Renal Denervation: What is Renal Denervation?
Hypertension, or high blood pressure, is a major health issue affecting millions globally. It’s essential to manage it well to avoid heart disease and stroke. These complications can be life-threatening. Renal Denervation is a modern method for treating hypertension. It has drawn interest for its ability to help patients control their blood pressure. This is when other treatments have not worked.
This article will explore the specifics of Renal Denervation, its advantages, and its role in changing how we manage hypertension. By grasping this cutting-edge treatment, both healthcare professionals and patients can make better choices about its application. To grasp renal denervation, we must first understand its definition and physiological underpinnings. It’s a medical intervention aimed at treating hypertension. It works by disrupting the nerves in the kidneys that control blood pressure.
Definition and Basic Concept
Renal denervation employs a catheter-based system to ablate the nerves around the renal arteries. This method is grounded in the belief that the sympathetic nervous system heavily influences blood pressure.
The Physiological Basis
The core of renal denervation’s effectiveness lies in its impact on the sympathetic nervous system and the kidney-brain connection.
Sympathetic Nervous System’s Role
The sympathetic nervous system plays a vital role in blood pressure regulation. It does so through mechanisms like vasoconstriction and heart rate modulation. In cases of hypertension, this system tends to be overactive.
Kidney-Brain Connection in Blood Pressure Regulation
The kidneys and the brain communicate through the renal nerves, affecting blood pressure. By disrupting these nerves, blood pressure can decrease.
Renal denervation’s success in managing hypertension stems from its ability to block harmful signals between the kidneys and the brain. This interruption leads to a reduction in blood pressure.
The History and Evolution of Renal Denervation
Renal denervation, a procedure for treating resistant hypertension, has a long and evolving history. The idea has been around for decades. Yet, its modern application is a more recent development.
Early Research and Development
Initial research into renal denervation aimed to understand the role of renal nerves in blood pressure control. Studies showed that these nerves are vital in managing sympathetic nerve activity. This activity is often heightened in those with hypertension.
Key Milestones in Clinical Application
The first human trials on renal denervation began in the early 2000s. They showed promising results in lowering blood pressure in patients with resistant hypertension. Following studies further confirmed the procedure’s safety and effectiveness.
FDA Approval Journey
The path to FDA approval for renal denervation devices has been long and challenging. Several devices have received approval for use in the U.S. The approval process required extensive clinical trials. These trials aimed to prove the safety and efficacy of these devices.
The history and evolution of renal denervation highlight its promise as a treatment for resistant hypertension.
The Science Behind Renal Denervation
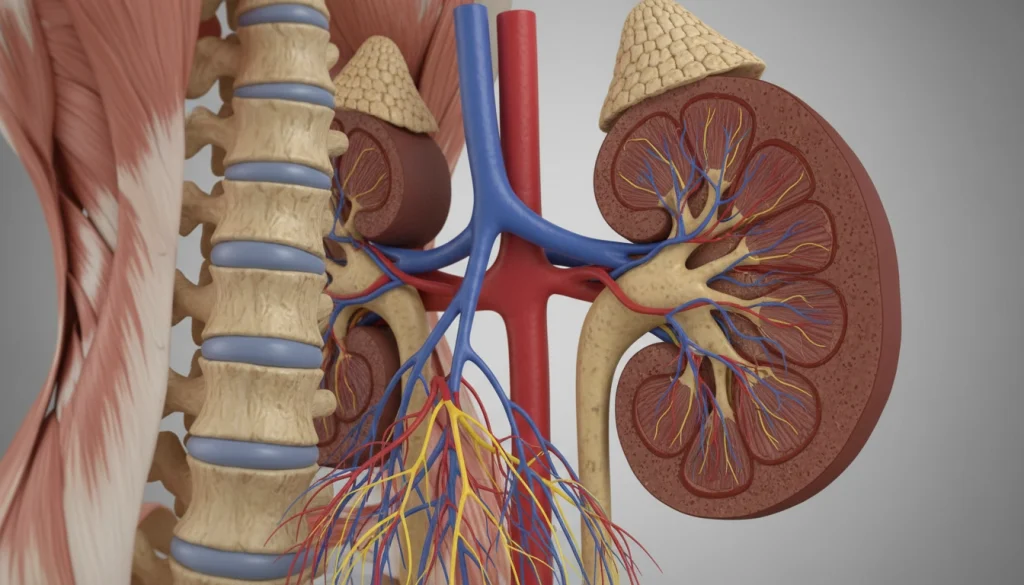
To grasp the science of Renal Denervation, we must explore renal nerve anatomy, hypertension’s pathophysiology, and how it lowers blood pressure. This procedure targets the renal nerves, essential for blood pressure control.
