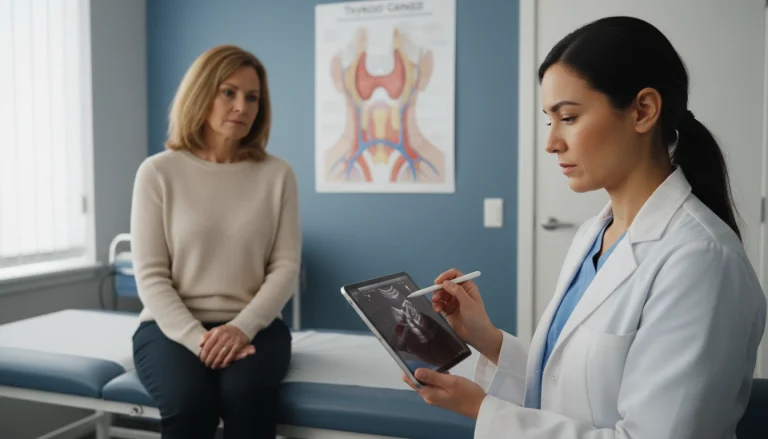
Renal Artery Stenosis: Anatomy of the Renal Arterial System
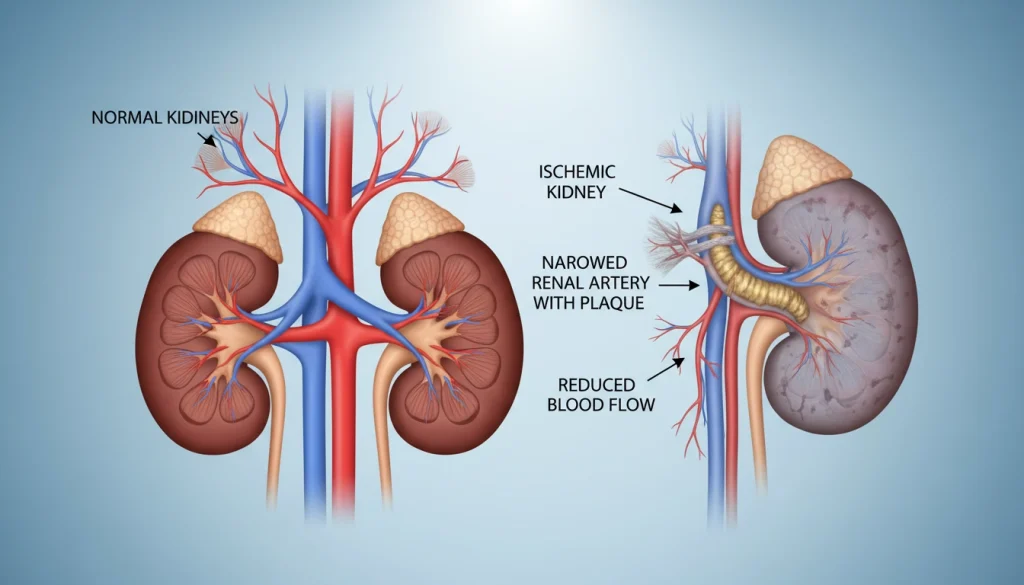
Renal Artery Stenosis is a serious medical condition where the narrowing of the renal arteries restricts blood flow to the kidneys. This condition can lead to severe hypertension and kidney damage. It potentially results in cardiovascular complications. Understanding the underlying causes, recognizing the symptoms, and exploring treatment options are key steps in managing Renal Artery Stenosis effectively. Early diagnosis and appropriate intervention are vital. They can significantly impact the prevention of long-term damage and improve patient outcomes.
Understanding Renal Artery Stenosis
Diving into the intricacies of Renal Artery Stenosis, we uncover the vital role of the renal arteries. These arteries are essential for delivering oxygen-rich blood to the kidneys. Any narrowing here can severely affect kidney function and overall health.
