PFAPA Syndrome: What Is PFAPA Syndrome?
PFAPA Syndrome is a rare periodic fever disorder mainly affecting children. It is marked by recurring fever episodes. Symptoms can include sore throat, mouth ulcers, and swollen lymph nodes. This condition can severely impact the quality of life for those affected. It causes discomfort and disrupts daily activities. Understanding PFAPA Syndrome is vital for diagnosis and management. This allows healthcare providers to offer the right care and support.
Given its rarity, it’s critical to raise awareness and knowledge about PFAPA Syndrome. This is key for early detection and effective treatment strategies. PFAPA Syndrome, short for Periodic Fever, Aphthous Stomatitis, Pharyngitis, and Adenitis, is a rare autoinflammatory disorder. It is marked by recurring fever episodes, often paired with mouth ulcers, sore throat, and swollen lymph nodes.
Definition and Classification
PFAPA Syndrome is classified as a periodic fever syndrome, a group of disorders with recurring fever episodes. It is diagnosed by ruling out other fever causes. Its classification hinges on specific clinical features, like the periodic fever and associated symptoms.
To diagnose PFAPA Syndrome, one must see periodic fever, aphthous stomatitis, pharyngitis, and cervical adenitis without other fever causes.
Historical Background and Discovery
PFAPA Syndrome was first documented in the late 20th century. Marshall et al. identified it in 1987, noting children with periodic fever, aphthous stomatitis, pharyngitis, and adenitis. The recognition of PFAPA Syndrome as a distinct entity has grown, with ongoing research into its causes and treatment.
The discovery of PFAPA Syndrome has greatly advanced our understanding of it. It shows the need for continued research into rare and complex conditions.
The Epidemiology of PFAPA Syndrome
PFAPA Syndrome epidemiology is a critical area of study that sheds light on the frequency and distribution of the disorder. This knowledge is vital for healthcare providers and researchers aiming to understand and manage the condition effectively.
Prevalence and Incidence Rates
Studies on the prevalence and incidence of PFAPA Syndrome have shown varying results. This is largely due to differences in population demographics and diagnostic criteria. Despite this, it is generally considered a relatively rare condition. The reported incidence varies geographically.
Research indicates that PFAPA Syndrome is one of the most common periodic fever syndromes in children. This highlights its significance in pediatric medicine.
Demographic Distribution and Risk Factors
The demographic distribution of PFAPA Syndrome reveals that it predominantly affects children, often beginning before the age of five. There is evidence suggesting a slight male predominance. Risk factors for developing PFAPA Syndrome are not fully understood.
Familial cases have been reported, suggesting a possible genetic component. This indicates that genetic factors may play a role in the development of PFAPA Syndrome.
Understanding the Pathophysiology
The pathophysiology of PFAPA Syndrome involves a complex interplay between genetic predisposition and immune system dysregulation. This condition is marked by recurrent fever, aphthous stomatitis, pharyngitis, and cervical adenitis. These symptoms suggest an abnormal immune response.
Immune System Involvement
The immune system’s role in PFAPA Syndrome is critical, with evidence showing an imbalance in the inflammatory response. During episodes, inflammatory cytokines surge, leading to symptoms like fever and swollen lymph nodes.
The triggers for these inflammatory episodes are not fully understood. Research indicates that an inappropriate activation of the innate immune system may be responsible. The innate immune system acts as the body’s first defense, and its dysregulation can cause excessive inflammation.
Genetic Factors and Inheritance Patterns
Genetic factors are key in PFAPA Syndrome susceptibility. While it’s not strictly hereditary, there may be a genetic predisposition. Research into familial cases has shed light on possible genetic mechanisms. Yet, a specific gene or set of genes responsible for PFAPA Syndrome remains unknown.
The inheritance pattern of PFAPA Syndrome is not straightforward. Some families show a pattern suggesting autosomal dominant inheritance, but this is not universal. Further genetic studies are essential to understand PFAPA Syndrome’s hereditary aspects.
Key Clinical Features of PFAPA Syndrome
Understanding PFAPA Syndrome’s key clinical features is vital for accurate diagnosis and effective management. This condition is marked by recurring symptoms that can severely impact an individual’s quality of life.