Renal Nerve Anatomy and Function
Renal nerves form a complex network of sympathetic and afferent fibers that cover the kidneys. They regulate kidney functions like sodium absorption, renin release, and blood vessel tone. The sympathetic renal nerves are key players in hypertension.
Pathophysiology of Hypertension
Hypertension is a complex disorder with elevated blood pressure. It involves genetics, environment, and neurohormonal interactions. Renal nerves significantly influence this, affecting blood pressure through kidney modulation.
Mechanism of Blood Pressure Reduction
Renal Denervation works by disrupting sympathetic renal nerves, reducing kidney sympathetic drive. This leads to several positive outcomes.
Immediate Effects
Right after Renal Denervation, there’s a drop in sympathetic nerve activity. This decrease in renin release and sodium absorption lowers blood pressure.
Long-term Physiological Adaptations
Long-term, Renal Denervation causes sustained blood pressure drops through physiological changes. These include reduced renal vascular resistance and enhanced baroreflex sensitivity. These adaptations make Renal Denervation effective in managing hypertension.
Types of Renal Denervation Techniques
Several renal denervation techniques have emerged, providing various options for those with hypertension. These methods differ in how they disrupt the renal nerves that contribute to high blood pressure.
Radiofrequency Ablation Methods
Radiofrequency ablation is a common technique in renal denervation. It employs radiofrequency energy to ablate the renal nerves.
Single-electrode Systems
Single-electrode systems were among the first developed. They use a single catheter to deliver radiofrequency energy to the renal artery.
Multi-electrode Systems
Multi-electrode systems are an advancement. They allow for more thorough coverage of the renal nerves through simultaneous ablation at multiple points.
Ultrasound-Based Approaches
Ultrasound-based renal denervation is another technique. It uses ultrasound energy to target the renal nerves. This method may offer a different safety and efficacy profile compared to radiofrequency ablation.
Chemical Denervation Methods
Chemical denervation involves using chemicals to disrupt the renal nerves. This approach is in the early stages of research but shows promise as an alternative to energy-based methods.
Emerging Technologies
The field of renal denervation is constantly evolving. Several emerging technologies are being explored. These include new catheter designs and alternative energy sources aimed at improving the procedure’s efficacy and safety.
The Renal Denervation Procedure in Detail
Understanding the renal denervation procedure is key for those considering it. This treatment involves several steps, from initial evaluation to post-procedure care. It’s a complex process.
Pre-Procedure Evaluation and Testing
Before starting, patients undergo a detailed evaluation. This checks if they’re right for the treatment. The evaluation includes:
- Medical history review
- Blood pressure monitoring
- Renal function tests
- Imaging studies to assess renal anatomy
This thorough assessment identifies risks and confirms the patient’s suitability.
Step-by-Step Procedure Overview
The renal denervation procedure has several key steps:
Anesthesia and Patient Preparation
The procedure is done under local anesthesia, with or without sedation. This aims to reduce discomfort.
Catheter Insertion and Positioning
A catheter is inserted through the femoral artery. It’s guided to the renal arteries using imaging techniques.
Ablation Process
With the catheter in place, ablation disrupts the renal nerves. The ablation method varies by technology used.
Post-Procedure Monitoring
After the procedure, patients are closely monitored. This checks for immediate complications and the treatment’s initial effect.