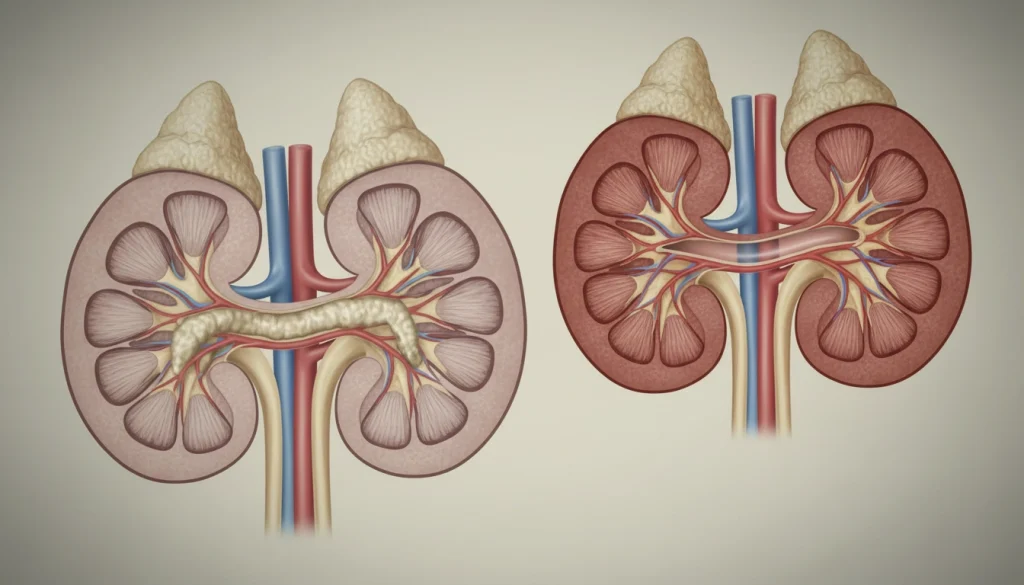
Definition and Basic Anatomy
Renal Artery Stenosis involves the narrowing of one or both renal arteries. These arteries are key for blood flow to the kidneys. The kidneys are vital for filtering waste, regulating blood pressure, and maintaining electrolyte balance. Originating from the aorta, the renal arteries are a critical part of the vascular system.
The renal arteries’ anatomy is complex, with variations in size, origin, and branching among individuals. Grasping this anatomy is vital for diagnosing and treating Renal Artery Stenosis effectively.
Prevalence and Significance
Renal Artery Stenosis is a significant condition, affecting certain populations more. It’s estimated that it impacts a notable percentage of those with hypertension and atherosclerosis. The condition is more prevalent in older adults and those with risk factors like smoking, diabetes, and high cholesterol.
- Renal Artery Stenosis is often linked to atherosclerosis, where plaque builds up in arteries.
- This condition can cause renovascular hypertension, a challenging high blood pressure to manage.
- Without treatment, Renal Artery Stenosis can lead to ischemic nephropathy, potentially causing kidney failure.
The importance of Renal Artery Stenosis lies in its ability to cause severe hypertension and kidney damage if untreated. Early detection and management are key to preventing long-term complications.
Anatomy of the Renal Arterial System
Understanding the renal arterial system’s anatomy is key for diagnosing and treating related conditions. This system is vital for the kidney’s vascular supply, essential for maintaining normal kidney function.
Normal Renal Artery Structure
The normal renal artery branches off from the aorta, splitting into segmental arteries. These segmental arteries then divide into lobar, interlobar, arcuate, and interlobular arteries. The arteries supply blood to the nephrons, the kidneys’ functional units. The anatomy of these arteries is complex, with variations in branching patterns among individuals.
Blood Flow Dynamics in Kidney Function
Blood flow dynamics are critical for kidney function. Alterations in flow can lead to significant pathophysiological changes. The kidneys receive about 20% of the cardiac output. The renal arteries deliver oxygenated blood to the nephrons. Changes in blood flow can impact kidney function, leading to conditions like renal artery stenosis.
