pelvic pain and dysfunction. This includes pain relievers, hormonal therapies, and muscle relaxants. Pain relievers like NSAIDs or acetaminophen can lessen pain and inflammation. Hormonal therapies are used for conditions like endometriosis. Muscle relaxants help with pelvic floor muscle spasms.
The choice of pharmacological treatment depends on the diagnosis, patient history, and possible side effects. For instance, hormonal therapies are more frequently used for gynecological causes of pelvic pain.
Minimally Invasive Procedures
When pharmacological treatments are not enough, minimally invasive procedures offer a good alternative. These procedures aim to reduce recovery time and minimize scarring. Examples include injections for pain management, nerve blocks, and certain types of laparoscopic surgery.
Nerve blocks can provide temporary or sometimes long-term relief by blocking pain signals to the brain. Laparoscopic surgery is used for diagnosing and treating conditions like endometriosis or adhesions.
Surgical Options
Surgical options are considered when other treatments have failed or when the underlying cause requires surgery. Surgical procedures can range from removing the source of pain, such as endometriotic lesions, to more complex operations like hysterectomy in severe cases.
The decision to proceed with surgery is made after weighing the benefits and risks. Surgical options are often reserved for cases where the condition significantly impacts the patient’s quality of life.

In conclusion, the medical treatment approaches for pelvic pain and dysfunction are diverse and tailored to the individual’s condition. A healthcare provider collaborates with the patient to determine the most suitable treatment plan. This may include a combination of pharmacological interventions, minimally invasive procedures, and surgical options.
Physical Therapy for Pelvic Pain and Dysfunction
Pelvic pain and dysfunction can be effectively managed through targeted physical therapy interventions. This non-invasive treatment approach focuses on addressing the musculoskeletal and biomechanical aspects of pelvic pain.
Manual Therapy Techniques
Manual therapy techniques are a cornerstone of physical therapy for pelvic pain. These techniques include:
- Myofascial release to relax tense muscles and improve tissue mobility
- Trigger point therapy to address specific areas of muscle tension
- Joint mobilization to improve pelvic joint mobility and reduce pain
These manual techniques can help in reducing pain and improving the overall function of the pelvic region.
Therapeutic Exercises
Therapeutic exercises are another critical component of physical therapy for pelvic pain. These exercises are designed to:
- Strengthen the pelvic floor muscles
- Improve flexibility and range of motion
- Enhance core stability and posture
By strengthening the muscles that support the pelvic organs and improving overall pelvic stability, therapeutic exercises can significantly reduce pelvic pain.
Biofeedback and Electrical Stimulation
Biofeedback and electrical stimulation are advanced techniques used in physical therapy to manage pelvic pain. Biofeedback helps patients become aware of their pelvic floor muscle activity, allowing them to learn how to relax or contract these muscles appropriately. Electrical stimulation involves the use of gentle electrical currents to stimulate muscle contractions and can be helpful in strengthening weak pelvic floor muscles.
Together, these physical therapy interventions offer a holistic approach to managing pelvic pain and dysfunction. They improve the quality of life for individuals affected by these conditions.
Psychological Aspects and Mental Health
Pelvic pain and dysfunction significantly affect mental health, going beyond physical pain. Living with chronic pelvic pain can cause frustration, anxiety, and depression. These feelings can greatly reduce a person’s quality of life.
Chronic Pain and Psychological Impact
Chronic pelvic pain is more than a physical issue; it deeply affects mental well-being. The ongoing pain can cause emotional strain, making people feel isolated and withdrawn. This psychological impact can be as severe as the physical pain, impacting relationships, work, and overall well-being.
The relationship between chronic pain and mental health is complex. Pain can worsen anxiety and depression, which in turn can increase pain perception. Breaking this cycle requires support and treatment.
Cognitive Behavioral Therapy and Other Approaches
Cognitive Behavioral Therapy (CBT) is key in managing the mental side of chronic pelvic pain. CBT helps individuals change negative thought patterns and behaviors that add to their distress. This can help them cope with pain and improve their mental health.
Other methods, like mindfulness-based stress reduction and psychological counseling, are also helpful. These therapies give people tools to manage pain and related mental distress more effectively.
