Polycythemia: Causes and Risk Factors
A rare blood disorder characterized by an excessive number of red blood cells, Polycythemia can lead to serious health complications if left untreated. This condition can cause a range of symptoms, including headaches, dizziness, and fatigue. These symptoms arise from the increased viscosity of the blood. The causes of this disorder can vary. Some cases are primary, resulting from genetic mutations. Others are secondary, resulting from chronic hypoxia or other factors.
Understanding the causes, symptoms, and treatment options is key to managing the condition effectively. Treatment aims to reduce the red blood cell count and alleviate symptoms.
Understanding Polycythemia
Polycythemia is a complex blood disorder that has garnered significant attention in the medical community. It is known for its multifaceted nature. To fully understand this condition, it’s essential to explore its definition and historical background.
Definition and Overview
Polycythemia is characterized by an abnormal increase in the number of red blood cells in the body. This leads to thicker blood, which can cause serious health issues. These include blood clots and cardiovascular problems. The definition encompasses various aspects, including the physiological and pathological characteristics that distinguish it from other blood disorders.
Historical Background
The concept of polycythemia has evolved significantly over the years. Initially identified in the early 20th century, it was first associated with an increased risk of thrombosis. Research has progressed, leading to a better understanding of its causes, symptoms, and treatment options. The historical context provides valuable insights into how the perception and management of polycythemia have changed.
Types of Polycythemia
Grasping the various forms of polycythemia is key to precise diagnosis and treatment. This condition encompasses several conditions, each with unique causes and traits.
Polycythemia Vera
Polycythemia Vera (PV) is a rare blood disorder marked by excessive red, white blood cells, and platelets. It’s a myeloproliferative neoplasm, often caused by a JAK2 gene mutation.
JAK2 Mutation
The JAK2 V617F mutation activates the JAK-STAT pathway, driving cell growth and survival. This mutation affects about 95% of PV patients.
Clinical Presentation
Symptoms of PV include headaches, dizziness, and thrombosis due to increased blood viscosity. Patients may also experience itching and erythromelalgia, characterized by burning pain and redness in hands and feet.
Secondary Polycythemia
Secondary Polycythemia results from external factors or medical conditions, not a myeloproliferative neoplasm. It’s a body response to certain states.
Hypoxia-Induced
Chronic hypoxia, like in COPD or high altitudes, triggers secondary polycythemia. The body compensates by increasing red blood cells.
Hormone-Induced
Hormonal disorders, such as Cushing’s syndrome or testosterone use, can also cause secondary polycythemia. Hormonal increases stimulate red blood cell production.
Relative Polycythemia
Relative Polycythemia, or apparent polycythemia, occurs when plasma volume decreases. This results in a relative increase in red blood cell concentration. It’s often seen in dehydration or diuretic use.
In summary, each type of polycythemia demands a specific diagnostic and treatment strategy. Recognizing these differences is vital for effective management.