Causes of Renal Artery Stenosis
Renal artery stenosis, a condition affecting kidney blood flow, has various causes. Understanding these is key to diagnosing and managing it effectively.
Atherosclerosis
Atherosclerosis is the leading cause of renal artery stenosis, mainly in older adults. It results from plaque buildup in arterial walls, narrowing or blocking the renal arteries. This mirrors coronary artery disease, where plaque can cause heart attacks. Risk factors include hypertension, diabetes, smoking, and high cholesterol.
Fibromuscular Dysplasia
Fibromuscular dysplasia (FMD) is a notable cause of renal artery stenosis, common in younger people. It involves abnormal growth in arterial walls, causing stenosis or aneurysms. It often affects the renal and internal carotid arteries. The cause of FMD is unknown, but it’s more common in women. Diagnosis relies on imaging studies.
Other Rare Causes
Rare causes of renal artery stenosis include vasculitis, congenital abnormalities, and external compression. Vasculitis is inflammation of blood vessels, leading to stenosis. Congenital issues involve abnormal renal artery development. External compression can result from tumors or masses. These are less common but should be considered in differential diagnosis, for patients with unusual symptoms.
Risk Factors for Developing Renal Artery Stenosis
Renal artery stenosis develops due to a mix of factors that can be changed and those that cannot. Knowing these factors is key to spotting those at high risk and taking steps to prevent it.
Modifiable Risk Factors
Modifiable risk factors play a big role in renal artery stenosis. These include high blood pressure, smoking, and high cholesterol. By changing lifestyle habits and using medication, these risks can be lowered.
- Hypertension: High blood pressure can damage the renal arteries, making them more susceptible to stenosis.
- Smoking: Smoking is a significant risk factor as it damages the vascular endothelium and promotes atherosclerosis.
- High Cholesterol: Elevated levels of low-density lipoprotein (LDL) cholesterol can lead to atherosclerotic plaque formation in the renal arteries.
Non-modifiable Risk Factors
There are also non-modifiable factors that raise the risk of renal artery stenosis. These include age, family history, and certain genetic conditions.
- Age: The risk of renal artery stenosis increases with age, significantly after 50.
- Family History: A family history of vascular disease can predispose individuals to renal artery stenosis.
- Genetic Conditions: Certain genetic conditions, such as fibromuscular dysplasia, can cause renal artery stenosis.
Pathophysiology of Renal Artery Stenosis
The pathophysiology of Renal Artery Stenosis is complex, involving mechanisms that impact blood pressure and kidney function. This condition reduces blood flow to the kidney, triggering a series of events with significant clinical implications.
Renin-Angiotensin-Aldosterone System Activation
Reduced renal perfusion activates the renin-angiotensin-aldosterone system (RAAS). The kidney releases renin in response to decreased blood flow. This enzyme initiates reactions leading to angiotensin II production, a potent vasoconstrictor. Angiotensin II increases blood pressure by constricting vessels and stimulates aldosterone release, promoting sodium retention and fluid buildup.
- Increased renin release due to reduced renal perfusion
- Conversion of angiotensinogen to angiotensin I by renin
- Angiotensin-converting enzyme (ACE) converts angiotensin I to angiotensin II
- Angiotensin II-mediated vasoconstriction and aldosterone release
Hemodynamic Changes
Hemodynamic changes are key in Renal Artery Stenosis pathophysiology. The stenosis causes a pressure drop, leading to decreased perfusion pressure in the distal renal artery. This reduction can decrease glomerular filtration rate (GFR) and activate the RAAS.
Progressive Kidney Damage
Progressive kidney damage occurs due to sustained ischemia and hypertension from Renal Artery Stenosis. Chronic reduction in renal perfusion causes parenchymal damage, fibrosis, and eventual loss of kidney function. Damage severity is related to stenosis degree and duration.
- Chronic ischemia leading to parenchymal damage
- Fibrosis and scarring within the affected kidney
- Potential for progression to chronic kidney disease or end-stage renal disease
Understanding Renal Artery Stenosis pathophysiology is vital for effective management. It requires addressing the stenosis and its effects on kidney function and blood pressure regulation.
