Septoplasty: What is Septoplasty?
Nasal septum surgery, commonly known as septoplasty, is a corrective procedure aimed at fixing the displacement of the nasal septum. This displacement can cause significant breathing difficulties and other respiratory issues. Septoplasty is performed to improve airflow through the nostrils, which enhances overall respiratory function. By correcting the nasal septum’s position, individuals can experience a significant reduction in nasal congestion and related problems.
This guide will walk you through the essentials of nasal septum surgery. It includes its benefits, the procedure itself, and what to expect during recovery. Understanding septoplasty is essential for those considering this surgery to alleviate nasal obstruction symptoms.
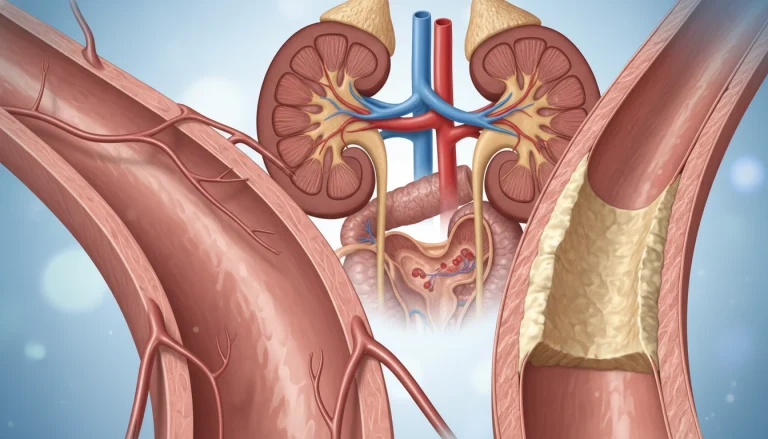
Understanding Nasal Septum Deviation and Its Impact
It’s vital to grasp the nasal septum’s role and how its deviation affects us. This thin wall of bone and cartilage divides the nasal passages. It’s key to our breathing and nasal health.
The Structure and Function of the Nasal Septum
The nasal septum is made of cartilage and bone, covered by mucous membrane. It’s designed to direct airflow through each nostril. A straight septum ensures unimpeded breathing, vital for air exchange between nostrils and lungs.
How Septal Deviation Affects Breathing and Health
A deviated nasal septum makes one passage smaller, causing breathing issues. The narrower path restricts airflow. This can also lead to nasal congestion, sinus infections, and other respiratory problems.
These breathing problems can disrupt sleep, causing sleep apnea. Deviation can also lead to facial pain, headaches, and nosebleeds. These symptoms arise from abnormal airflow and pressure in the nasal passages.
What is Septoplasty?
Septoplasty is often suggested when the nasal septum is not centered, leading to various health issues. This surgical procedure aims to correct any deviations or damages in the nasal septum. The nasal septum, composed of cartilage and bone, divides the nasal cavity into two nostrils. An off-center septum can make one nostril smaller, causing breathing problems.
Definition and Medical Purpose
Septoplasty is a corrective surgery that straightens the nasal septum, improving airflow. Its medical goals include relieving nasal obstruction symptoms, better breathing, and less nasal discharge and crusting. It’s commonly used to treat deviated septum, which can cause discomfort and health problems.
The surgery involves removing or repositioning the deviated parts of the nasal septum. Surgeons may choose between traditional open septoplasty or endoscopic septoplasty, based on the case’s complexity and the patient’s needs.
- Relieves nasal obstruction
- Improves airflow through the nostrils
- Reduces nasal discharge and crusting
History and Evolution of the Procedure
The history of septoplasty began in the early 20th century with the first surgical techniques for nasal septum corrections. Over time, the procedure has seen significant advancements, thanks to medical technology and surgical techniques.
Today, septoplasty uses endoscopic methods for less invasive procedures with faster recovery times. These advancements have made septoplasty more effective and safer, leading to better patient outcomes.
Common Causes of Deviated Septum
Several factors contribute to the development of a deviated septum, affecting breathing and overall health. A deviated septum occurs when the thin wall of cartilage and bone between the nasal passages is displaced. This makes one nasal passage smaller than the other.
Congenital Factors
Congenital factors play a significant role in the development of a deviated septum. Some people are born with a deviated septum due to genetic factors or the way the nasal septum developed in the womb. Studies have shown that a significant percentage of the population has some degree of septal deviation, often present at birth.