The Pathophysiology of Polycythemia
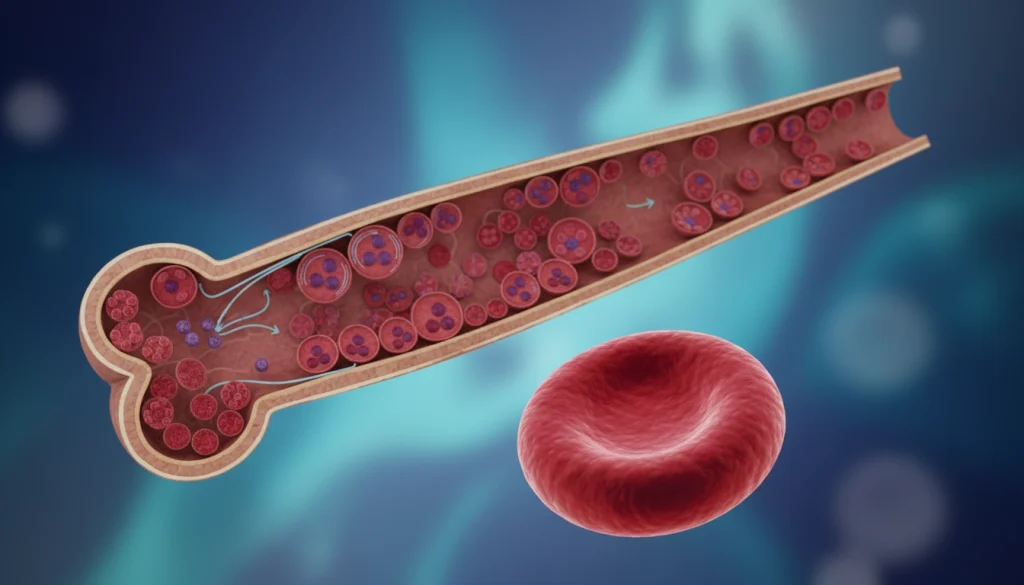
Polycythemia’s development is tied to changes in blood cell production, known as erythropoiesis.
Normal Blood Cell Production
Erythropoiesis, the production of blood cells, is a finely tuned process. It involves red, white blood cells, and platelets. Erythropoietin, a hormone from the kidneys, is key in making red blood cells. The body keeps a balance between making and destroying blood cells under normal conditions.
Dysregulated Erythropoiesis
In polycythemia, this balance is upset, causing too many red blood cells. This imbalance can stem from genetic issues, chronic low oxygen, or other health problems. The excess red blood cells make blood thicker, which can cause blood clots and other issues.
Polycythemia vera, a specific type, often has a JAK2 gene mutation. This mutation turns on pathways that make more blood cells, leading to too many red blood cells.
Molecular Mechanisms
The molecular basis of polycythemia involves complex signaling pathways. In polycythemia vera, the JAK/STAT pathway is always on because of the JAK2 V617F mutation. This constant activity makes blood cells more responsive to growth factors, causing too many red blood cells.
Causes and Risk Factors
The onset of polycythemia is shaped by a mix of genetic, environmental, and medical elements. Grasping these factors is key to diagnosing and managing the condition.
Genetic Predisposition
Genetic predisposition significantly influences polycythemia development. Specific genetic mutations can heighten the risk of this condition.
Hereditary Mutations
Hereditary mutations, like those in the JAK2 gene, can lead to polycythemia vera. These mutations are passed down from family members, raising the risk for relatives.
Familial Patterns
Studies show familial patterns in polycythemia, hinting at a genetic link. Those with a family history may face a higher risk.
Environmental Triggers
Environmental factors also play a role in polycythemia development. Exposure to specific conditions or substances can trigger the condition.
For example, high-altitude living can cause secondary polycythemia due to lower oxygen levels. Smoking and exposure to certain chemicals also increase the risk.
Associated Medical Conditions
Certain medical conditions can raise the risk of polycythemia. These include conditions that impair oxygen delivery to tissues, like COPD and sleep apnea.
Other associated conditions include kidney disease and certain tumors that can cause secondary polycythemia.
Signs and Symptoms of Polycythemia
Polycythemia, a condition with too many red blood cells, shows various signs and symptoms. These can greatly affect a person’s life quality. It’s vital to recognize these symptoms early for timely diagnosis and effective treatment.
Common Clinical Manifestations
Polycythemia’s symptoms can vary, impacting different body systems. Common issues include headaches, dizziness, and fatigue. These occur due to blood’s increased viscosity from the high red blood cell count. Some people may also feel itching, often after warm baths or showers, and a burning sensation in their hands and feet.
Other symptoms include a ruddy complexion, spleen enlargement, and high blood pressure. The thickened blood can reduce blood flow to organs, potentially causing thrombosis.
Early Warning Signs
Early signs of polycythemia can be subtle. They may include blurred vision, weakness, and shortness of breath. These symptoms arise from decreased oxygen delivery to tissues and organs due to abnormal blood rheology.