Clinical Manifestations and Symptoms
Renal Artery Stenosis presents in various ways, often with hypertension that’s hard to manage. This condition can cause a range of symptoms, from high blood pressure to signs of kidney function decline. Recognizing these symptoms early is key to timely diagnosis and treatment.
Hypertension Patterns
Hypertension is a common symptom of Renal Artery Stenosis, often showing as resistant or refractory hypertension. This type of high blood pressure is challenging to control with usual treatments, needing multiple drugs or higher doses. The severity of hypertension varies among individuals.
- Resistant hypertension
- Accelerated hypertension
- Malignant hypertension
Kidney Function Abnormalities
Renal Artery Stenosis can cause kidney function issues, including a drop in glomerular filtration rate (GFR). This decrease in kidney function happens because the stenosis limits blood flow to the kidney. It’s vital to monitor kidney function in managing Renal Artery Stenosis.
Other Clinical Presentations
Patients with Renal Artery Stenosis may also experience other symptoms. These include flash pulmonary edema, a sudden onset of pulmonary edema, and various cardiovascular issues. The presence of these symptoms suggests the severity of the stenosis and the need for immediate action.
- Flash pulmonary edema
- Cardiovascular complications
- Signs of peripheral artery disease
Diagnostic Approaches for Renal Artery Stenosis
Diagnosing Renal Artery Stenosis requires a blend of clinical assessment and cutting-edge imaging. Accurate diagnosis is key to selecting the right treatment and improving patient outcomes.
Initial Clinical Evaluation
The first step in diagnosing Renal Artery Stenosis is a detailed clinical evaluation. This involves examining risk factors like hypertension, diabetes, and atherosclerosis. It also looks for symptoms that might point to renal artery stenosis.
Laboratory Tests
Laboratory tests are critical in the diagnostic process. They include serum creatinine and electrolytes to check kidney function. Other markers may indicate underlying conditions contributing to Renal Artery Stenosis.
Functional Tests
Functional tests, such as renal scintigraphy, assess the impact of Renal Artery Stenosis on kidney function. These tests help determine the stenosis’s significance and guide treatment choices.
Imaging Techniques
Imaging techniques are essential for visualizing the renal arteries and diagnosing Renal Artery Stenosis. Various modalities are available, each with its own strengths and limitations.
Doppler Ultrasound
Doppler ultrasound is a non-invasive method that uses sound waves to evaluate blood flow in the renal arteries. It’s a valuable initial screening tool due to its safety and relatively low cost.
CT Angiography
CT angiography uses computed tomography with contrast dye to visualize the renal arteries. It offers detailed images and is great for identifying stenosis and assessing its severity.
MR Angiography
MR angiography uses magnetic resonance technology to image the renal arteries without ionizing radiation. It’s beneficial for patients who can’t undergo CT angiography due to contrast allergy or kidney dysfunction.
Conventional Angiography
Conventional angiography, or digital subtraction angiography, is the gold standard for diagnosing Renal Artery Stenosis. It involves injecting contrast dye directly into the renal arteries through a catheter, providing precise images of the arterial anatomy.
By combining these diagnostic approaches, healthcare providers can accurately diagnose Renal Artery Stenosis. This allows for the development of an effective treatment plan tailored to the individual patient’s needs.
Classification and Grading Systems
Accurate classification of renal artery stenosis is essential for choosing the right treatment. Classification and grading systems ensure standardized diagnosis and guide treatment choices.
Severity Classification
The severity of renal artery stenosis is often determined by the percentage of narrowing. This classification is key in assessing the impact on kidney function and blood pressure.
- Mild stenosis:
- Moderate stenosis: 50-70% narrowing
- Severe stenosis: >70% narrowing
Knowing the severity is critical for deciding if intervention is needed and what type is best.
Anatomical Classification
Anatomical classification looks at the stenosis’s location and characteristics. It’s vital for planning the best interventional or surgical approach.
