Retinopathy: What is Retinopathy?
Retinopathy impacts the retina, the light-sensitive tissue at the back of the eye. It can cause vision issues and, if untreated, may lead to blindness. This condition is commonly linked to diabetes but can also stem from other causes. Symptoms include blurred vision, floaters, and night vision difficulties. Treatment varies based on the cause and severity. Options range from lifestyle adjustments and medication to surgery.
Grasping retinopathy is key for early detection and effective management. This piece will explore its causes, symptoms, and treatment options. It aims to provide a detailed look at this critical eye condition. Retinopathy is a group of disorders that harm the retina, the light-sensitive tissue at the back of the eye. It can cause significant vision problems and, if untreated, severe vision loss. Understanding retinopathy is key for early detection and treatment.
Definition and Basic Mechanisms
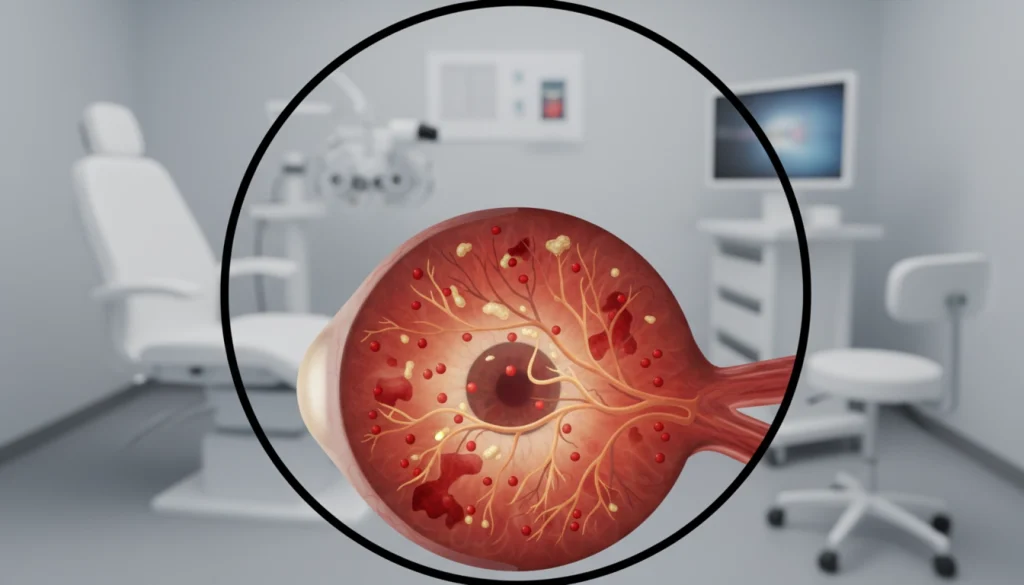
Retinopathy damages the retina’s blood vessels, leading to bleeding or fluid leakage. This distorts vision. The retina converts light into signals for the brain, enabling us to see. When retinopathy strikes, it can disrupt this process, potentially causing blindness. Factors like diabetes, hypertension, and other heart conditions play a role in retinopathy.
Impact on Vision and Quality of Life
Retinopathy’s impact on vision can vary, from mild disturbances to complete blindness. As it worsens, it can significantly affect daily life. Simple tasks like reading, driving, and recognizing faces become hard, leading to loss of independence. The psychological toll of vision loss is also significant, causing depression and anxiety. Early detection and management are vital to prevent these effects and preserve vision.
Types of Retinopathy
It’s vital to grasp the various forms of retinopathy for accurate diagnosis and treatment. This condition affects the retina, leading to several complications. Each type has its own set of characteristics and treatment needs.
Diabetic Retinopathy
Diabetic retinopathy is a common diabetes complication, damaging the retina’s blood vessels. It’s a major cause of blindness in adults.
Non-proliferative Diabetic Retinopathy
Non-proliferative diabetic retinopathy (NPDR) is the initial stage, featuring microaneurysms, hemorrhages, and exudates. It’s the early phase of diabetic retinopathy.