Periodic Fever Patterns
PFAPA Syndrome is characterized by periodic fevers. These fevers are high, often over 39°C (102.2°F), and can last several days. Fever episodes are accompanied by other symptoms and recur at regular intervals.
- Fevers can occur as frequently as every 2-4 weeks.
- The duration of fever episodes can vary but typically lasts 3-5 days.
- Fever episodes are often associated with significant discomfort and other systemic symptoms.
Aphthous Stomatitis (Mouth Ulcers)
Aphthous stomatitis, or mouth ulcers, is another common feature of PFAPA Syndrome. These ulcers can be painful and may cause difficulty eating or drinking during fever episodes.
- Mouth ulcers are typically shallow and can occur on the tongue, lips, or elsewhere inside the mouth.
- They often resolve on their own within a week or so after the fever episode subsides.
Pharyngitis (Sore Throat)
Pharyngitis, or sore throat, is a frequent complaint during PFAPA Syndrome episodes. The sore throat can be severe and is often associated with difficulty swallowing.
- The pharyngitis is usually accompanied by inflammation and redness of the throat.
- Symptoms can be managed with supportive care, such as hydration and throat lozenges.
Cervical Adenitis (Swollen Lymph Nodes)
Cervical adenitis, characterized by swollen lymph nodes in the neck, is a common finding in PFAPA Syndrome. This symptom can be quite pronounced during fever episodes.
The swollen lymph nodes are typically tender to the touch and can be a source of discomfort.
Recognizing PFAPA Syndrome Symptoms
Identifying PFAPA Syndrome symptoms is key to early diagnosis and treatment. This rare autoinflammatory disorder is marked by recurring fever episodes, often paired with other symptoms.
Primary Symptoms and Presentation
The main symptoms of PFAPA Syndrome include recurring fever episodes. These can be accompanied by mouth ulcers, sore throat, and swollen lymph nodes. The severity and frequency of these symptoms can vary.
- Periodic fever episodes
- Aphthous stomatitis (mouth ulcers)
- Pharyngitis (sore throat)
- Cervical adenitis (swollen lymph nodes)
These primary symptoms are typically seen during fever episodes and are a hallmark of PFAPA Syndrome.
Secondary and Associated Symptoms
Some individuals with PFAPA Syndrome may also experience secondary symptoms. These can include headache, fatigue, abdominal pain, and nausea. The presence and severity of these symptoms can vary widely among those affected.
- Headache
- Fatigue
- Abdominal pain
- Nausea
Understanding all symptoms of PFAPA Syndrome is vital for effective management and care.
The Diagnostic Journey
The journey to diagnose PFAPA Syndrome is complex, requiring a detailed approach. It involves a thorough clinical evaluation, a review of the patient’s medical history, and adherence to established diagnostic criteria. This ensures an accurate identification of the condition.
Clinical Criteria for Diagnosis
Diagnosing PFAPA Syndrome relies heavily on clinical criteria. These include recurrent fever, aphthous stomatitis, pharyngitis, and cervical adenitis. These symptoms recur at regular intervals, significantly affecting the patient’s quality of life.
- Recurrent fever episodes
- Aphthous stomatitis (mouth ulcers)
- Pharyngitis (sore throat)
- Cervical adenitis (swollen lymph nodes)
Differential Diagnosis Considerations
When diagnosing PFAPA Syndrome, it’s important to rule out other periodic fever syndromes and autoinflammatory disorders. Conditions like Familial Mediterranean Fever (FMF), Hyper-IgD Syndrome (HIDS), and Tumor Necrosis Factor Receptor-Associated Periodic Syndrome (TRAPS) must be considered. This involves both clinical assessment and laboratory tests.

Diagnostic Challenges and Misdiagnosis
Despite clear clinical criteria, diagnosing PFAPA Syndrome can be tricky, leading to misdiagnosis. The condition’s similarity to other periodic fever syndromes and the absence of a specific diagnostic test add to these challenges. A meticulous, patient-focused approach is critical for accurate diagnosis and management.