Recognizing the mental impact of pelvic pain and using the right therapies can lead to better care. Healthcare providers can significantly improve the quality of life for those with chronic pelvic pain by doing so.
Complementary and Alternative Approaches
Many seek relief from pelvic pain through complementary and alternative therapies. These methods can enhance conventional treatments, providing extra relief.

Acupuncture and Traditional Chinese Medicine
Acupuncture, a cornerstone of traditional Chinese medicine, involves inserting fine needles into body points. It aims to stimulate the body’s healing processes and enhance pain management.
- Studies indicate acupuncture can lessen pain and enhance life quality for some.
- Traditional Chinese medicine also includes herbal remedies and other therapies, complementing standard treatments.
Mind-Body Techniques
Mind-body techniques, like meditation, yoga, and cognitive behavioral therapy, tackle pelvic pain’s psychological facets. They help manage chronic pain.
- Meditation and mindfulness lower stress and boost pain tolerance.
- Yoga combines physical activity with deep breathing, improving flexibility and reducing pain.
- Cognitive behavioral therapy (CBT) aids in managing chronic pain by altering how individuals perceive and deal with pain.
Incorporating these complementary and alternative methods into treatment plans can offer more relief and better quality of life for those with pelvic pain and dysfunction.
Living with Chronic Pelvic Pain: Moving Forward
Dealing with chronic pelvic pain is tough, but there are ways to manage it and enhance life quality. Effective Chronic Pelvic Pain Management requires a multi-faceted approach. This includes medical treatment, physical therapy, and lifestyle adjustments.
Creating a detailed treatment plan is essential for Living with Pelvic Pain. This might involve medication, physical therapy like manual therapy and exercises, and alternative methods like acupuncture and mind-body techniques.
Managing chronic pelvic pain also means making lifestyle changes. Keeping a healthy weight, exercising regularly, and using stress-reducing techniques can improve well-being. Seeking support from healthcare professionals, support groups, and loved ones is also vital. It offers emotional support and helps cope with the psychological effects of chronic pain.
By adopting a proactive and holistic approach to managing chronic pelvic pain, individuals can enhance their quality of life. With the right strategies and support, it’s possible to lessen the impact of chronic pelvic pain and live a more fulfilling life.
FAQ
Q: What is pelvic pain and dysfunction?
A: Pelvic pain and dysfunction encompass a variety of conditions. They cause pain or discomfort in the pelvic area. Often, these issues also affect bowel, bladder, or sexual functions.
Q: How common is pelvic pain?
A: Pelvic pain is quite common, affecting millions globally. It significantly impacts one’s quality of life.
Q: What are the main causes of pelvic pain in women?
A: Women often experience pelvic pain due to gynecological issues. These include endometriosis, adenomyosis, and pelvic inflammatory disease. Pregnancy-related pain is another common cause.
Q: What are the common causes of pelvic pain in men?
A: Men commonly face pelvic pain from conditions like prostatitis. Testicular and scrotal disorders also contribute to this issue.
Q: How is pelvic pain diagnosed?
A: Diagnosing pelvic pain involves a detailed medical history and physical exam. Imaging and lab tests are also used. Sometimes, specialized procedures are necessary.
Q: What are the treatment options for pelvic pain and dysfunction?
A: Treatment options include pharmacological interventions and minimally invasive procedures. Surgical options, physical therapy, and alternative therapies are also available.
Q: How can physical therapy help with pelvic pain?
A: Physical therapy uses manual therapy, exercises, biofeedback, and electrical stimulation. These methods help manage pelvic pain.
Q: Can pelvic pain be related to gastrointestinal or urological issues?
A: Yes, conditions like irritable bowel syndrome and interstitial cystitis can cause pelvic pain. These are gastrointestinal and urological issues, respectively.
Q: What role does mental health play in managing pelvic pain?
A: Mental health is critical in managing pelvic pain. Chronic pain can have a significant psychological impact. Cognitive behavioral therapy and other mental health approaches are essential.
Q: Are there any alternative therapies that can help with pelvic pain?
A: Yes, alternative therapies like acupuncture and traditional Chinese medicine may help. Mind-body techniques also offer relief for some individuals with pelvic pain.















