Pulmonary Hemorrhage: What is Pulmonary Hemorrhage?
A life-threatening condition characterized by bleeding in the lungs, Pulmonary Hemorrhage is a critical respiratory emergency that requires immediate medical attention. This condition can result from various causes, including trauma, infection, or autoimmune disorders. Its severity can range from mild to life-threatening. Understanding the causes, symptoms, and treatment options for Pulmonary Hemorrhage is vital. It’s essential for healthcare professionals and individuals at risk. Timely intervention can significantly impact outcomes.
What is Pulmonary Hemorrhage
Pulmonary hemorrhage is a critical condition that involves bleeding in the lungs. It can be life-threatening if not treated correctly. To grasp this, we must explore its definition, epidemiology, and clinical importance.
Definition and Overview
Pulmonary hemorrhage is bleeding within the lung tissue. It can appear as diffuse alveolar hemorrhage, affecting many alveoli, or as localized hemorrhage. The severity and how it’s presented can vary greatly, depending on the cause and extent of the bleeding.
Epidemiology and Prevalence
The occurrence of pulmonary hemorrhage varies based on its causes. Conditions like autoimmune disorders or infections can raise the risk. Due to its diverse causes and sudden onset, the prevalence is not well-documented.
Clinical Significance
Pulmonary hemorrhage poses a significant risk of severe respiratory distress, low oxygen levels, and even death if not treated quickly. Prompt diagnosis and management are key to better outcomes. Healthcare providers must understand the causes, risk factors, and symptoms to effectively manage this condition.
Pathophysiology of Pulmonary Hemorrhage
The pathophysiology of pulmonary hemorrhage involves a complex interplay of hemodynamic, inflammatory, and structural factors. Grasping these mechanisms is key to diagnosing and managing the condition effectively.
Alveolar-Capillary Membrane Disruption
The alveolar-capillary membrane is vital for gas exchange in the lungs. Its disruption can cause bleeding into the alveoli, a defining feature of pulmonary hemorrhage. Various factors, including autoimmune disorders, infections, and toxic exposures, can lead to this disruption.
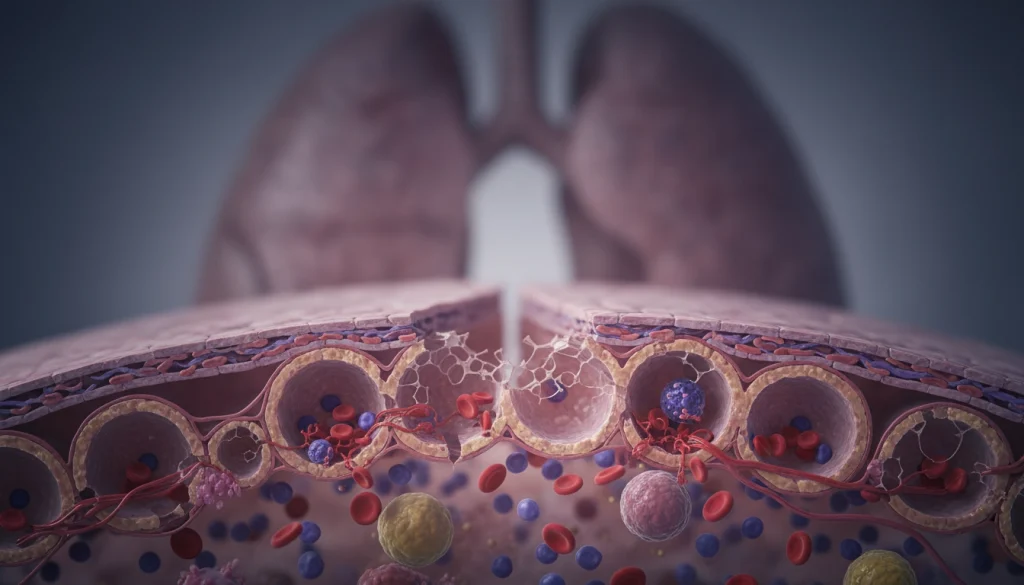
Hemodynamic Factors
Hemodynamic factors, such as elevated pulmonary vascular pressures, play a role in pulmonary hemorrhage. Conditions like heart failure and pulmonary hypertension can increase these pressures. This can lead to vessel rupture and bleeding.