Proliferative Diabetic Retinopathy
Proliferative diabetic retinopathy (PDR) is a more severe stage. It’s characterized by the growth of new, fragile blood vessels. This can cause severe vision loss if untreated.
Hypertensive Retinopathy
Hypertensive retinopathy results from high blood pressure damaging the retina’s blood vessels. It can lead to vision issues and is linked to cardiovascular diseases.
Other Forms of Retinopathy
There are other significant retinopathy types, each affecting different groups.
Retinopathy of Prematurity
Retinopathy of prematurity (ROP) affects premature babies, causing abnormal blood vessel growth in the retina. It can result in blindness if not treated quickly.
Central Serous Retinopathy
Central serous retinopathy (CSR) involves fluid accumulation under the retina, causing visual distortion. It’s prevalent among young and middle-aged adults.
Each retinopathy type has unique features and treatment approaches. Recognizing these differences is essential for effective management and preventing vision loss.
Causes and Risk Factors of Retinopathy
Several factors contribute to the risk of developing retinopathy, including diabetes, hypertension, and genetic predisposition. Understanding these causes is essential for effective prevention and management strategies.
Diabetes as a Primary Cause
Diabetes is recognized as a primary cause of retinopathy, with diabetic retinopathy being a notable example. High blood sugar levels over time can damage the blood vessels in the retina, leading to vision problems. Managing diabetes through lifestyle changes and medication is critical in preventing diabetic retinopathy.
Hypertension and Cardiovascular Factors
Hypertension, or high blood pressure, is another significant risk factor for retinopathy. It can cause hypertensive retinopathy by damaging the blood vessels in the retina. Controlling hypertension through lifestyle modifications and, if necessary, medication can help mitigate this risk.
Other Contributing Factors
Besides diabetes and hypertension, other factors can contribute to the development of retinopathy. These include genetic predisposition and environmental factors.
Genetic Predisposition
Genetic predisposition plays a role in the susceptibility to certain forms of retinopathy. Individuals with a family history of retinopathy or related conditions may be at higher risk.
Environmental Factors
Environmental factors, such as exposure to certain toxins or having a poor diet, can also influence the risk of developing retinopathy. Maintaining a healthy lifestyle is important for overall eye health.
Signs and Symptoms of Retinopathy
Understanding the signs and symptoms of retinopathy is key for early detection and effective management. This condition can progress significantly before noticeable symptoms appear. Awareness of its early signs is vital.
Early Warning Signs
Early warning signs of retinopathy include subtle changes in vision, such as blurred vision or difficulty seeing colors. Individuals may also notice floaters, which are spots or dark strings floating in their field of vision. Regular eye exams are essential for detecting these changes early.
Progressive Symptoms
As retinopathy progresses, symptoms become more pronounced. Vision may continue to blur, and the presence of floaters can increase. In some cases, individuals may experience vision loss, which can be partial or complete, depending on the severity of the condition.
Emergency Symptoms Requiring Immediate Attention
Certain symptoms require immediate medical attention, such as sudden vision loss, severe eye pain, or flashes of light. These could indicate advanced retinopathy or complications like retinal detachment, which is a medical emergency.
Stages of Retinopathy Progression
Understanding how retinopathy progresses is key to managing and treating it effectively. This condition, which damages the retina, goes through several stages. Each stage has its own impact on vision and eye health.
Mild to Moderate Stages
In the early stages, symptoms might be slight, but neglect can lead to worsening.
- Mild non-proliferative diabetic retinopathy (NPDR) shows as small swellings in the retina’s blood vessels.
- Moderate NPDR sees more widespread vascular changes, including blockages and increased retinal ischemia.
Severe and Proliferative Stages
As retinopathy worsens, it can cause severe complications, including proliferative diabetic retinopathy (PDR).
- Severe NPDR is marked by significant vascular obstruction and retinal hypoxia.
- PDR is characterized by the growth of new, fragile blood vessels in the retina, which can lead to vitreous hemorrhage or retinal detachment.
End-Stage Complications
The final stages of retinopathy can cause severe and irreversible vision loss if untreated.