- Genetic predisposition
- Abnormal development in the womb
- Family history of nasal or septal issues
Traumatic Injuries
Traumatic injuries to the nose are another common cause of a deviated septum. A blow to the nose, whether from a fall, a sports injury, or an accident, can cause the nasal septum to become deviated. The impact can displace the cartilage and bone, leading to breathing difficulties and other complications.
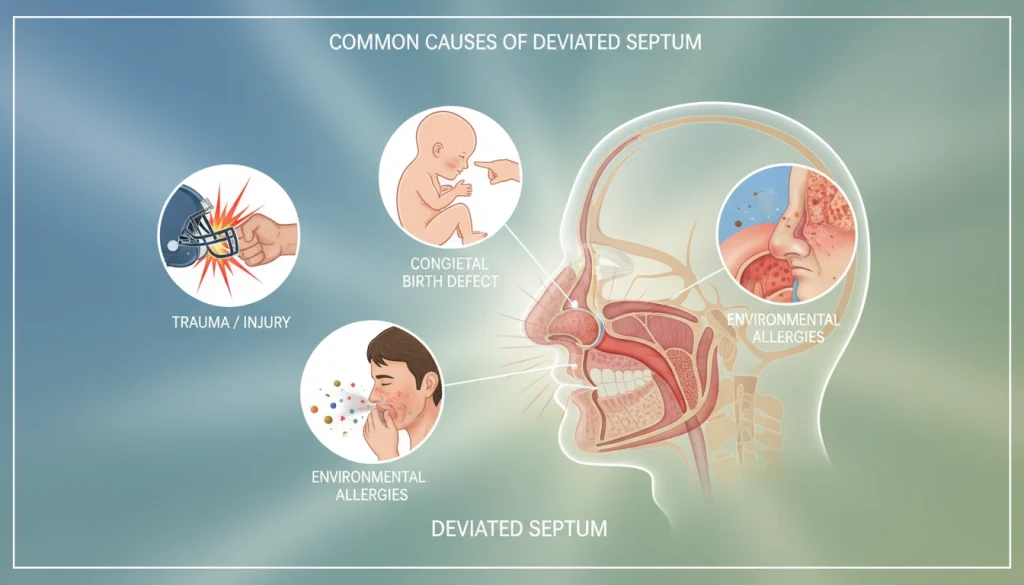
Developmental Changes
Developmental changes and growth spurts during puberty can also lead to a deviated septum. As the nasal passages and facial structures grow, the septum can become displaced. Age-related changes can also cause the nasal septum to deviate over time.
- Nasal growth during puberty
- Age-related changes
- Other developmental factors
Understanding these causes is essential for diagnosing and treating a deviated septum effectively. By identifying the underlying reason for the deviation, healthcare professionals can recommend the most appropriate treatment. This may include septoplasty.
Symptoms That May Indicate You Need Septoplasty
Identifying symptoms of a deviated septum is vital for determining if septoplasty is needed. A deviated septum can cause various symptoms that affect daily life. Understanding these symptoms helps determine if surgery is required.
Breathing Difficulties and Obstruction
Breathing troubles due to nasal blockage are a key sign that septoplasty might be necessary. A deviated septum can make one nasal passage smaller, leading to obstructed airflow. This can cause breathing through the nose to become difficult, prompting many to seek medical help.
Breathing issues can worsen with allergies, colds, or other nasal problems. If you often struggle to breathe through your nose, it could indicate a deviated septum.
Sleep-Related Issues
A deviated septum can also cause sleep problems due to nasal blockage. Snoring and sleep apnea are common complications. The blockage can cause turbulent airflow, leading to snoring. In severe cases, it can lead to sleep apnea, where breathing pauses during sleep.
Septoplasty can help address these sleep issues. It can improve sleep quality and reduce health risks.
Recurrent Sinus Infections and Other Complications
People with a deviated septum are more likely to get recurrent sinus infections. The abnormal airflow and drainage issues increase the risk of sinusitis. This condition causes facial pain, headaches, and nasal discharge.
Other complications include nasal discharge, facial pain, and postnasal drip. These symptoms can greatly impact daily life. Considering septoplasty is essential to alleviate these issues.
Diagnosis and Evaluation Process
ENT specialists use a detailed diagnostic method to decide if septoplasty is needed. This method includes physical exams, advanced tools, and functional tests. These steps help assess the nasal septum’s health and its effects on the patient’s well-being.
Physical Examination Techniques
An ENT specialist will start with a physical check of the nasal passages during the first visit. They might use anterior rhinoscopy, a tool with a light, to see the nasal cavity’s front part. They look for signs of septal deviation, nasal polyps, or other issues that could cause symptoms.