Inflammatory Processes
Inflammatory processes are significant in the pathophysiology of pulmonary hemorrhage. Inflammation can damage the alveolar-capillary membrane, leading to bleeding. Conditions like vasculitis and pneumonia can trigger these inflammatory responses.
The interplay of these factors showcases the complexity of pulmonary hemorrhage. Understanding the underlying pathophysiology is essential for developing effective treatment strategies.
Classification of Pulmonary Hemorrhage
Understanding the different classifications of Pulmonary Hemorrhage is key for effective management. It can be broadly categorized into three main types. These classifications are based on clinical presentation and severity.
Diffuse Alveolar Hemorrhage
Diffuse Alveolar Hemorrhage involves widespread bleeding into the alveoli. It’s often linked to autoimmune disorders or vasculitis. Symptoms include hemoptysis, anemia, and diffuse infiltrates on chest imaging.
Localized Pulmonary Hemorrhage
Localized Pulmonary Hemorrhage is bleeding confined to a specific lung area. It’s usually caused by infections, tumors, or vascular abnormalities. The symptoms vary based on the cause and extent of bleeding.
Massive Hemoptysis
Massive Hemoptysis is a severe condition where a large volume of blood is coughed up. It’s typically over 200 mL in 24 hours. Immediate medical attention is needed to secure the airway and control the bleeding.
Common Causes of Pulmonary Hemorrhage
Understanding the causes of pulmonary hemorrhage is key to effective management. This condition can stem from various factors. Identifying the underlying cause is essential for proper treatment.
Autoimmune Disorders
Autoimmune disorders are a major cause of pulmonary hemorrhage. Conditions like Goodpasture syndrome, systemic lupus erythematosus, and vasculitis can cause lung bleeding. These disorders occur when the immune system attacks the body’s own tissues, potentially damaging the alveolar-capillary membrane.
Infectious Causes
Infections can also lead to pulmonary hemorrhage. Severe pneumonia, tuberculosis, and fungal infections can cause inflammation and damage to lung tissue, resulting in bleeding. The severity and type of infection can influence the likelihood of hemorrhage.
Traumatic Injuries
Traumatic injuries to the chest can cause pulmonary hemorrhage. The force of the injury can damage the blood vessels in the lungs, leading to bleeding. This type of hemorrhage is often associated with significant trauma, such as that sustained in a car accident or a fall from a height.
Cardiovascular Conditions
Cardiovascular conditions, including heart failure and pulmonary embolism, can also contribute to pulmonary hemorrhage. Elevated pressures in the pulmonary vessels or obstruction of blood flow can lead to rupture of the vessels and subsequent bleeding.
In conclusion, pulmonary hemorrhage is a complex condition with multiple causes. Understanding these causes is vital for diagnosing and treating the condition effectively.
Risk Factors for Developing Pulmonary Hemorrhage
Understanding the risk factors for pulmonary hemorrhage is key to early detection and management. Several factors can increase the likelihood of developing this condition.
Genetic Predispositions
Genetic predispositions significantly influence the risk of pulmonary hemorrhage. Certain genetic disorders, like hereditary hemorrhagic telangiectasia and Goodpasture’s syndrome, raise the risk. This is due to vascular abnormalities or autoimmune responses.
Environmental Exposures
Inhalation of toxic substances or pollutants can damage lung tissue, increasing the risk of pulmonary hemorrhage. Smoking is a major risk factor. It damages the lungs and impairs vascular integrity.
Pre-existing Medical Conditions
Pre-existing medical conditions, such as cardiovascular disease, chronic kidney disease, and autoimmune disorders, also raise the risk. These conditions can compromise lung function and vascular health. This makes pulmonary hemorrhage more likely.
Managing these risk factors is vital for preventing pulmonary hemorrhage and improving patient outcomes.
Clinical Presentation and Symptoms
Understanding Pulmonary Hemorrhage symptoms is key for early diagnosis and treatment. The presentation can vary, but it often includes a mix of respiratory and systemic signs.
Respiratory Manifestations
Respiratory symptoms are a key indicator of Pulmonary Hemorrhage. Patients may experience hemoptysis, ranging from mild to severe. Other symptoms include dyspnea, cough, and chest tightness. In severe cases, respiratory failure may occur, necessitating mechanical ventilation.