- Advanced diabetic eye disease can lead to complications such as vitreous hemorrhage, retinal detachment, and neovascular glaucoma.
- Prompt treatment can help mitigate some of these complications, highlighting the importance of regular eye exams.
Diagnosis of Retinopathy
Diagnosing retinopathy requires a detailed approach, including various eye exams and tests. Accurate diagnosis is key for effective treatment and management.
Comprehensive Eye Examinations
Comprehensive eye exams are the initial step in diagnosing retinopathy. These exams include a detailed medical history, visual acuity tests, and a thorough retina check. Professionals look for signs like microaneurysms, hemorrhages, and exudates.
Diagnostic Imaging Techniques
Diagnostic imaging is essential in retinopathy diagnosis. These methods help detect the condition and assess its severity.
Fluorescein Angiography
Fluorescein angiography involves injecting fluorescent dye into the bloodstream. This dye highlights the retina’s blood vessels, allowing professionals to spot abnormalities.
Optical Coherence Tomography
Optical coherence tomography (OCT) is a non-invasive test that captures high-resolution retina images. It detects retinal thickening, fluid accumulation, and other retinopathy signs.

Laboratory Tests and Assessments
Laboratory tests, like blood glucose and lipid profiles, are vital. They help identify underlying causes of retinopathy. These tests are essential for diagnosing diabetes or other conditions contributing to retinopathy.
In conclusion, diagnosing retinopathy involves eye exams, imaging techniques, and lab tests. Early detection and diagnosis are critical for preventing vision loss and managing the condition effectively.
Treatment Options for Retinopathy
Understanding the various treatments for retinopathy is key. This includes medical, laser, and surgical options. The right treatment depends on the type and severity of the condition, along with the patient’s health.
Medical Management
Medical management is often the first step. It aims to control the underlying causes of retinopathy.
Anti-VEGF Therapy
Anti-vascular endothelial growth factor (VEGF) therapy is a common treatment. It’s used for diabetic retinopathy and other forms. This therapy involves injecting drugs to reduce vascular leakage and prevent vision loss.
Corticosteroid Medications
Corticosteroids help reduce inflammation in the retina. They can be injected or implanted. This provides targeted treatment with fewer side effects.
Laser Therapy and Surgical Interventions
For advanced retinopathy, laser therapy and surgery may be needed. These treatments aim to prevent further vision loss.
Panretinal Photocoagulation
Panretinal photocoagulation (PRP) is a laser treatment. It destroys ischemic areas of the retina. This is often used for proliferative diabetic retinopathy.
Vitrectomy
Vitrectomy involves removing the vitreous gel from the eye. It’s used for complications like vitreous hemorrhage or retinal detachment.
Emerging Treatments and Clinical Trials
New treatments for retinopathy are being researched. This includes gene therapy, stem cell therapy, and new drugs.
- Gene therapy targets genetic causes of retinopathy.
- Stem cell therapy aims to repair damaged retinal tissue.
- New drugs are being developed to target specific pathways in retinopathy.
These emerging treatments offer hope for better outcomes for patients with retinopathy.
Prevention Strategies for Retinopathy
Preventing retinopathy requires a multi-faceted approach. It involves controlling blood sugar, managing blood pressure, and adopting a healthy lifestyle. Understanding the risk factors and taking proactive steps can greatly lower the chance of developing retinopathy.
Blood Sugar Management for Diabetic Patients
For those with diabetes, managing blood sugar is key to preventing retinopathy. This means regular glucose monitoring, following medication schedules, and adjusting diets as needed. Keeping blood sugar levels in check can prevent diabetic retinopathy from developing or worsening.
- Monitor blood glucose regularly
- Adhere to prescribed medication
- Make informed dietary choices
Blood Pressure Control
Hypertension is a major risk factor for retinopathy. Controlling blood pressure through lifestyle changes and, if needed, medication is essential. Regular blood pressure checks and a healthy lifestyle are critical for preventing retinopathy.