Recovery Timeline
The recovery from renal denervation is generally quick. Most patients can return to normal activities within a few days. Yet, recovery times can differ based on individual factors and the procedure specifics.
Ideal Candidates for Renal Denervation
Identifying the right candidates for renal denervation is key to its success. This procedure has shown promise in treating resistant hypertension. Yet, its effectiveness largely hinges on selecting patients carefully.
Diagnostic Criteria for Resistant Hypertension
Resistant hypertension is defined as blood pressure that stays high despite three antihypertensive drugs, including a diuretic, at their highest doses. To qualify for renal denervation, patients must meet certain criteria. These include:
- Office blood pressure measurements ≥140/90 mmHg
- Confirmation of adherence to prescribed antihypertensive medication
- Exclusion of secondary causes of hypertension
Patient Selection Guidelines
Several factors are considered when selecting patients for renal denervation:
Age Considerations
Age is a significant factor, though there’s no strict age limit. Most studies focus on adults under 80.
Comorbidity Factors
Patients with conditions like diabetes, kidney disease, or heart disease are evaluated individually. These conditions can affect the decision to proceed with renal denervation.
Contraindications
Some conditions make renal denervation unsuitable. These include:
Absolute Contraindications
- Significant renal artery stenosis or other vascular abnormalities
- Prior renal artery intervention or stenting
Relative Contraindications
- Type 2 diabetes with significant kidney damage
- Severe kidney disease or chronic kidney disease stage 4 or 5
Evaluating these factors is critical to determine if a patient is suitable for renal denervation.
Clinical Outcomes and Effectiveness
Renal denervation has shown promise in treating resistant hypertension. Studies have focused on its ability to lower blood pressure. This has been a key area of research.
Short-Term Blood Pressure Reduction
Initial studies indicate renal denervation can effectively reduce blood pressure in the short term. A meta-analysis of several trials found systolic blood pressure dropped by an average of 10 mmHg within six months post-procedure.
Long-Term Efficacy Data
Long-term data on renal denervation’s effectiveness is also positive. Research suggests its blood pressure-lowering effects can last up to three years or more after the procedure.
Predictors of Treatment Success
Identifying predictors of successful treatment outcomes is essential. Factors such as baseline blood pressure, renal function, and comorbidities have been studied as predictors.
Non-Responder Phenomenon
Despite its overall effectiveness, a subset of patients does not respond to renal denervation. This phenomenon is known as non-response.
Potential Causes
- Incomplete denervation
- Underlying secondary causes of hypertension
- Advanced vascular stiffness
Management Strategies
Managing non-responders requires a multi-faceted approach. This includes re-evaluating the patient’s hypertension etiology and considering alternative or adjunctive treatments.
The effectiveness of renal denervation in clinical practice is supported by a growing body of evidence. Ongoing research aims to refine patient selection criteria and improve treatment outcomes.
Benefits of Renal Denervation Beyond Blood Pressure
Renal Denervation is a groundbreaking treatment for hypertension, showing benefits beyond just lowering blood pressure. It’s not just about managing high blood pressure; it positively impacts overall health. By reducing sympathetic nerve activity, it addresses various cardiovascular health aspects.
Reduction in Medication Burden
One key advantage of Renal Denervation is the reduction in medication for patients with resistant hypertension. This procedure can help patients decrease their need for multiple antihypertensive drugs. It simplifies treatment and boosts adherence.
Metabolic Effects
Renal Denervation also has positive metabolic effects, such as better insulin sensitivity and glucose metabolism. These benefits are critical for patients with hypertension and metabolic syndrome risk.
Cardiovascular Risk Reduction
By lowering blood pressure and sympathetic nerve activity, Renal Denervation reduces cardiovascular risk factors. This decrease can lower the risk of heart attacks, strokes, and kidney disease progression.
Quality of Life Improvements
Patients who get Renal Denervation often see their quality of life improve. The drop in blood pressure and medication burden, along with metabolic benefits, enhances overall well-being. It encourages a more active lifestyle.