Systemic Symptoms
Patients with Pulmonary Hemorrhage may also show systemic symptoms. These include fever, fatigue, and weight loss. These signs can point to an underlying inflammatory or autoimmune condition.
Severity Assessment
Assessing the severity of Pulmonary Hemorrhage is vital for determining the right care level. Severity is determined by hemoptysis volume, respiratory failure, and hemodynamic instability.Patients with severe cases need immediate care to stabilize their airway and manage bleeding. The clinical presentation and symptoms of Pulmonary Hemorrhage require a detailed evaluation. This is essential for effective management strategies.
Differential Diagnosis of Pulmonary Hemorrhage
The process of diagnosing pulmonary hemorrhage is complex. It requires distinguishing it from numerous other pulmonary conditions. Symptoms like cough, dyspnea, and hemoptysis are common to many respiratory diseases. This makes the diagnosis challenging.
Distinguishing from Other Pulmonary Conditions
To differentiate pulmonary hemorrhage from other conditions, a detailed clinical history and physical examination are essential. Conditions such as pulmonary embolism, pneumonia, and malignancies can present with similar symptoms. This necessitates a thorough evaluation to narrow down the differential diagnoses.
Mimicking Disorders
Several disorders can mimic pulmonary hemorrhage. These include vasculitides, Goodpasture syndrome, and idiopathic pulmonary hemosiderosis. Each of these conditions requires specific diagnostic tests to confirm their presence accurately.
Diagnostic Challenges
Diagnosing pulmonary hemorrhage is difficult due to its nonspecific symptoms. Advanced imaging techniques and laboratory tests are often necessary to confirm the diagnosis. This complexity highlights the challenges in accurately diagnosing pulmonary hemorrhage.
Diagnostic Approaches for Pulmonary Hemorrhage
Diagnosing pulmonary hemorrhage involves a detailed strategy. It includes laboratory tests, imaging studies, and histopathological examination. This approach is essential for precise diagnosis and effective treatment.
Laboratory Testing
Laboratory tests are key in diagnosing pulmonary hemorrhage. They help evaluate the patient’s condition and identify underlying causes.
Blood Tests
Blood tests are vital for patients suspected of pulmonary hemorrhage. Important tests include:
- Complete Blood Count (CBC) to check for anemia or infection signs
- Coagulation studies to detect bleeding disorders
- Blood urea nitrogen (BUN) and creatinine to assess kidney function
Bronchoscopy and Lavage Analysis
Bronchoscopy with bronchoalveolar lavage (BAL) is a critical tool. It allows direct airway visualization and fluid collection for analysis. Blood in BAL fluid indicates pulmonary hemorrhage.
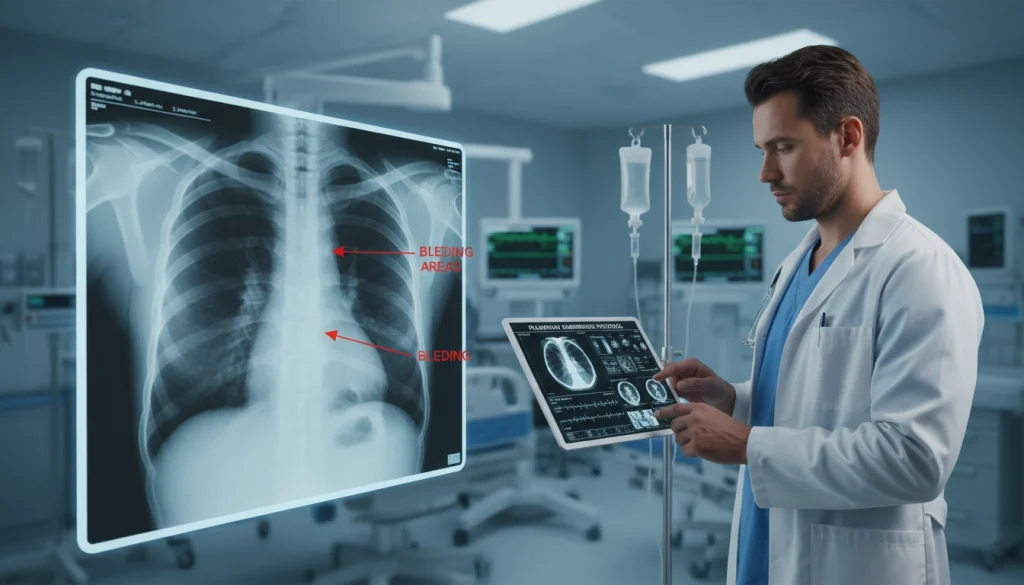
Imaging Studies
Imaging studies are vital for diagnosing and managing pulmonary hemorrhage. They provide essential information on the hemorrhage’s location and extent.
