Pneumothorax: What is Pneumothorax?
A pneumothorax is a serious condition that affects lung health, occurring when air enters the space between the lungs and chest cavity. This can potentially lead to lung collapse. It’s vital for both patients and healthcare providers to understand the diagnosis, treatment, and recovery processes. Diagnosis usually involves imaging tests to confirm air in the pleural space. Treatment varies based on the condition’s severity, from conservative management to surgery. The recovery process aims to restore lung function and prevent future occurrences.
This article aims to provide an overview of pneumothorax. It covers diagnosis, treatment options, and what to expect during recovery. Our goal is to inform and guide those affected by this condition. To grasp pneumothorax, we must explore its definition and its effects on the body. It’s known as a collapsed lung, happening when air leaks into the space between the lung and chest wall. This can cause partial or complete lung collapse, impacting breathing and overall respiratory function.
Definition and Basic Mechanism
Pneumothorax is characterized by air or gas in the pleural cavity, the space between lungs and chest wall. It occurs when there’s a breach in the lung or airway, allowing air to leak into this cavity. This air can come from outside, through a wound, or from within, due to lung disease or injury.
Impact on Respiratory Function
The air in the pleural space can cause lung collapse, reducing lung expansion and contraction. This affects respiratory function, as the lung’s ability to take in oxygen and expel carbon dioxide is compromised. The severity of this impact varies based on the pneumothorax size and individual lung health.
Prevalence and Demographics
Pneumothorax can affect anyone, but some groups are more at risk. It’s more common in tall, thin males aged 10 to 30 and those with lung diseases like COPD or cystic fibrosis. The incidence is higher, with primary spontaneous pneumothorax occurring in about 7.4 per 100,000 men and 1.2 per 100,000 women annually.
Understanding pneumothorax is key for diagnosis and treatment. Its effects on respiratory function and prevalence among different groups underscore the importance of awareness and timely medical intervention.
Types and Classification of Pneumothorax
Grasping the various pneumothorax classifications is key to accurate diagnosis and treatment. This condition, with its multiple forms, demands a tailored management approach. Each type requires a specific strategy to address its unique challenges.
Primary Spontaneous Pneumothorax
Primary spontaneous pneumothorax affects individuals without lung disease, mainly tall, thin males. The cause is often unknown but thought to stem from the rupture of small air blisters on the lung’s surface.
Secondary Spontaneous Pneumothorax
Secondary spontaneous pneumothorax is linked to lung diseases like COPD, cystic fibrosis, or pneumonia. It’s more prevalent in older adults and can be more severe due to the lung’s compromised state.
Traumatic Pneumothorax
Traumatic pneumothorax arises from chest injuries, such as those from car accidents or penetrating wounds. These injuries allow air to leak into the pleural space, causing lung collapse.
Tension Pneumothorax
Tension pneumothorax is a critical condition where air enters the pleural space but cannot escape. This leads to increasing pressure, potentially shifting the mediastinum and compromising heart and lung function. It necessitates immediate medical intervention.
Iatrogenic Pneumothorax
Iatrogenic pneumothorax is caused by medical procedures, such as lung biopsies, central line placements, or mechanical ventilation. It’s a critical consideration in diagnosing pneumothorax, mainly in hospitalized patients.
In summary, categorizing pneumothorax into its different types is vital for understanding its pathophysiology and developing effective treatment plans. Each type presents unique characteristics and implications for patient care.