- Regularly check blood pressure
- Adopt a low-sodium diet
- Engage in regular physical activity
Lifestyle Modifications and Preventive Care
Making lifestyle changes is vital for preventing retinopathy. This includes eating a healthy diet, staying physically active, and avoiding smoking.
Nutrition and Diet
Eating a balanced diet rich in fruits, vegetables, and omega-3 fatty acids supports eye health. The right nutrition can help manage blood sugar and blood pressure, both critical for reducing retinopathy risk.
Exercise and Physical Activity
Regular exercise is beneficial for managing blood sugar and blood pressure. It also boosts overall health. Activities like walking, cycling, and swimming are great for staying physically fit.
By adopting these prevention strategies, individuals can significantly lower their risk of retinopathy. Regular eye exams and consultations with healthcare providers are also vital for a complete prevention plan.
Complications of Untreated Retinopathy
Treating retinopathy is critical, as ignoring it can lead to severe consequences. Neglecting retinopathy can severely harm vision and eye health, potentially causing permanent damage.
Vision Loss and Blindness
Untreated retinopathy can cause vision loss, potentially leading to blindness. The severity of retinopathy, presence of other eye issues, and treatment effectiveness are key risk factors.
- Severe vision impairment
- Increased risk of blindness
- Reduced quality of life
Secondary Eye Conditions
Retinopathy can also trigger secondary eye conditions, complicating eye health further. Macular edema and retinal detachment are two notable conditions that can arise.
Macular Edema
Macular edema involves fluid buildup in the macula, causing swelling. This can distort vision and, in severe cases, lead to significant vision loss.
Retinal Detachment
Retinal detachment occurs when the retina separates from the underlying tissue. It’s a medical emergency that requires immediate attention to prevent permanent vision loss.
Impact on Overall Health
Untreated retinopathy’s effects extend beyond vision. It’s often linked to conditions like diabetes and hypertension. These can lead to cardiovascular and renal issues if not managed well.
- Increased risk of cardiovascular disease
- Potential for kidney damage
- Impact on overall well-being
Living with Retinopathy
Receiving a retinopathy diagnosis can be a turning point in life. Yet, with the right strategies, one can adapt. It involves a holistic approach, including adapting to vision changes, leveraging support resources, and managing the psychological effects of the condition.
Adapting to Vision Changes
Adapting to vision changes is a significant challenge for those with retinopathy. Symptoms like blurred vision, blind spots, and night blindness can occur. To cope, individuals can use assistive devices such as magnifying glasses, enhanced lighting, and specialized software on digital devices.
Making simple adjustments, like increasing font size on digital devices and using contrasting colors, can greatly improve visibility. Regular eye exams are vital to track the condition’s progression and adjust strategies as needed.
Support Resources and Assistive Technologies
There are many support resources and assistive technologies for individuals with retinopathy. Support groups, both online and in-person, offer a community where people can share experiences and learn from others. These groups provide invaluable support and advice.
Assistive technologies range from basic tools like white canes and magnifying glasses to advanced software that reads out text or describes the environment. These tools can significantly enhance daily life.
- Screen readers and text-to-speech software
- Smart glasses with enhanced vision capabilities
- Mobile apps designed for vision assistance
Psychological Impact and Coping Strategies
Retinopathy can have a profound psychological impact, leading to feelings of loss, anxiety, and depression. It’s critical to address these emotional aspects to maintain overall well-being.
Depression and Anxiety Management
Managing depression and anxiety requires a combination of professional help and personal strategies. This can include therapy, medication, and practices like mindfulness and meditation. These methods can help individuals cope with their emotional challenges.
Support Groups and Counseling
Support groups and counseling offer a safe space for individuals to discuss their feelings and challenges. These resources provide emotional support, practical advice, and a sense of community. They are essential for maintaining mental health and well-being.
Special Populations and Retinopathy
Special populations, like pediatric patients and pregnant women, need unique care for retinopathy. This condition shows up differently in various groups, making personalized management essential.
Pediatric Retinopathy
Pediatric retinopathy includes several retinal issues in children, often caused by prematurity, genetics, or systemic diseases. Retinopathy of prematurity (ROP) is a major concern for preterm babies, needing prompt screening and treatment to avoid vision loss. Treatment involves monitoring, laser therapy, and sometimes surgery.