The anatomical details can affect the choice between endovascular treatment and surgical revascularization.
Complications of Untreated Renal Artery Stenosis
Untreated Renal Artery Stenosis can lead to severe and potentially life-threatening complications. The narrowing of the renal arteries can have far-reaching effects on kidney function and overall cardiovascular health. If left unaddressed, these complications can significantly impact the quality of life and increase the risk of mortality.
Renovascular Hypertension
One of the primary complications of untreated Renal Artery Stenosis is renovascular hypertension. This condition is characterized by high blood pressure due to the reduced blood flow to the kidneys. Managing renovascular hypertension can be challenging and may require multiple medications.
Ischemic Nephropathy
Prolonged reduction in blood flow to the kidneys can lead to ischemic nephropathy, a condition where the kidneys suffer from inadequate blood supply. This can result in irreversible kidney damage if not promptly addressed. Ischemic nephropathy is a significant concern in patients with untreated Renal Artery Stenosis.
Cardiovascular Complications
Untreated Renal Artery Stenosis also increases the risk of cardiovascular complications. The condition is associated with an increased risk of heart failure, coronary artery disease, and other cardiovascular events. The systemic nature of atherosclerosis, a common cause of Renal Artery Stenosis, contributes to these cardiovascular risks.
Flash Pulmonary Edema
Flash pulmonary edema is a life-threatening complication that can occur in patients with untreated Renal Artery Stenosis. Characterized by a sudden onset of pulmonary edema, this condition requires immediate medical attention. It is often associated with severe hypertension and can be recurrent if the underlying cause is not treated.
Medical Management of Renal Artery Stenosis
Managing Renal Artery Stenosis medically involves a detailed plan. It includes controlling blood pressure and slowing atherosclerosis growth. The main goals are to ease symptoms, slow disease advancement, and prevent heart issues.
Antihypertensive Medications
Antihypertensive drugs are key in managing Renal Artery Stenosis. RAAS inhibitors, like ACE inhibitors and ARBs, are beneficial. They control blood pressure and protect the kidneys. Yet, it’s vital to watch kidney function and potassium levels closely.
Other drugs, like calcium channel blockers and beta-blockers, may be used together. This helps achieve the best blood pressure control.
Lipid-Lowering Therapy
Lipid-lowering therapy is vital to slow atherosclerosis growth. Statins are the main drugs used. They help lower heart risks and slow atherosclerosis.
Antiplatelet Medications
Antiplatelet drugs, like aspirin and P2Y12 inhibitors, prevent blood clots. They are key in patients with Renal Artery Stenosis due to atherosclerosis.
Lifestyle Modifications
Lifestyle changes are essential in managing Renal Artery Stenosis. Quitting smoking is critical, as smoking accelerates atherosclerosis. Eating a low-sodium diet and managing weight also help control blood pressure and heart risks.
By using these strategies, healthcare providers can manage Renal Artery Stenosis well. This improves patient outcomes and lowers heart disease risks.
Interventional Treatment Options
Interventional treatments have become a cornerstone in managing Renal Artery Stenosis. These procedures aim to restore normal blood flow to the kidneys. This helps alleviate symptoms and prevents further kidney damage.
Percutaneous Transluminal Renal Angioplasty
Percutaneous Transluminal Renal Angioplasty (PTRA) is a minimally invasive procedure. It’s used to widen the stenosed renal artery. A balloon is used to dilate the narrowed segment.
PTRA is often considered for patients with significant stenosis. It’s for those who are symptomatic or have declining kidney function. The success of PTRA depends on several factors, including the severity and location of the stenosis, and the patient’s overall health.
While PTRA can be effective, it may not be suitable for all types of Renal Artery Stenosis. This is true for complex or extensive lesions.
Renal Artery Stenting
Renal Artery Stenting is another interventional approach. It involves placing a stent in the narrowed renal artery to maintain its patency. Stenting is often used in conjunction with PTRA to improve outcomes and reduce the risk of restenosis.