Spotting these early signs is key for timely medical evaluation. Anyone experiencing these symptoms should see a healthcare provider. This is even more important if there’s a family history of polycythemia or other myeloproliferative disorders.
When to Seek Medical Attention
Seeking medical help is critical if symptoms persist or get worse. Severe headaches, chest pain, or trouble breathing require immediate care. Early diagnosis and treatment can greatly improve outcomes for those with polycythemia.
Regular check-ups with a healthcare provider are essential for managing the condition. Understanding polycythemia’s signs and symptoms empowers individuals to actively participate in their care. This helps in maintaining their overall health.
Diagnostic Approaches for Polycythemia
Healthcare professionals use various diagnostic methods to identify polycythemia. These approaches are essential for diagnosing the condition, determining its type, and guiding treatment. They help in creating a tailored treatment plan for each patient.
Complete Blood Count Analysis
A complete blood count (CBC) is a key test for diagnosing polycythemia. It measures the levels of different blood cells. In polycythemia, the CBC shows an elevated count of red blood cells, hematocrit, and hemoglobin.
This analysis is critical. It provides initial evidence of polycythemia and helps differentiate it from other conditions. It’s important for identifying the condition accurately.
Erythropoietin Level Testing
Erythropoietin (EPO) is a hormone that stimulates red blood cell production. Testing EPO levels helps distinguish between primary and secondary polycythemia. Low EPO levels are often seen in polycythemia vera, while high levels may indicate secondary polycythemia.

Bone Marrow Examination
A bone marrow biopsy and aspiration are performed to examine the bone marrow’s cellularity and morphology. In polycythemia vera, the bone marrow is hypercellular with an increased number of red and white blood cells, and platelets. This examination helps diagnose polycythemia vera and rule out other myeloproliferative neoplasms.
Genetic and Molecular Testing
Genetic testing for mutations such as JAK2 V617F is critical in diagnosing polycythemia vera. Most patients with polycythemia vera have this mutation. Additional genetic tests may be conducted to identify other relevant mutations.
These diagnostic approaches, when used together, provide a detailed understanding of polycythemia. They help in developing an appropriate treatment plan for each patient.
Treatment Options for Polycythemia
Managing Polycythemia requires a variety of treatment strategies to lower complication risks and enhance patient outcomes. Each treatment plan is customized, considering the unique aspects of the patient’s condition.
Therapeutic Phlebotomy
Therapeutic phlebotomy is a primary treatment for Polycythemia, involving blood removal to decrease red blood cell count. This method reduces the risk of blood clots and alleviates symptoms caused by thickened blood.
The frequency of phlebotomy sessions varies based on the patient’s condition and treatment response. Continuous monitoring is critical to adjust the treatment plan as necessary.
Myelosuppressive Medications
Myelosuppressive medications aim to lower blood cell production in the bone marrow. These drugs help manage Polycythemia symptoms and decrease the need for frequent blood removal.
Hydroxyurea
Hydroxyurea is a myelosuppressive medication that inhibits DNA synthesis, reducing blood cell production. It’s commonly prescribed for patients needing frequent blood removal or at high risk of blood clots.
Interferon Alpha
Interferon alpha is another myelosuppressive agent for Polycythemia treatment. It modulates the immune system and decreases hematopoietic cell proliferation.
JAK Inhibitors
JAK inhibitors target the JAK/STAT signaling pathway involved in Polycythemia. These drugs reduce red blood cell production and alleviate symptoms.
Aspirin Therapy
Aspirin therapy is often combined with other treatments to prevent blood clots in Polycythemia patients. Low-dose aspirin helps prevent heart-related complications.
Using aspirin must be carefully weighed, as it can increase bleeding risks. Regular monitoring is essential to manage the benefits and risks.