PFAPA Syndrome vs. Other Periodic Fever Disorders
Understanding the differences between PFAPA Syndrome and other periodic fever disorders is key. These conditions share some traits, but each has unique characteristics that help in diagnosis.
Familial Mediterranean Fever (FMF)
Familial Mediterranean Fever is a genetic disorder that causes recurring fever, serositis, and synovitis. It’s triggered by mutations in the MEFV gene. Unlike PFAPA, FMF often includes abdominal pain and arthritis.
Hyper-IgD Syndrome (HIDS)
Hyper-IgD Syndrome is a rare genetic disorder linked to MVK gene mutations. It’s marked by recurring fever, abdominal pain, diarrhea, and skin issues. HIDS is different from PFAPA due to its early onset and high IgD levels.
Tumor Necrosis Factor Receptor-Associated Periodic Syndrome (TRAPS)
TRAPS is an autosomal dominant disorder caused by TNFRSF1A gene mutations. It’s known for prolonged fever episodes, abdominal pain, and skin issues. TRAPS stands out from PFAPA with its longer fever episodes and rash and eye symptoms.
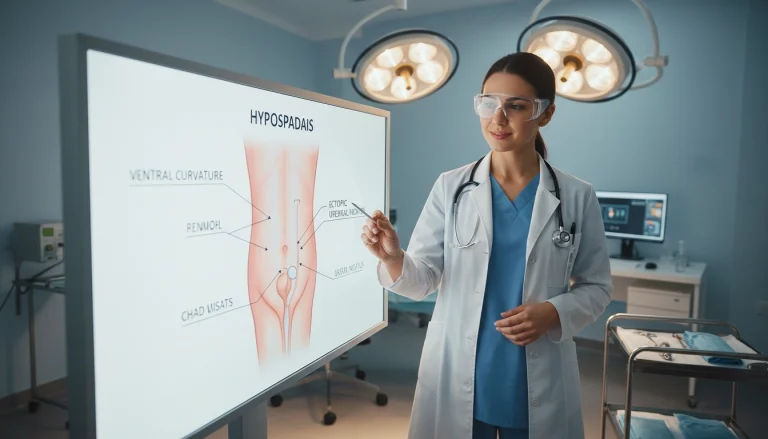
Laboratory and Imaging Studies
Laboratory and imaging studies are essential in diagnosing PFAPA Syndrome. They help doctors confirm the condition and exclude other causes of symptoms.
Blood Tests and Inflammatory Markers
Blood tests are key in assessing inflammation and identifying PFAPA Syndrome markers. Important tests include:
- Complete Blood Count (CBC)
- C-Reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR)
- Genetic Testing
Complete Blood Count (CBC)
A CBC checks the patient’s overall health and detects blood cell count abnormalities. These can signal inflammation or infection.
C-Reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR)
CRP and ESR are markers of inflammation. They are often high during PFAPA Syndrome episodes, showing an active inflammatory process.
Genetic Testing
Genetic testing is not always used for diagnosis. It may be considered to find genetic mutations linked to PFAPA Syndrome or other periodic fever syndromes.
Role of Imaging in Diagnosis
Imaging, like ultrasound or CT scans, helps evaluate inflammation in the throat and lymph nodes. This is during episodes of pharyngitis and cervical adenitis.
Treatment Approaches for PFAPA Syndrome
PFAPA Syndrome treatment aims to reduce symptoms and enhance life quality. Given its unpredictable nature and varied symptoms, a personalized management strategy is essential.
Medication Options
Several treatments are available for PFAPA Syndrome, each with its own advantages and drawbacks.
Corticosteroids
Corticosteroids are commonly used to stop fever episodes and lessen symptoms. They work well for most but can lead to side effects with prolonged use.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs help manage fever and pain during PFAPA Syndrome episodes. Yet, their effectiveness varies among patients.
Colchicine and Other Medications
Colchicine is sometimes used to decrease episode frequency. Other treatments may be explored based on the patient’s symptoms and initial treatment response.
- Corticosteroids: Effective for aborting fever episodes
- NSAIDs: Useful for managing fever and pain
- Colchicine: May reduce episode frequency
Surgical Interventions: Tonsillectomy and Adenoidectomy
In some instances, removing the tonsils and adenoids (tonsillectomy and adenoidectomy) is considered. This is often for those who don’t respond to medication or have severe symptoms.