The decision to use stenting is based on the characteristics of the stenosis and the patient’s response to PTRA. Stenting has been shown to be beneficial in cases where PTRA alone is insufficient or when there is a high risk of restenosis.
Comparing Interventional Approaches
When comparing PTRA and stenting, several factors are considered. These include the technical success rate, complication rate, and long-term outcomes. Both procedures have their advantages and are chosen based on individual patient needs and the specific characteristics of the stenosis.
The choice between PTRA and stenting, or a combination of both, is made on a case-by-case basis. It’s based on the latest clinical guidelines and the expertise of the interventional team.
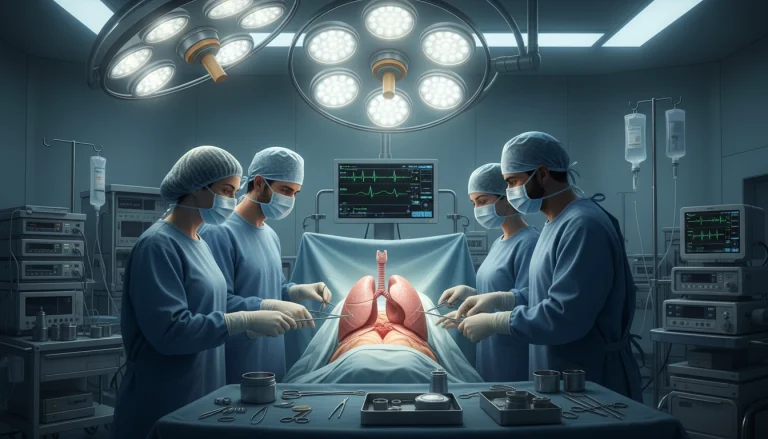
Surgical Management Strategies
Surgical approaches are vital for managing Renal Artery Stenosis, mainly in complex cases. When other treatments fail, surgery is needed to ensure blood flow to the kidneys.
Renal Artery Bypass
Renal artery bypass surgery creates a detour around the narrowed part of the artery. It’s beneficial for those with complex lesions or who didn’t respond to other treatments. The graft can come from the saphenous vein or internal iliac artery.
Endarterectomy
Endarterectomy removes plaque from the renal artery. This procedure enlarges the artery, improving blood flow to the kidney. It’s often chosen for severe stenosis due to atherosclerosis.
Nephrectomy in Advanced Cases
In severe cases, where the kidney is badly damaged, nephrectomy might be the only option. This is when the kidney fails and causes hypertension or other issues.
- Renal artery bypass is considered for complex lesions.
- Endarterectomy is used to remove plaque buildup.
- Nephrectomy is considered in cases of severe kidney damage.

Prognosis and Long-term Outcomes
The prognosis for patients with Renal Artery Stenosis is shaped by several factors. These include the severity of the stenosis and the chosen treatment’s effectiveness. Understanding these elements is vital for predicting long-term outcomes and guiding clinical management.
Factors Affecting Prognosis
Several key factors influence the prognosis of Renal Artery Stenosis. These include:
- The severity of the stenosis
- The underlying cause of the stenosis
- Kidney function at the time of diagnosis
- The presence of comorbid conditions, such as hypertension and diabetes
Assessing these factors helps clinicians predict the likelihood of disease progression and the presence of complications.
Outcomes After Medical Management
Medical management of Renal Artery Stenosis focuses on controlling hypertension, managing lipid profiles, and preventing disease progression. Outcomes can vary, with some patients experiencing:
- Stable kidney function
- Improved blood pressure control
- Reduced risk of cardiovascular events
Yet, the effectiveness of medical management hinges on patient compliance and the severity of the underlying condition.
Outcomes After Interventional Procedures
Interventional procedures, such as angioplasty and stenting, aim to restore blood flow to the kidneys. Outcomes after these procedures can include:
- Improved kidney function
- Better control of hypertension
- Reduced risk of disease progression
The success of interventional procedures depends on various factors. These include the technical success of the procedure and the patient’s overall health.