Early detection through screening is key for effective treatment. Telemedicine has made it easier to screen and monitor high-risk infants.
Retinopathy in Pregnant Women
Retinopathy in pregnant women is often linked to gestational diabetes and hypertension. Hormonal shifts and increased blood volume can affect the retina. Regular eye checks are critical for pregnant women with diabetes or high blood pressure to track retinopathy.
Geriatric Considerations
The elderly face a higher risk of retinopathy, including age-related macular degeneration and diabetic retinopathy. Conditions like hypertension and heart disease can complicate treatment. Regular eye exams and detailed care plans are vital to maintain vision and quality of life.
When to Consult an Eye Specialist
Knowing when to see an eye specialist is key for those at risk of retinopathy. Early visits can greatly affect the condition’s management and outcome.
Recommended Screening Schedules
Regular eye exams are essential for catching retinopathy early. The needed frequency depends on the individual’s health condition.
For Diabetic Patients
Diabetics need a thorough eye check-up annually. Those with diabetic retinopathy might need more frequent exams.
For Hypertensive Patients
Hypertensive patients should also get regular eye tests. High blood pressure can cause hypertensive retinopathy. The exam frequency may change based on blood pressure levels.
Warning Signs That Require Immediate Attention
Certain symptoms need immediate eye specialist visits. These include:
- Sudden vision loss
- Severe eye pain
- Flashes of light or floaters
- Blurred vision

Spotting these signs early is vital to avoid severe retinopathy complications.
Advances in Retinopathy Research and Future Directions
Recent years have seen significant strides in retinopathy research, shedding light on its underlying causes and treatments. The focus has been on the complex relationship between diabetes, hypertension, and other factors that lead to retinopathy.
Advances in diagnostic imaging and genetic research have greatly enhanced our understanding of retinopathy’s progression. New treatments, such as anti-vascular endothelial growth factor (anti-VEGF) therapies and stem cell therapies, hold promise. They aim to manage the condition and prevent vision loss.
The future of retinopathy research may include personalized medicine, tailored to each patient’s needs. Ongoing clinical trials are exploring new therapeutic targets and strategies. This offers hope for better outcomes for those with retinopathy. As research advances, managing retinopathy is expected to become more effective. This will reduce the risk of vision loss and improve the quality of life for those affected.
FAQ
Q: What is retinopathy?
A: Retinopathy occurs when the retina, the light-sensitive tissue at the back of the eye, is damaged. This damage is often caused by diabetes, hypertension, or other factors.
Q: What are the symptoms of retinopathy?
A: Symptoms include blurred vision, floaters, flashes of light, and vision loss. Some people may not notice symptoms until the condition is advanced.
Q: How is retinopathy diagnosed?
A: Diagnosis involves a detailed eye examination. This includes visual acuity tests, dilated eye exams, and imaging techniques like fluorescein angiography and optical coherence tomography.
Q: What are the treatment options for retinopathy?
A: Treatment depends on the type and stage of retinopathy. Options include medical management with anti-VEGF therapy or corticosteroids, laser therapy, and sometimes surgery like vitrectomy.
Q: Can retinopathy be prevented?
A: While some risk factors are unavoidable, managing diabetes and controlling blood pressure are key. A healthy lifestyle and regular eye exams can also help prevent or slow retinopathy’s progression.
Q: What are the complications of untreated retinopathy?
A: Untreated retinopathy can cause vision loss and blindness. It can also lead to secondary conditions like macular edema and retinal detachment. These complications can significantly impact overall health.
Q: How often should diabetic patients have their eyes screened?
A: Diabetic patients should have a thorough eye examination annually. They may need more frequent exams, as advised by their eye care professional.
Q: Are there any new treatments being developed for retinopathy?
A: Yes, research is exploring new treatments. This includes emerging therapies and ongoing clinical trials, aiming to improve outcomes for retinopathy patients.