This physical exam is key to understanding the nasal septum’s state. It helps identify any breathing problems or related issues.
Nasal Endoscopy and Imaging Studies
Nasal endoscopy is used for a closer look. A flexible or rigid endoscope is inserted into the nasal passages. This lets the specialist see the nasal cavity and sinuses. CT scans or X-rays might also be used to get more information about the nasal septum and sinuses.
Nasal endoscopy and imaging studies give important details about the nasal septum’s structure. They help spot any complications or related conditions.
Functional Breathing Assessments
Functional breathing tests are also vital in the diagnosis. These might include rhinomanometry, which measures nasal airflow, or peak nasal inspiratory flow (PNIF) tests. These tests show how much septal deviation affects breathing.
By combining physical exams, nasal endoscopy, imaging, and breathing tests, ENT specialists can accurately determine if septoplasty is needed. They can then create a suitable treatment plan.
Selecting the Right Surgeon for Your Septoplasty
Choosing the right surgeon for septoplasty is critical for a successful outcome. The surgeon’s qualifications and experience can significantly impact the surgery’s success and your recovery. It’s essential to find a surgeon who can ensure a safe and effective procedure.
Qualifications to Look For
When searching for a septoplasty surgeon, look for board certification by the American Board of Otolaryngology (ABOto). This certification shows the surgeon has completed extensive training and has proven expertise in otolaryngology, including septoplasty.
Also, consider the surgeon’s experience with septoplasty. A surgeon with a high success rate in septoplasty surgeries likely has a refined technique. This could lead to better results for you.
Questions to Ask During Consultation
During your initial consultation, it’s vital to ask the right questions. This will help you assess the surgeon’s qualifications and approach. Some key questions include:
- What experience do you have with septoplasty procedures?
- Can you explain your surgical technique and the type of anesthesia used?
- What are the possible risks and complications of septoplasty?
- How will you manage pain and discomfort during recovery?
These questions offer valuable insights into the surgeon’s expertise. They help you make an informed decision.

Red Flags to Watch Out For
When evaluating surgeons, be aware of red flags. These can indicate a lack of qualifications or experience. Some red flags include:
- Lack of board certification in otolaryngology
- Unwillingness to discuss risks and complications
- Poor communication or unprofessional behavior
Being cautious of these red flags can help you avoid surgeons who may not be suitable for your septoplasty procedure.
Preparing for Septoplasty Surgery
Preparing for septoplasty surgery involves several key steps. These include pre-surgical testing, adjusting medications, and understanding what to expect on surgery day. A thorough approach is necessary for a smooth and successful procedure.
Pre-Surgical Testing and Evaluations
Your surgeon will require tests and evaluations before septoplasty. These may include a physical exam, nasal endoscopy, and imaging studies like a CT scan. These tests help your surgeon understand your nasal anatomy and any issues that might affect the surgery.
You may also need blood tests to check for bleeding disorders or other health concerns. Your surgeon will assess your breathing and nasal function to gauge the severity of your septal deviation.
Medication Adjustments and Dietary Guidelines
You may need to adjust your medications before septoplasty to reduce bleeding risks. This could mean stopping or reducing certain medications, like anticoagulants or antiplatelet agents. It’s vital to follow your surgeon’s instructions to ensure your safety during and after the surgery.
There may also be dietary guidelines to follow for optimal recovery. You might be advised to avoid certain foods or substances that could interfere with your surgery or healing. Staying hydrated and eating a balanced diet can support your health and recovery.
What to Expect on the Day of Surgery
On surgery day, you’ll arrive at the facility or hospital well before the procedure. You’ll receive specific instructions on when to arrive and what to bring. Once settled, your surgical team will prepare you, which may include administering anesthesia and other preparations.
Knowing what to expect on surgery day can help ease any anxiety. Your surgeon and team will be there to answer questions and provide support throughout the process.