In conclusion, Renal Denervation’s benefits go beyond just lowering blood pressure. It offers a wide range of health improvements that can greatly impact patients’ lives. As research advances, these benefits will become even clearer, solidifying Renal Denervation as a valuable hypertension treatment.
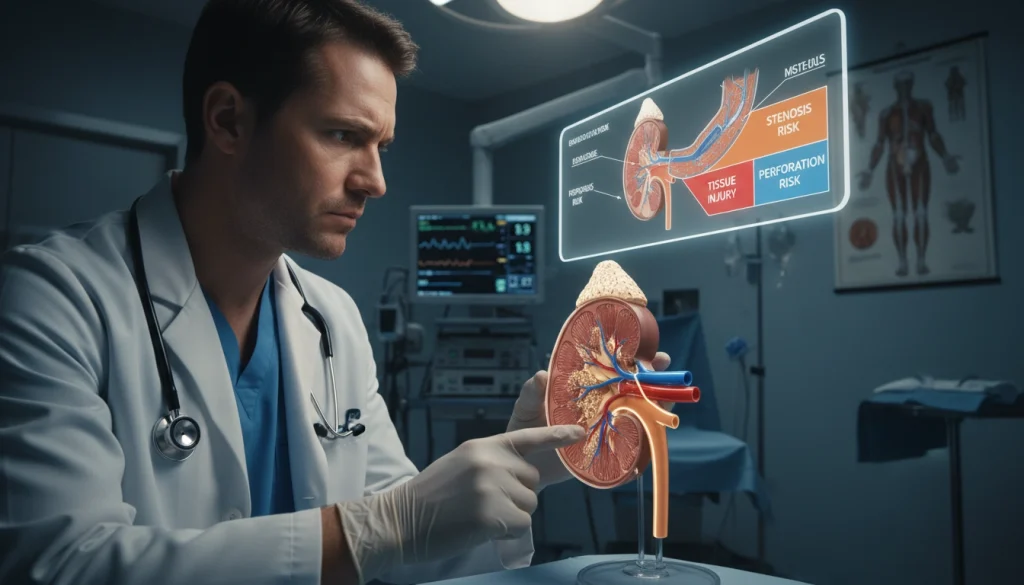
Potential Risks and Complications
Renal denervation, a procedure gaining traction for hypertension treatment, is not without its risks and complications. As with any medical intervention, understanding these risks is key for informed decision-making.
Procedure-Related Complications
Complications can arise during or immediately after renal denervation. These are often tied to the technical aspects of the procedure.
Vascular Access Issues
Vascular access issues, such as bleeding or hematoma at the access site, are among the complications. Proper technique and post-procedure care can help minimize these risks.
Renal Artery Damage
Renal artery damage is a serious complication that can occur during the procedure. This highlights the need for precise technique and experienced practitioners.
Post-Procedure Side Effects
Patients may experience side effects after the procedure, ranging from mild discomfort to serious conditions. Monitoring and follow-up care are critical to manage these side effects effectively.
Long-Term Safety Considerations
The long-term safety of renal denervation is an area of ongoing research. As a relatively new procedure, continued monitoring of patients is necessary to fully understand its long-term implications.
Risk Mitigation Strategies
To minimize the risks associated with renal denervation, several strategies can be employed. These include careful patient selection, thorough pre-procedure evaluation, and adherence to best practices during and after the procedure.
By understanding the risks and complications and implementing strategies to mitigate them, healthcare providers can offer renal denervation as a safe and effective treatment option for appropriate candidates.
Renal Denervation Compared to Traditional Treatments
When looking at treatments for high blood pressure, it’s key to compare Renal Denervation with traditional pharmacological therapy. This comparison sheds light on the pros and cons of each method.
Pharmacological Therapy vs. Renal Denervation
Pharmacological therapy has been a mainstay in managing hypertension. Yet, Renal Denervation offers a new interventional strategy that has drawn considerable interest.
Efficacy Comparison
Research indicates that Renal Denervation can effectively lower blood pressure in those with resistant hypertension. On the other hand, pharmacological therapy works well for many but its success varies by patient and medication.