Choosing surgery should be a careful decision, weighing the benefits against the risks for each patient.
Managing PFAPA Syndrome in Children
Managing PFAPA Syndrome in children demands a holistic strategy. It involves schools, healthcare providers, and families. This condition, marked by periodic fever, aphthous stomatitis, pharyngitis, and cervical adenitis, severely affects a child’s quality of life and academic performance.
School Considerations and Accommodations
Children with PFAPA Syndrome require school accommodations to manage their condition effectively. This might include flexible attendance policies, allowing rest during fever episodes, and providing a quiet space for recovery. Teachers and school staff should be well-informed about the condition to offer the necessary support.
Supportive Care During Fever Episodes
Supportive care is essential during fever episodes to ensure the child’s comfort and safety. This includes hydration, rest, and possibly medication to manage fever and pain. Parents should have a plan for emergency situations, knowing when to seek medical attention.
Communication with Healthcare Providers and Schools
Effective communication between healthcare providers, schools, and families is critical for managing PFAPA Syndrome. Regular updates on the child’s condition, treatment plans, and any necessary accommodations should be shared among all parties. This ensures a cohesive care approach.
PFAPA Syndrome in Adults
PFAPA Syndrome is not just a childhood issue; it can also affect adults. It’s important to understand how it presents and is managed in adults to ensure proper care.
Differences from Pediatric Presentation
In adults, PFAPA Syndrome can show different symptoms than in children. Adults might have more severe or varied symptoms. This includes more frequent or severe fever, aphthous stomatitis, pharyngitis, and cervical adenitis. It can also affect daily life and work, requiring specific management strategies.
Long-term Management Strategies
Managing PFAPA Syndrome in adults over the long term requires a mix of medication, lifestyle changes, and regular check-ups. Corticosteroids can help manage symptoms during episodes. Making lifestyle adjustments, like dietary changes and stress management, is also key in reducing episode frequency and severity.
It’s vital to have regular follow-ups with healthcare providers. This ensures treatment plans can be adjusted as needed and any new issues can be addressed promptly.
Lifestyle Modifications and Home Care
Managing PFAPA Syndrome demands a holistic approach, encompassing lifestyle adjustments and home care tactics. By making specific changes in daily routines, those with PFAPA Syndrome can manage their symptoms more effectively. This, in turn, enhances their quality of life significantly.
Dietary Considerations and Possible Triggers
Diet is a critical factor in managing PFAPA Syndrome. Some foods can trigger or worsen symptoms, while others may offer relief. It’s vital to consume a diet rich in fruits, vegetables, and whole grains. Identifying and avoiding foods that trigger symptoms can help reduce episode frequency and severity.
- Eat a balanced diet rich in fruits, vegetables, and whole grains.
- Avoid foods that may trigger or worsen symptoms.
- Stay hydrated by drinking plenty of water.
Physical Activity Guidelines and Limitations
Physical activity is vital for overall health, but for those with PFAPA Syndrome, it’s essential to balance it with rest. During fever episodes, reducing physical activity is often necessary to aid in recovery.
- Engage in regular, moderate physical activity when not experiencing a fever episode.
- Avoid overexertion, specially during episodes.
- Listen to your body and rest when needed.
Stress Management Techniques
Stress can potentially trigger or worsen PFAPA Syndrome symptoms. Implementing effective stress management techniques can help mitigate this risk.
- Practice relaxation techniques such as deep breathing or meditation.
- Engage in activities that help reduce stress, such as yoga or reading.
- Maintain a regular sleep schedule to help manage stress.

By integrating these lifestyle modifications and home care strategies, individuals with PFAPA Syndrome can manage their condition more effectively. This approach significantly improves their overall well-being.
Psychological Impact and Support Systems
Living with PFAPA Syndrome is a significant challenge, and grasping its psychological effects is key to effective care. The unpredictable nature of its episodes and recurring symptoms can deeply impact a patient’s mental health and overall well-being.