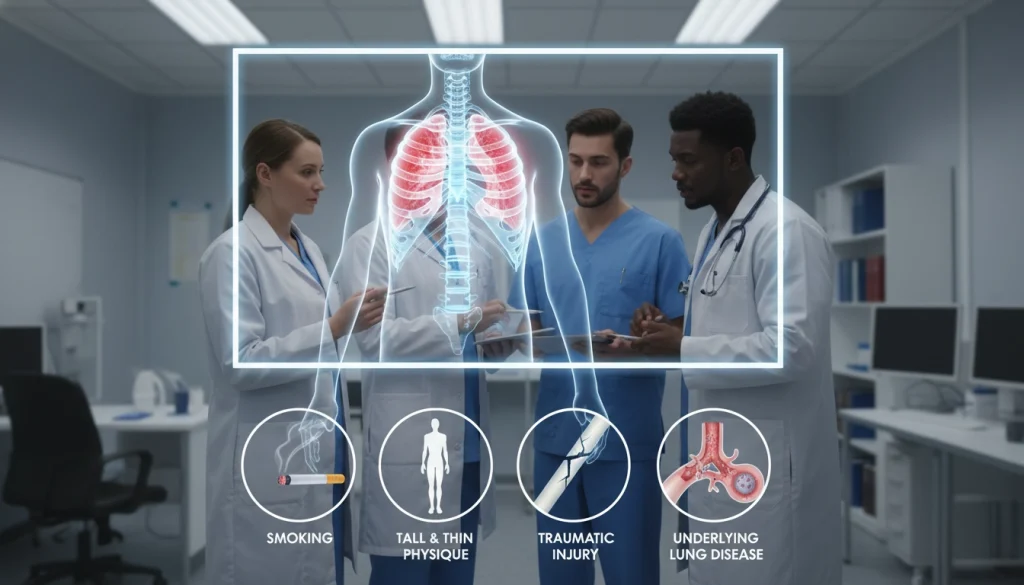
Common Causes and Risk Factors
Understanding the causes and risk factors of pneumothorax is key to prevention and management. Pneumothorax can stem from various factors. These include underlying lung conditions, lifestyle choices, genetic predispositions, and environmental influences.
Underlying Lung Conditions
Pre-existing lung conditions significantly increase the risk of developing pneumothorax. These conditions can weaken the lung tissue, making it more susceptible to rupture.
COPD and Emphysema
Chronic Obstructive Pulmonary Disease (COPD) and emphysema are major risk factors. COPD encompasses conditions that cause airflow obstruction. Emphysema involves damage to the alveoli, making it harder for the lungs to exchange oxygen and carbon dioxide.
Cystic Fibrosis
Cystic fibrosis, a genetic disorder, is another significant risk factor. It causes severe damage to the lungs, digestive system, and other organs. The thick mucus associated with cystic fibrosis can lead to lung damage and increase the likelihood of pneumothorax.
Lung Cancer
Lung cancer can also contribute to the development of pneumothorax. Tumors can weaken the lung tissue and cause air leaks.
Lifestyle Factors
Lifestyle choices play a significant role in the risk of developing pneumothorax.
Smoking
Smoking is a major risk factor. It damages lung tissue and increases the likelihood of lung disease.
Physical Activities
Certain physical activities, such as those involving changes in air pressure or strenuous exercise, can increase the risk of pneumothorax.
Genetic Predispositions
Genetic factors can predispose individuals to conditions that increase the risk of pneumothorax. For instance, genetic conditions like alpha-1 antitrypsin deficiency can lead to lung disease.
Environmental Factors
Environmental factors, such as exposure to high altitudes or changes in atmospheric pressure, can also contribute to the risk of pneumothorax.
By understanding these causes and risk factors, individuals can take steps to mitigate their risk. Healthcare providers can offer targeted prevention and treatment strategies.
Recognizing Pneumothorax Symptoms
It’s vital for patients to recognize the signs of pneumothorax to get timely medical care. The symptoms can vary, and knowing these variations is key for early diagnosis and treatment.
Common Symptoms
Sudden chest pain and shortness of breath are the most common symptoms of pneumothorax. These symptoms arise when the lung collapses. This collapse hampers the lung’s ability to expand and contract.
- Sharp, stabbing chest pain that worsens with deep breathing
- Difficulty breathing or shortness of breath
- Bluish discoloration of the skin due to lack of oxygen
- Fatigue or feeling weak
Emergency Warning Signs
In severe cases, pneumothorax can be life-threatening. Look out for these emergency warning signs:
- Severe difficulty breathing
- Rapid heart rate or palpitations
- Loss of consciousness or fainting
- Severe chest pain
Symptom Variations by Type
The symptoms of pneumothorax differ based on the type. Traumatic pneumothorax often has more immediate and severe symptoms due to injury. Spontaneous pneumothorax may develop more gradually.