Side Effect Profiles
The side effect profiles of Renal Denervation and pharmacological therapy differ significantly. Pharmacological treatments can lead to numerous side effects due to their systemic impact. In contrast, Renal Denervation, being a targeted procedure, generally has fewer systemic side effects.
Cost-Effectiveness Analysis
Assessing the cost-effectiveness of Renal Denervation versus long-term pharmacological therapy is vital. The initial cost of the procedure might be high, but the long-term savings from reduced medication could make it cost-effective for some.
Patient Preference Considerations
Patient preferences are a significant factor in choosing between Renal Denervation and pharmacological therapy. Some patients might prefer a procedural solution to avoid the daily pill burden. Others might prefer the familiarity of pharmacological treatments.
In summary, comparing Renal Denervation with traditional pharmacological treatments reveals the distinct advantages and considerations of each. Grasping these differences is essential for making informed decisions in managing hypertension.
Latest Research and Clinical Trials
The latest research on renal denervation is shedding light on its role in managing hypertension and beyond. Recent studies have greatly enhanced our understanding of this procedure. They have shown its efficacy and its wide-ranging applications.
Recent Landmark Studies
Several landmark studies have significantly influenced the field of renal denervation. The SYMPLICITY HTN trials and the SPYRAL HTN studies have been instrumental. They have provided vital insights into the procedure’s safety and effectiveness.
SYMPLICITY HTN Trials
The SYMPLICITY HTN trials were groundbreaking. They demonstrated renal denervation’s promise in treating resistant hypertension. The trials revealed significant blood pressure reductions among participants.
SPYRAL HTN Studies
The SPYRAL HTN studies built upon the SYMPLICITY HTN findings. They explored renal denervation’s effects on various patient groups. This expanded our understanding of its applications.
Ongoing Research Initiatives
Research into renal denervation is ongoing, pushing the boundaries of what is possible. Current studies are examining the procedure’s long-term benefits. They aim to uncover its advantages for different patient populations.
Emerging Applications Beyond Hypertension
Renal denervation is being explored for uses beyond hypertension. It is being considered for treating heart failure, arrhythmias, and metabolic disorders. This broadens its therapeutic scope.
Heart Failure
Research into renal denervation for heart failure is promising. Early results suggest it could improve patient outcomes. This is an exciting area of investigation.
Arrhythmias
Renal denervation’s application in managing arrhythmias is also being studied. Researchers are examining its impact on heart rhythm. This could lead to new treatments for arrhythmias.
Metabolic Disorders
Studies are also exploring renal denervation’s role in managing metabolic disorders. Preliminary findings suggest it could have a broader therapeutic role. This opens up new possibilities for treatment.
As research progresses, renal denervation’s role in clinical practice is expected to grow. It will likely offer new treatment options for patients with various cardiovascular conditions.
Insurance Coverage and Financial Considerations
Understanding insurance for Renal Denervation is complex, with many factors at play. It’s vital for those considering this treatment to grasp the financial implications.
Current Reimbursement Landscape in the US
The US reimbursement for Renal Denervation is changing. Recent updates have broadened coverage, yet differences persist among insurance companies.
Medicare and Medicaid Coverage
Medicare and Medicaid do cover Renal Denervation under specific conditions. It’s important for patients to check their coverage details.
Private Insurance Policies
Private insurance policies on Renal Denervation vary widely. Some may cover it, while others do not. Key points to consider include:
- Verify if your policy includes Renal Denervation.
- Understand the costs you’ll face out-of-pocket.
- Review any pre-approval or pre-authorization needs.
Patient Assistance Programs
There are patient assistance programs to help with Renal Denervation costs. These programs offer financial support and relief.

Patients must discuss their insurance and financial options with their healthcare provider. This ensures they make informed decisions about their treatment.
Finding Specialized Renal Denervation Centers
The journey to undergo Renal Denervation starts with finding a qualified medical facility. It’s vital for patients to locate a center with experience in the procedure. They should also have a team ready to provide full care.