Chest X-ray Findings
Chest X-rays are often the first imaging study. They may show signs like alveolar infiltrates or consolidation, suggesting pulmonary hemorrhage.
CT Scan Evaluation
Computed Tomography (CT) scans offer more detailed information than chest X-rays. They help identify the hemorrhage’s presence, location, and extent, as well as underlying causes.
Histopathological Examination
In some cases, lung tissue examination is necessary for confirmation. This involves analyzing tissue samples from biopsy or other methods to identify pulmonary hemorrhage features.
The combination of laboratory tests, imaging studies, and histopathological examination provides a thorough diagnostic approach. It enables clinicians to accurately diagnose and develop effective treatment plans for pulmonary hemorrhage.
Emergency Management of Acute Pulmonary Hemorrhage
Dealing with acute Pulmonary Hemorrhage in an emergency situation requires quick and accurate actions. These steps are essential to stabilize the patient and stop the bleeding.
Airway Stabilization
The initial step in managing acute Pulmonary Hemorrhage is to secure the airway. This process involves:
- Checking the airway for blockages
- Supplying extra oxygen
- Considering endotracheal intubation if required
Effective airway management is key to avoid asphyxiation and ensure proper oxygenation.
Hemodynamic Support
Supporting the hemodynamics is critical in managing Pulmonary Hemorrhage. It helps maintain blood pressure and vital organ perfusion. Strategies include:
- Administering fluids and blood products as needed
- Using vasoactive medications to support blood pressure
- Monitoring hemodynamic parameters closely
Localization and Control of Bleeding
Identifying and controlling the bleeding site is essential. Techniques for managing the bleeding include:
- Bronchoscopic examination to locate the bleeding source
- Application of topical hemostatic agents
- Considering interventional radiology procedures or surgery
Effective emergency management of Pulmonary Hemorrhage demands a team effort. It requires input from pulmonology, critical care, and other relevant fields.
Treatment Strategies for Pulmonary Hemorrhage
Treating pulmonary hemorrhage involves a combination of pharmacological and interventional methods. The treatment choice depends on the cause, severity, and the patient’s health status.
Pharmacological Interventions
Pharmacological interventions are key in managing pulmonary hemorrhage. They aim to stabilize the patient, control bleeding, and address underlying causes.
Immunosuppressive Therapy
For autoimmune-related pulmonary hemorrhage, immunosuppressive therapy is used. It reduces inflammation and prevents further bleeding. Corticosteroids and cyclophosphamide are common medications used.
Antifibrinolytics
Antifibrinolytic agents, like tranexamic acid, help stabilize clots and prevent bleeding. They are effective in severe cases of hemorrhage.
Interventional Procedures
When drugs alone are not enough, or the condition is severe, interventional procedures are considered.
Bronchial Artery Embolization
Bronchial artery embolization is a minimally invasive procedure. It blocks the bleeding vessel to stop further hemorrhage.

In severe cases, surgery may be necessary. Surgical options include removing the affected area or repairing damaged blood vessels. Managing pulmonary hemorrhage requires a personalized approach. A team of specialists is essential for complex cases.