Silent Pneumothorax
In some cases, pneumothorax can be asymptomatic, known as silent pneumothorax. This condition is dangerous because it may not be diagnosed until it’s severe or found by chance during imaging for another condition.
Knowing the range of pneumothorax symptoms is essential for early detection and treatment. If you or someone else shows symptoms of pneumothorax, seek immediate medical attention.
Diagnostic Procedures for Pneumothorax
Pneumothorax diagnosis combines physical assessment and imaging modalities. Accurate diagnosis is key for the right treatment plan.
Physical Examination
The first step in diagnosing pneumothorax is a physical examination. Healthcare providers check for symptoms like chest pain and shortness of breath. They also perform auscultation to detect decreased breath sounds on the affected side.
Imaging Studies
Imaging studies are vital for confirming pneumothorax diagnosis.
Chest X-rays
Chest X-rays are the first imaging choice. They show air in the pleural space and the pneumothorax size.
CT Scans
CT scans offer detailed images. They help spot underlying lung issues or complications.
Ultrasound
Ultrasound is useful in emergencies. It quickly identifies pneumothorax.
Other Diagnostic Tools
Other tools include assessing the patient’s overall clinical presentation and history.
Differential Diagnosis
Differential diagnosis rules out conditions like pleurisy or pulmonary embolism. A detailed diagnostic workup is necessary for accurate diagnosis.
Key factors in differential diagnosis include:
- Patient’s medical history
- Symptom presentation
- Imaging findings
Treatment Approaches and Interventions
Pneumothorax treatment spans from conservative methods to surgical options. The treatment choice hinges on the pneumothorax’s severity, type, and the patient’s health status.
Conservative Management
Small, uncomplicated pneumothoraces might be managed conservatively. This method involves monitoring with serial chest X-rays and clinical evaluations.
Oxygen Therapy
Oxygen therapy aids in faster pleural air absorption. Patients receive high-flow oxygen through a mask.
Needle Aspiration
Needle aspiration is a minimally invasive procedure. It involves inserting a needle into the pleural space to remove air. It’s often used for primary spontaneous pneumothorax patients.
Chest Tube Insertion
Chest tube insertion is a common pneumothorax treatment. It involves placing a tube into the pleural space to drain air.
Traditional Chest Tubes
Traditional chest tubes are effective for draining large amounts of air or fluid from the pleural space.
Small-bore Catheters
Small-bore catheters are less invasive. They are used for smaller pneumothoraces or as a follow-up to traditional chest tubes.
Surgical Options
For recurrent or complicated pneumothoraces, surgical intervention is often necessary.
Video-Assisted Thoracoscopic Surgery (VATS)
VATS is a minimally invasive technique. It treats pneumothorax by removing bullae or blebs causing the condition.
Thoracotomy
A thoracotomy is a more invasive procedure. It involves making an incision into the chest cavity to access the lungs and pleura directly.
Pleurodesis
Pleurodesis involves creating inflammation between the pleural layers. This adhesion prevents future pneumothoraces.
The choice of treatment is highly individualized. It considers the patient’s specific condition, medical history, and preferences.
Recovery Process and Timeline
The recovery from pneumothorax is a detailed process, starting with hospital care and extending to home recovery and ongoing health checks. Knowing the various stages and what to anticipate can greatly enhance the recovery journey.
Hospital Recovery
Hospital care is the initial phase post-diagnosis. It includes continuous monitoring by medical staff, oxygen therapy if needed, and sometimes a chest tube to expand the lung. The duration of hospital stay varies based on the pneumothorax’s severity and the patient’s health.
Home Recovery Guidelines
After discharge, patients must adhere to specific home recovery guidelines. This includes ample rest, avoiding heavy activities, and following prescribed medications. It’s also vital to watch for any signs of complications or worsening symptoms.
Physical Activity Restrictions
Restrictions on physical activity are a key part of recovery. Patients are usually advised to avoid heavy lifting, bending, or intense exercise for weeks. The exact timeframe depends on the individual’s health and the doctor’s advice.
Breathing Exercises
Breathing exercises are beneficial for lung function and recovery. Simple deep breathing exercises can be helpful. Yet, it’s important to consult a healthcare provider before starting any new exercise routine.