Identifying Qualified Providers
When searching for a Renal Denervation center, look for institutions with a proven track record. This includes:
- Experienced interventional cardiologists or radiologists
- A multidisciplinary team approach to patient care
- State-of-the-art facilities and equipment
Checking for certifications and accreditations from reputable bodies can also provide assurance of the center’s quality.
Questions to Ask Your Healthcare Team
Before committing to a Renal Denervation procedure, it’s essential to have an open dialogue with your healthcare provider. Consider asking:
- What experience do you have with Renal Denervation?
- What are the possible risks and complications?
- How will my progress be monitored after the procedure?
Preparing for Consultations
To make the most out of your consultation, prepare by:
- Gathering all relevant medical records
- Listing your medications and dosages
- Writing down your questions and concerns
Referral Process Navigation
Navigating the referral process can sometimes be complex. Ensure you understand the steps involved and the timeline for your procedure.
By taking these steps, patients can confidently find a specialized Renal Denervation center that meets their needs. This ensures the best possible outcome.
The Future of Hypertension Management and Renal Denervation
The field of hypertension management is rapidly evolving, with Renal Denervation at the forefront. This treatment is gaining traction as research progresses. It’s expected to play a larger role in managing hypertension.
Recent studies have highlighted Renal Denervation’s effectiveness in lowering blood pressure for those with resistant hypertension. With ongoing research and new applications, its possibilities are immense.
Looking ahead, hypertension management will likely focus more on personalized care. Renal Denervation will be considered for certain patients. As the medical community delves deeper into its benefits and risks, its place in treatment plans will become clearer.
Technological and procedural advancements will enhance Renal Denervation’s safety and effectiveness. This will make it a viable option for more patients. The future of hypertension management will be shaped by innovative treatments like Renal Denervation.
FAQ
Q: What is Renal Denervation?
A: Renal Denervation is a minimally invasive procedure. It aims to treat resistant hypertension by disrupting the nerves in the kidneys that contribute to high blood pressure.
Q: How does Renal Denervation work?
A: Renal Denervation works by ablating the renal nerves, which are part of the sympathetic nervous system. This system plays a significant role in regulating blood pressure. By reducing the activity of these nerves, Renal Denervation can help lower blood pressure.
Q: What are the benefits of Renal Denervation beyond lowering blood pressure?
A: Beyond lowering blood pressure, Renal Denervation has been associated with a reduction in medication burden. It also improves metabolic effects, reduces cardiovascular risk, and enhances quality of life.
Q: What are the potentially risks and complications of Renal Denervation?
A: The procedure may involve procedure-related complications such as vascular access issues and renal artery damage. Post-procedure side effects and long-term safety considerations are also concerns.
Q: Is Renal Denervation covered by insurance?
A: Insurance coverage for Renal Denervation varies. In the US, coverage is available under certain conditions through Medicare, Medicaid, and some private insurance policies. Patient assistance programs may also be available.
Q: How do I find a qualified provider for Renal Denervation?
A: To find a qualified provider, start by asking your primary care physician for a referral. You can also check with professional medical organizations or patient advocacy groups for recommendations.
Q: What should I expect during the Renal Denervation procedure?
A: The procedure involves pre-procedure evaluation, anesthesia, catheter insertion, and the ablation process. Post-procedure monitoring and a recovery timeline will also be part of your experience.
Q: Are there any contraindications for Renal Denervation?
A: Yes, there are absolute and relative contraindications. These include certain vascular conditions, kidney diseases, and other health issues that may make the procedure risky or unsuitable.
Q: Can Renal Denervation be used for conditions other than hypertension?
A: Emerging research is exploring the use of Renal Denervation for conditions beyond hypertension. This includes heart failure, arrhythmias, and metabolic disorders.
Q: What does the future hold for Renal Denervation in hypertension management?
A: The future of Renal Denervation looks promising. Ongoing research and advancements are likely to expand its role in managing hypertension and potentially other related conditions.