Coping with Chronic Illness Uncertainty
The uncertainty tied to PFAPA Syndrome can cause anxiety and stress for both patients and their families. To cope, developing strategies like maintaining a routine, practicing stress-reduction techniques, and staying connected with support networks is essential. These actions help manage the uncertainty effectively.
Resources and Support Groups for Families
Families facing PFAPA Syndrome need access to resources and support groups. These networks offer emotional support, share experiences, and provide practical advice on managing the condition. Organizations focused on periodic fever syndromes often provide valuable resources and connections to support groups.
Complications and Prognosis
PFAPA Syndrome, while not life-threatening, can lead to several complications that impact the quality of life. These complications, though not common, require a detailed management plan to lessen their effects.
Potential Complications and Quality of Life Impact
The periodic fever episodes associated with PFAPA Syndrome can lead to various complications, including:
- Frequent school absences due to recurring episodes, potentially impacting academic performance.
- Emotional distress and anxiety related to the unpredictability of episodes.
- Potential for dehydration and other secondary complications if fever episodes are not managed properly.
These complications can significantly affect a patient’s quality of life. It’s essential to develop strategies for managing symptoms and reducing their impact.
Long-term Outlook and Natural History
The long-term outlook for individuals with PFAPA Syndrome is generally favorable. Most patients experience spontaneous resolution of symptoms within a few years.
Yet, some individuals may continue to experience episodes into adulthood. This requires ongoing management and potentially different treatment approaches.
Living Well with PFAPA Syndrome: Strategies for Success
Effective PFAPA Syndrome management is key to improving life quality for those affected. Understanding the disorder and its symptoms helps patients face the challenges of periodic fever episodes. This knowledge empowers them to navigate these hurdles more effectively.
Managing PFAPA Syndrome involves a multi-faceted approach. This includes medical treatment, lifestyle adjustments, and emotional support. Corticosteroids can manage fever episodes. In some cases, tonsillectomy and adenoidectomy may be considered.
Lifestyle modifications also play a significant role in managing PFAPA Syndrome. A healthy diet, staying hydrated, and stress-reducing techniques can mitigate symptoms. These actions contribute to overall well-being.
Combining these strategies and working with healthcare providers is essential. Individuals with PFAPA Syndrome can lead active, fulfilling lives. Support from family, friends, and support groups is vital for coping with the emotional aspects of the condition.
FAQ Aboout PFAPA Syndrome
Q: What is PFAPA Syndrome?
A: PFAPA Syndrome, or Periodic Fever, Aphthous Stomatitis, Pharyngitis, and Adenitis, is a rare autoinflammatory disorder. It is marked by recurring episodes of fever, mouth ulcers, sore throat, and swollen lymph nodes.
Q: What causes PFAPA Syndrome?
A: The exact cause of PFAPA Syndrome remains unknown. It is thought to stem from a complex interaction of genetic and environmental factors. This interaction leads to an imbalance in the immune system.
Q: How is PFAPA Syndrome diagnosed?
A: Diagnosis is based on clinical criteria. This includes the presence of periodic fevers, aphthous stomatitis, pharyngitis, and cervical adenitis. It also involves ruling out other causes of periodic fever.
Q: What are the treatment options for PFAPA Syndrome?
A: Treatment options include corticosteroids, non-steroidal anti-inflammatory drugs (NSAIDs), and colchicine. These are used to manage symptoms. In some cases, tonsillectomy and adenoidectomy may also be considered.
Q: Can PFAPA Syndrome be cured?
A: While there is no cure for PFAPA Syndrome, symptoms can be effectively managed. Many children outgrow the condition by adulthood.
Q: How does PFAPA Syndrome affect quality of life?
A: PFAPA Syndrome can significantly impact quality of life. Recurring episodes of fever and other symptoms are common. Yet, with proper management, individuals can lead active lives.
Q: Are there any support groups for PFAPA Syndrome?
A: Yes, there are support groups and resources available for families affected by PFAPA Syndrome. These provide emotional support, education, and advocacy.
Q: What is the long-term outlook for individuals with PFAPA Syndrome?
A: The long-term outlook varies. Many individuals experience a reduction in symptoms over time. Some may even enter remission.