Pain Management
Effective pain management is essential during recovery. This may involve pain medication as directed by a healthcare provider. Techniques like relaxation and deep breathing can also help manage pain.
Long-term Monitoring
Long-term monitoring is critical to ensure the lung remains expanded and to detect any recurrence or complications. Regular follow-up appointments with a healthcare provider are vital for monitoring recovery and addressing any concerns.
In summary, recovering from pneumothorax requires a holistic approach, including medical treatment, rest, rehabilitation, and ongoing monitoring. By understanding the recovery process and timeline, patients can better navigate their journey towards full recovery.
- Rest and avoid strenuous activities
- Follow medication regimens as prescribed
- Monitor for signs of complications
- Attend follow-up appointments
Pneumothorax Complications
Pneumothorax complications can be categorized into short-term and long-term effects. Each category presents unique challenges for patient care and recovery.
Short-term Complications
Short-term complications of pneumothorax can arise during or immediately after the initial event. These complications can significantly impact the patient’s immediate health. They require prompt medical attention.
Respiratory Distress
Respiratory distress is a common short-term complication. It is characterized by difficulty breathing, rapid breathing rate, and decreased oxygen saturation. It may necessitate supplemental oxygen therapy and close monitoring.
Infection
Infection is another short-term complication. It can occur due to the introduction of bacteria during medical procedures or due to the pneumothorax itself. Signs of infection include fever, increased white blood cell count, and purulent discharge.
Long-term Complications
Long-term complications can persist or develop after the initial pneumothorax event. They affect the patient’s quality of life and require ongoing management.
Chronic Pain
Chronic pain is a significant long-term complication. It results from nerve damage, adhesions, or other factors related to the pneumothorax or its treatment. Management strategies may include pain medication, physical therapy, and other interventions.
Reduced Lung Function
Reduced lung function can occur due to the pneumothorax itself or as a result of treatments. Pulmonary rehabilitation and breathing exercises can help improve lung function over time.
Recurrence Rates and Factors
The recurrence of pneumothorax is a significant concern. Rates vary based on the underlying cause and treatment approach. Factors influencing recurrence include the presence of underlying lung disease, smoking status, and the effectiveness of initial treatment.
- Primary spontaneous pneumothorax has a higher recurrence rate compared to other types.
- Smoking cessation is critical in reducing the risk of recurrence.
- Certain underlying conditions, such as COPD, increase the likelihood of recurrence.
Understanding these complications and their management is essential for healthcare providers. It is vital for delivering optimal care and improving patient outcomes.
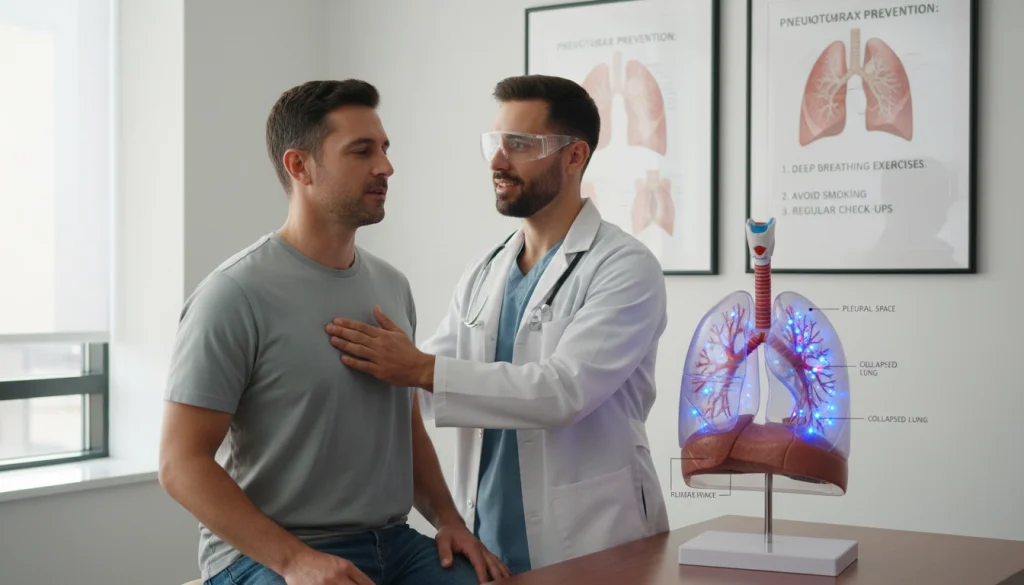
Prevention Strategies for High-Risk Individuals
Preventing pneumothorax in high-risk groups requires a multi-faceted approach. This includes lifestyle changes and medical interventions. Understanding and addressing risk factors helps individuals take proactive steps to reduce their risk.