Managing Polycythemia Long-Term
Managing polycythemia long-term requires a multi-faceted approach. This includes lifestyle changes and regular medical check-ups. Such a strategy helps in reducing symptoms and complications.
Lifestyle Modifications
Lifestyle adjustments are key in managing polycythemia. These changes can greatly improve the quality of life for those affected.
Hydration Importance
Hydration is critical for polycythemia patients. It helps maintain blood viscosity and lowers the risk of blood clots.
Physical Activity Guidelines
Regular physical activity is advised, but it must be tailored to the individual’s health. Gentle exercises like walking or yoga are beneficial.
Dietary Considerations
A balanced diet is recommended, rich in fruits, vegetables, and whole grains. It’s also important to limit sodium and avoid excessive alcohol.
Regular Monitoring and Follow-up
Regular monitoring and follow-up care are vital for managing polycythemia. This includes regular blood tests to check hematocrit levels and adjusting treatment plans as needed.
Follow-up appointments with healthcare providers are essential. They help in early detection of complications and timely interventions.
Potential Complications of Polycythemia
Understanding the complications of Polycythemia is key to effective management and better patient outcomes. If not managed well, Polycythemia can lead to serious health issues.
Thrombotic Events
Thrombotic events are a major complication of Polycythemia. These events can have a significant impact on patient outcomes.
Arterial Thrombosis
Arterial thrombosis occurs when a blood clot forms in an artery. This can lead to serious cardiovascular events like heart attacks and strokes.
Venous Thromboembolism
Venous thromboembolism, including deep vein thrombosis and pulmonary embolism, is a significant risk for patients with Polycythemia. It requires careful management.
Bleeding Complications
Bleeding complications can occur in patients with Polycythemia. This is often due to acquired von Willebrand syndrome or other coagulopathies associated with the condition.
- Common bleeding sites include the gastrointestinal tract and skin.
- Management strategies often involve addressing the underlying cause.
- Close monitoring is essential to prevent severe bleeding episodes.
Progression to Myelofibrosis or Leukemia
Patients with Polycythemia Vera are at risk of progressing to myelofibrosis or acute myeloid leukemia. Both are serious conditions requiring distinct management approaches.
Regular follow-up and monitoring are critical to detect any signs of progression early.
Prognosis and Outcomes
The prognosis for individuals with Polycythemia varies based on several key factors. Understanding these factors is essential for managing the condition and improving patient outcomes.
Survival Rates
Survival rates for Polycythemia patients have seen a significant improvement with advancements in treatment options. Studies indicate that with proper management, many patients can lead active lives for many years.
The overall survival rate is influenced by the type of Polycythemia, with Polycythemia Vera having a relatively better prognosis compared to secondary forms.
- Median survival for Polycythemia Vera patients is approximately 10-20 years.
- Early diagnosis and treatment can significantly improve survival rates.
- Regular monitoring is critical for managing the condition effectively.
Quality of Life Considerations
Quality of life for Polycythemia patients can be impacted by symptoms and treatment side effects. Effective management strategies are key to maintaining a good quality of life.
Lifestyle adjustments, such as staying hydrated and avoiding extreme temperatures, can help manage symptoms.
Factors Affecting Prognosis
Several factors can influence the prognosis for Polycythemia patients, including age, overall health, and response to treatment.
- Age at diagnosis: Older patients may have a poorer prognosis.
- Presence of other health conditions: Comorbidities can complicate treatment.
- Genetic mutations: Certain mutations can impact disease progression.
Understanding these factors helps healthcare providers tailor treatment plans to individual patient needs.
Living with Polycythemia
Managing polycythemia effectively requires more than just medical treatments. It also involves adopting coping strategies and utilizing support resources. This condition demands a holistic approach, addressing both physical and emotional challenges.
Coping Strategies
Coping with polycythemia means managing symptoms and the emotional toll it can take. Effective strategies can greatly enhance one’s quality of life.