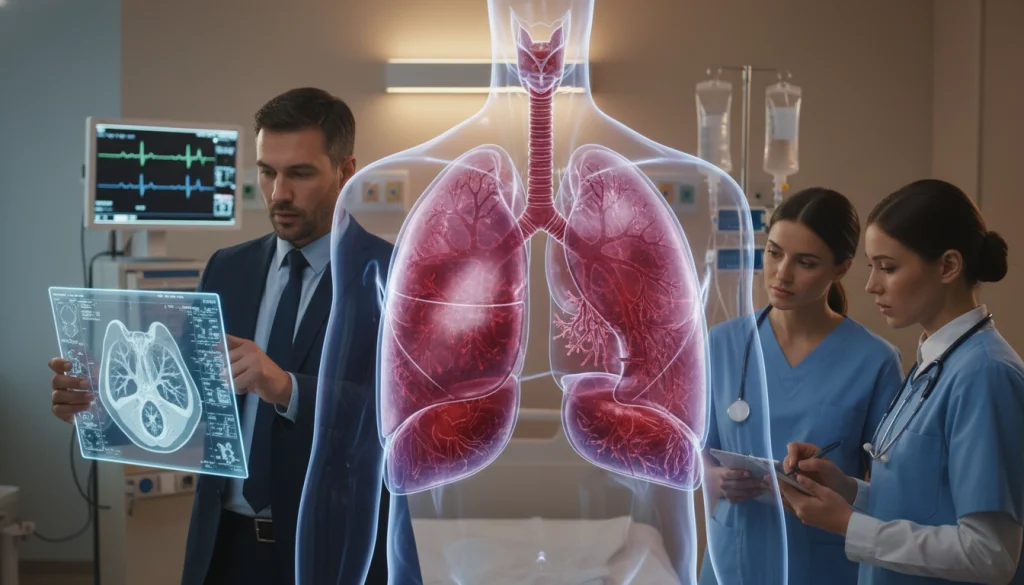
Multidisciplinary Approach to Managing Pulmonary Hemorrhage
Managing Pulmonary Hemorrhage effectively requires a team effort. It demands a detailed plan that involves several healthcare experts. This ensures a holistic approach to treatment.
Role of Pulmonologists
Pulmonologists are key in diagnosing and treating Pulmonary Hemorrhage. They perform tests like bronchoscopy and create personalized treatment plans. This is based on the patient’s specific condition.
Critical Care Management
Critical care specialists are vital for severe Pulmonary Hemorrhage cases. They manage patients in the ICU, focusing on hemodynamic support and airway stability. Their expertise is critical.
Collaboration with Specialists
Working with specialists like radiologists, cardiologists, and rheumatologists is essential. This team tackles the root causes of Pulmonary Hemorrhage and manages related conditions. Their collaboration is vital for effective care.
Rehabilitation Considerations
Rehabilitation is a key part of the treatment plan. It’s vital for those with severe lung damage or long hospital stays. Pulmonary rehabilitation programs enhance lung function and improve quality of life.
In summary, a multidisciplinary approach is critical for managing Pulmonary Hemorrhage. By involving pulmonologists, critical care specialists, and other experts, patients receive thorough care. This addresses their complex needs comprehensively.
Complications and Long-term Sequelae
Understanding the complications of pulmonary hemorrhage is vital for effective management. Pulmonary hemorrhage can lead to serious and potentially life-threatening complications.
Acute Respiratory Failure
One of the most immediate and severe complications is acute respiratory failure. This occurs when the lungs fail to meet the body’s oxygen and gas exchange needs. Often, it requires mechanical ventilation.
Hemodynamic Instability
Hemodynamic instability is another significant complication. It arises from blood loss into the lungs. This can cause decreased blood pressure, reduced cardiac output, and inadequate perfusion of vital organs.
Chronic Pulmonary Dysfunction
Survivors may experience chronic pulmonary dysfunction. This is characterized by persistent respiratory symptoms, reduced lung function, and decreased quality of life.
Psychological Impact
The psychological impact of pulmonary hemorrhage should not be underestimated. Patients may develop anxiety, depression, or post-traumatic stress disorder (PTSD) following the acute event.
In conclusion, the complications and long-term sequelae of pulmonary hemorrhage are multifaceted. They can have a profound impact on patient outcomes. Early recognition and management of these complications are essential to improve survival and quality of life.
Special Populations and Pulmonary Hemorrhage
Pulmonary hemorrhage poses unique challenges in special populations. It requires a tailored approach to diagnosis and management.
Pediatric Considerations
In pediatric patients, pulmonary hemorrhage is often linked to conditions like congenital heart disease or infections. Symptoms can be subtle, such as irritability or failure to thrive.