Lifestyle Modifications
Lifestyle adjustments are key for preventing pneumothorax, mainly for those at high risk. Important changes include:
- Smoking Cessation: Quitting smoking significantly reduces pneumothorax risk. Smoking damages lung tissue, increasing the chance of lung collapse.
- Activity Adjustments: Avoiding activities with rapid air pressure changes, like scuba diving or flying in unpressurized planes, can prevent pneumothorax.
Management of Underlying Conditions
Managing lung conditions like COPD or asthma is critical in preventing pneumothorax. This involves following prescribed treatments, attending regular check-ups, and closely monitoring symptoms.
Preventive Procedures
For high-risk individuals, preventive procedures may be recommended. Pleurodesis, for example, involves introducing a substance into the pleural space. This causes inflammation and adhesion between the lung and chest wall, preventing future pneumothorax.
Regular Medical Check-ups
Regular medical check-ups are vital for high-risk individuals. These visits allow healthcare providers to monitor lung health, adjust treatments as needed, and address any concerns or symptoms promptly.
Special Considerations for Different Populations
Pneumothorax impacts various groups uniquely, requiring specialized care. Its effects differ by age, health, and lifestyle. It’s vital to grasp these differences for effective management.
Pneumothorax in Children and Adolescents
In children and teens, pneumothorax often stems from lung diseases or trauma. Symptoms can be vague, making diagnosis tricky.
- Higher incidence in tall, thin males
- Often related to underlying conditions like asthma or cystic fibrosis
- Requires careful consideration in diagnosis due to non-specific symptoms
Pneumothorax During Pregnancy
Pneumothorax in pregnancy is rare but dangerous. Pregnancy’s changes can alter how pneumothorax presents and is managed.
- Increased risk due to hormonal changes and lung volume shifts
- Requires careful monitoring and potentially adjusted treatment plans
- Consideration of the fetus’s health in management decisions
Pneumothorax in Elderly Patients
Elderly individuals face a higher risk of pneumothorax due to lung diseases and other health issues. Management must account for these factors.
- Higher risk due to chronic obstructive pulmonary disease (COPD) and other lung conditions
- Potential for more severe symptoms and complications
- Need for tailored treatment considering overall health status
Pneumothorax in Athletes
Athletes, mainly those in high-impact sports, are at risk of pneumothorax. This condition can severely limit their sports participation.
- Increased risk due to physical exertion and possible trauma
- Need for prompt diagnosis and treatment to allow return to activity
- Consideration of preventive measures for recurrent pneumothorax
Air Travel Considerations
Air travel poses risks for those with pneumothorax history due to air pressure changes.
- Avoiding air travel after recent pneumothorax episodes
- Consulting healthcare providers before flying
- Understanding airline policies for travelers with medical conditions
Healthcare providers must understand these special considerations to manage pneumothorax effectively across different populations. Tailored approaches can significantly improve outcomes for these patients.
Advances in Pneumothorax Research and Treatment
Medical technology and research have seen significant improvements, leading to better outcomes for those with pneumothorax. The field is constantly evolving. New diagnostic methods, innovative treatments, genetic research, and minimally invasive techniques are being developed.