Emotional Challenges
Those with polycythemia often face anxiety, depression, or stress. Seeking help from mental health professionals can be very beneficial.
Practical Daily Management
Practical management includes sticking to treatment plans and making lifestyle adjustments. It also involves monitoring symptoms closely.
Support Resources
Access to support resources is vital for those living with polycythemia. These resources offer valuable information, emotional support, and guidance on managing the condition.
Patient Organizations
Patient organizations provide a community and resources for those with polycythemia. They offer updates on research, treatment options, and coping strategies.
Educational Materials
Educational materials, such as brochures, websites, and workshops, help individuals understand their condition. They empower people to make informed decisions about their care.
Recent Advances in Polycythemia Research
The field of Polycythemia research is rapidly advancing, with groundbreaking discoveries that could lead to new treatments. These findings are essential for a deeper understanding of the condition and for developing more effective management strategies. As research continues, it is expected to result in better patient outcomes.
Novel Therapeutic Approaches
Recent studies have delved into novel therapeutic approaches for Polycythemia, focusing on targeted therapies. The use of JAK inhibitors has shown promise in reducing thrombotic risks and improving survival rates. Research into telomerase’s role in Polycythemia has also uncovered new treatment avenues.
Personalized medicine is set to significantly influence Polycythemia management in the future. Tailoring treatments to a patient’s genetic and molecular profile can offer more precise and effective care.
Ongoing Clinical Trials
Several ongoing clinical trials are exploring new treatments for Polycythemia, including interferon and targeted therapies. These trials aim to assess the safety and efficacy of these treatments. 
The results of these trials are highly anticipated, as they could significantly impact Polycythemia management. By advancing our understanding and developing more effective treatments, these trials aim to enhance the quality of life for those with Polycythemia.
The Future of Polycythemia Care
Research into Polycythemia is making strides, promising a brighter future for its care. New trends and breakthroughs are on the horizon, set to transform how we manage this condition. This brings hope to those affected by it.
Studies are now exploring novel therapies, including targeted treatments and gene editing. These innovations aim to enhance treatment results and improve the quality of life for Polycythemia patients.
Our understanding of Polycythemia is expanding, thanks to ongoing clinical trials. These trials are examining new medications and strategies. As we learn more about the condition’s molecular basis, we’re getting closer to more effective, personalized care.
The future of Polycythemia care will likely involve a more unified, multidisciplinary approach. Healthcare teams will collaborate to provide holistic, patient-focused care. The ongoing progress in research and treatment options is essential for bettering the lives of those with Polycythemia.
FAQ
Q: What is Polycythemia?
A: Polycythemia is a rare blood disorder. It’s marked by an excessive number of red blood cells.
Q: What are the main types of Polycythemia?
A: The main types include Polycythemia Vera, Secondary Polycythemia, and Relative Polycythemia.
Q: What is the JAK2 mutation, and how is it related to Polycythemia?
A: The JAK2 mutation is a genetic mutation linked to Polycythemia Vera. It’s a type of Polycythemia.
Q: What are the common symptoms of Polycythemia?
A: Symptoms include headache, dizziness, and fatigue. These are common in Polycythemia.
Q: How is Polycythemia diagnosed?
A: Diagnosis involves a complete blood count, erythropoietin level testing, and bone marrow examination. Genetic and molecular testing are also used.
Q: What are the treatment options for Polycythemia?
A: Treatments include therapeutic phlebotomy, myelosuppressive medications, and JAK inhibitors. Aspirin therapy is also used.
Q: How can Polycythemia be managed long-term?
A: Long-term management includes lifestyle changes, regular monitoring, and follow-up care.
Q: What are the possible complications of Polycythemia?
A: Complications include thrombotic events and bleeding complications. It can also lead to myelofibrosis or leukemia.
Q: What is the prognosis for individuals with Polycythemia?
A: Prognosis varies. It depends on the type of Polycythemia, treatment response, and overall health.