Early recognition and intervention are critical. They are key to improving outcomes in this vulnerable group.
Geriatric Patients
Geriatric patients with pulmonary hemorrhage often face multiple comorbidities. These include cardiovascular disease or chronic obstructive pulmonary disease (COPD). These conditions complicate management.
A treatment plan that addresses the patient’s overall health status is necessary. This is due to the presence of these comorbidities.
Pregnancy-Associated Cases
Pulmonary hemorrhage during pregnancy is rare but potentially life-threatening. It is often linked to disorders like Goodpasture syndrome or vasculitis.
Prompt diagnosis and management are essential. They are vital to prevent adverse outcomes for both mother and fetus.
Recent Advances in Pulmonary Hemorrhage Research
The field of Pulmonary Hemorrhage management is undergoing a transformation. This change is driven by groundbreaking research in diagnostics, treatments, and genetics. Studies are now delving deeper into the causes of Pulmonary Hemorrhage. This effort aims to create more precise diagnostic and therapeutic methods.
Novel Diagnostic Techniques
Recent breakthroughs in imaging and lab tests have significantly improved Pulmonary Hemorrhage diagnosis. Some of these new diagnostic tools include:
- High-resolution computed tomography (HRCT) scans, which offer detailed lung images to pinpoint hemorrhage locations and extent.
- Bronchoscopy with bronchoalveolar lavage (BAL), enabling direct airway inspection and sample collection for analysis.
- Molecular diagnostic tests, like PCR and NGS, which help identify infections or genetic factors contributing to the condition.
Emerging Treatment Modalities
Efforts to treat Pulmonary Hemorrhage are shifting towards more targeted and effective approaches. New treatment options include:
- Immunomodulatory therapies, such as rituximab and cyclophosphamide, for autoimmune-related Pulmonary Hemorrhage.
- Endovascular interventions, including embolization and stent placement, to manage bleeding and stabilize patients.
- Gene therapy and molecular-targeted treatments, being explored for their ability to address Pulmonary Hemorrhage’s root causes.
Genetic and Molecular Insights
Research into Pulmonary Hemorrhage’s genetic and molecular underpinnings has shed light on its pathogenesis. Key discoveries include:
- The identification of specific genetic mutations linked to a higher Pulmonary Hemorrhage risk.
- The role of inflammatory pathways and immune dysregulation in Pulmonary Hemorrhage development.
- The possibility of personalized medicine, tailored to each patient’s genetic and molecular profile.
Conclusion
Pulmonary Hemorrhage is a severe condition where bleeding occurs within the lungs. It’s vital to grasp its pathophysiology, types, and risk factors for proper management. The symptoms of Pulmonary Hemorrhage can be quite varied, making it hard to diagnose. Tests like lab work, imaging, and tissue analysis are key in pinpointing the cause. Emergency care focuses on securing the airway, stabilizing blood flow, and stopping the bleeding. Treatment options include medications and procedures. A team effort from pulmonologists, critical care specialists, and others is necessary for the best results.
Recent studies have introduced new diagnostic tools and treatments for Pulmonary Hemorrhage. This knowledge helps healthcare professionals deliver better care and enhance patient outcomes.
FAQ
Q: What is Pulmonary Hemorrhage?
A: Pulmonary Hemorrhage is a severe condition where blood bleeds into the lungs. This can cause respiratory failure and other serious issues.
Q: What are the common causes of Pulmonary Hemorrhage?
A: It can be caused by autoimmune disorders, infectious diseases, traumatic injuries, and cardiovascular conditions, among others.
Q: How is Pulmonary Hemorrhage diagnosed?
A: Diagnosis involves lab tests, imaging like chest X-rays and CT scans, and histopathological examination.
Q: What are the symptoms of Pulmonary Hemorrhage?
A: Symptoms include coughing up blood, fever, fatigue, and varying severity levels.
Q: How is acute Pulmonary Hemorrhage managed in an emergency?
A: Emergency management includes stabilizing the airway, supporting blood circulation, and controlling the bleeding.
Q: What are the treatment strategies for Pulmonary Hemorrhage?
A: Treatment includes immunosuppressive therapy, antifibrinolytics, and procedures like bronchial artery embolization.