New Diagnostic Approaches
Recent advancements in diagnostic imaging have greatly improved the detection and management of pneumothorax. Some of these new approaches include:
- High-resolution computed tomography (CT) scans for more accurate diagnosis
- Ultrasound imaging for quick and bedside assessment
- Advanced radiographic techniques for better visualization
Innovative Treatment Methods
Treatment strategies for pneumothorax have become more sophisticated, providing patients with more effective care. Some of these innovative methods include:
- Personalized treatment plans based on individual patient needs
- Use of advanced materials for chest drains and catheters
- Development of new protocols for managing recurrent pneumothorax
Genetic Research
Genetic studies are providing insights into the underlying causes of pneumothorax, focusing on spontaneous cases. This research is essential for understanding risk factors and developing preventive strategies.
Minimally Invasive Techniques
The shift towards minimally invasive procedures has significantly improved patient recovery times and reduced complications. Techniques such as video-assisted thoracoscopic surgery (VATS) are becoming increasingly common.
These advances in pneumothorax research and treatment are transforming patient care. They offer better outcomes and an improved quality of life.
When to Seek Medical Attention
Recognizing the need for urgent medical care is critical for pneumothorax patients. This condition necessitates close monitoring and prompt action.
Emergency Situations
Certain pneumothorax scenarios require immediate medical intervention. These include severe breathing difficulties, chest pain, or sudden symptom onset.
- Severe shortness of breath
- Chest pain or tightness
- Bleeding or signs of infection
Follow-up Care Guidelines
Post-treatment, follow-up care is vital to track recovery and manage complications. Patients must keep scheduled appointments and report any concerning symptoms.
Red Flags During Recovery
During recovery, specific symptoms or signs may signal complications. These include increased pain, breathing difficulties, or infection signs.
- Increased severity of symptoms
- Fever or chills
- Unexpected discharge or leakage
Communication with Healthcare Providers
Effective communication with healthcare providers is key in managing pneumothorax. Patients should be ready to discuss their symptoms, concerns, and any condition changes.

Moving Forward After Pneumothorax
Recovering from pneumothorax demands careful attention to long-term health and lifestyle adjustments. After treatment, following a healthcare provider’s guidance is key for a smooth recovery.
Patients should prioritize lung health post-pneumothorax. Avoiding smoking is critical, as it raises the risk of recurrence and respiratory issues.
Lifestyle changes may be needed to prevent future pneumothoraxes. This could mean modifying physical activities or avoiding certain environments that might trigger another episode.
Regular check-ups with healthcare providers are vital for monitoring recovery and addressing concerns. Being proactive about health can lower the risk of complications and enhance well-being post-pneumothorax.
Recovery from pneumothorax is a journey that requires patience, understanding, and cooperation with healthcare professionals. By making informed lifestyle changes and focusing on long-term health, individuals can effectively navigate their recovery.
FAQ
Q: What is pneumothorax?
A: Pneumothorax occurs when air enters the pleural cavity, causing lung collapse. This can be partial or complete.
Q: What are the main types of pneumothorax?
A: Pneumothorax types include primary spontaneous, secondary spontaneous, traumatic, tension, and iatrogenic pneumothorax.
Q: What are the symptoms of pneumothorax?
A: Symptoms include sudden chest pain, shortness of breath, and breathing difficulties. Some cases are asymptomatic, known as silent pneumothorax.
Q: How is pneumothorax diagnosed?
A: Diagnosis involves a physical exam, chest X-rays, CT scans, or ultrasound. Additional tools may confirm the extent of pneumothorax.
Q: What are the treatment options for pneumothorax?
A: Treatments range from conservative management and oxygen therapy to needle aspiration and chest tube insertion. Surgical options include VATS or thoracotomy.
Q: Can pneumothorax recur?
A: Yes, pneumothorax can recur. Recurrence risk depends on the type and individual factors. Preventive measures can reduce recurrence risk.
Q: How can high-risk individuals prevent pneumothorax?
A: High-risk individuals should quit smoking, manage lung conditions, make lifestyle changes, and get regular check-ups. These steps can lower pneumothorax risk.
Q: What are the possible complications of pneumothorax?
A: Complications include respiratory distress, infection, chronic pain, reduced lung function, and recurrence. Prompt treatment can minimize these risks.
Q: Are there any special considerations for different populations with pneumothorax?
A: Yes, children, pregnant women, elderly, and athletes require special considerations. Their unique needs and circumstances must be addressed in management.