Current Research and Emerging Treatments
The field of Renal Artery Stenosis management is rapidly advancing. This is thanks to new medical research and technological breakthroughs. Recent studies aim to enhance diagnostic methods and introduce innovative treatments.
Advances in Diagnostic Techniques
New imaging technologies have greatly improved Renal Artery Stenosis diagnosis accuracy. Contrast-enhanced ultrasound and magnetic resonance angiography are gaining traction. They offer high sensitivity and specificity, making them valuable tools.
- Contrast-enhanced ultrasound
- Magnetic resonance angiography
- Computed tomography angiography
Novel Therapeutic Approaches
New treatments are being explored to better manage Renal Artery Stenosis. Drug-coated balloons and bioresorbable stents are being tested. They aim to lower restenosis risk and enhance patency rates.
Ongoing Clinical Trials
Clinical trials are underway to assess the effectiveness and safety of new Renal Artery Stenosis treatments. These trials are essential for shaping future management strategies.
- Trial evaluating the efficacy of drug-coated balloons
- Study comparing outcomes with bioresorbable stents versus conventional stents
- Research on the role of antiplatelet therapy in Renal Artery Stenosis management
Key Takeaways on Renal Artery Stenosis Management
Managing Renal Artery Stenosis effectively involves a multi-faceted strategy. This includes medical treatments, interventional procedures, and lifestyle changes. It’s vital to grasp the underlying causes, risk factors, and complications to ensure timely diagnosis and treatment. Advanced diagnostic tools like Doppler studies, CT scans, and MRI are indispensable for assessing kidney health and detecting vascular problems.
For detailed insights into diagnostic methods, visit Acibadem International.
A team effort between nephrology and radiology specialists is key to precise diagnosis and treatment planning. By focusing on the core aspects of managing Renal Artery Stenosis, healthcare professionals can significantly enhance patient outcomes. Personalized treatment plans, backed by cutting-edge imaging and interventional methods, are critical for maintaining optimal renal vascular health.
FAQ
Q: What is Renal Artery Stenosis?
A: Renal Artery Stenosis is a condition where the renal arteries narrow. These arteries are vital for supplying blood to the kidneys.
Q: What are the causes of Renal Artery Stenosis?
A: Atherosclerosis, fibromuscular dysplasia, and rare conditions like vasculitis and congenital abnormalities are common causes. These factors can lead to the narrowing of the renal arteries.
Q: What are the symptoms of Renal Artery Stenosis?
A: Symptoms include high blood pressure, kidney damage, and cardiovascular issues. Some may also experience sudden pulmonary edema.
Q: How is Renal Artery Stenosis diagnosed?
A: Diagnosis involves a thorough clinical evaluation and various tests. These include laboratory tests, functional assessments, and imaging techniques like Doppler ultrasound and CT angiography.
Q: What are the treatment options for Renal Artery Stenosis?
A: Treatment options include medication and interventional procedures. Medications manage blood pressure and cholesterol levels. Procedures like angioplasty and stenting help widen the arteries.
Q: What is the prognosis for patients with Renal Artery Stenosis?
A: Prognosis varies based on stenosis severity, kidney function, and treatment response. Effective management can significantly improve outcomes and reduce complications.
Q: Can Renal Artery Stenosis be prevented?
A: While some risks are unavoidable, managing modifiable factors like hypertension and high cholesterol can prevent stenosis. Lifestyle changes and medical therapy are key.
Q: What are the complications of untreated Renal Artery Stenosis?
A: Untreated stenosis can lead to high blood pressure, kidney damage, cardiovascular issues, and sudden pulmonary edema.
Q: What is the role of lifestyle modifications in managing Renal Artery Stenosis?
A: Lifestyle changes are critical in managing stenosis. Quitting smoking, dietary adjustments, and regular exercise help reduce complications.
Q: Are there any emerging treatments for Renal Artery Stenosis?
A: Yes, research is exploring new treatments. This includes drug-coated balloons and bioresorbable stents, which are being tested in clinical trials.