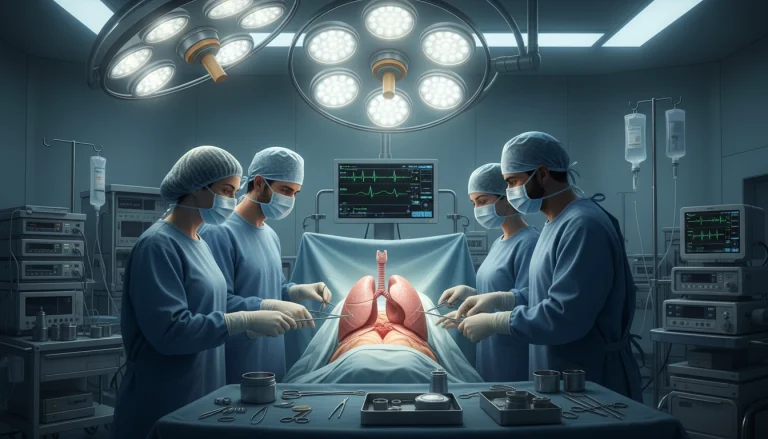
The Septoplasty Procedure: Surgical Techniques and Approaches
Septoplasty can greatly enhance nasal function by correcting a deviated nasal septum. This surgery is customized for each patient, aiming for the best results.
Anesthesia Options and Administration
Septoplasty can be done under local or general anesthesia, based on the case’s complexity and the patient’s choice. Local anesthesia numbs the area, while general anesthesia keeps the patient asleep. The decision on anesthesia is made after discussing with the patient and the anesthesiologist.
Traditional vs. Endoscopic Septoplasty
Traditional septoplasty involves an incision on one side of the nasal septum. Endoscopic septoplasty, using a small camera, offers a more precise correction with less tissue damage. This method may lead to less discomfort and a faster recovery.
Step-by-Step Surgical Process
The septoplasty procedure includes several steps. First, the surgeon may use a nasal speculum to see the nasal septum. Then, the mucosa is lifted, and the deviated parts of the septum are removed or realigned. The surgeon also addresses any other nasal obstructions.
- The surgeon may remove any bony or cartilaginous obstructions.
- The septum is then repositioned to improve airflow.
- The mucosa is re-draped over the septum.
Combining Septoplasty with Other Procedures
In some cases, septoplasty is done with other nasal surgeries, like turbinate reduction or sinus surgery. This approach can be more efficient and may shorten the recovery time.
Recovery and Healing After Septoplasty
The path to full recovery after septoplasty demands diligent post-operative care and patience. The body’s healing process is essential for achieving the desired outcomes. Knowing the recovery steps can help patients prepare and ensure a smoother healing process.
Immediate Post-Operative Care
Right after septoplasty, patients are kept under close watch in a recovery area for a few hours. Medical staff monitor for any immediate complications and manage pain. Patients are advised to rest and avoid strenuous activities. Nasal packing or splints may be used to support the septum as it heals.
Nasal saline irrigations are often recommended to keep the nasal passages clean and promote healing. It’s vital to follow the surgeon’s instructions regarding post-operative care to minimize the risk of complications.
Week-by-Week Recovery Timeline
The recovery process can be divided into several weeks, each with its milestones and expectations.
- Week 1: Rest and recovery are critical. Patients may experience swelling, bruising, and nasal congestion.
- Week 2-4: Gradually, patients can return to normal activities. Swelling subsides, and breathing improves.
- Week 4-6: Most patients can resume all normal activities, including exercise.
Pain Management and Comfort Measures
Pain management is a critical aspect of the recovery process. Surgeons often prescribe pain medication to manage discomfort. Using humidifiers and saline nasal sprays can also help alleviate dryness and discomfort.
Activity Restrictions and Return to Normal Life
Patients are advised to avoid heavy lifting, bending, and strenuous activities for several weeks after surgery. Gradually returning to normal life is key to a successful recovery. It’s also recommended to avoid blowing the nose forcefully and to be gentle when washing the face.

Potential Risks and Complications
It’s essential for patients to grasp the possible risks and complications of septoplasty before making a decision. This surgery is generally safe but, like any surgical intervention, it comes with its own set of risks and complications.
Common Side Effects and Their Management
Septoplasty can lead to nasal congestion, swelling, and bruising around the eyes and nose. These symptoms are usually temporary and can be managed with pain medication, nasal saline irrigations, and cold compresses. Rest and avoiding strenuous activities are also recommended to aid in recovery.
Another common side effect is a temporary alteration in the sense of smell. This typically resolves within a few weeks post-surgery. In some instances, patients might experience bleeding or discharge from the nose. These can be managed with nasal packing or other interventions as directed by the surgeon.
Serious Complications and Warning Signs
While rare, serious complications can arise. These include severe bleeding, infection, or a perforation of the nasal septum. It’s critical for patients to be vigilant about warning signs such as increasing pain, fever, or difficulty breathing, which may indicate a complication.
Other serious complications include a change in the shape of the nose or a septal perforation. These may require additional surgery to rectify. Adhering strictly to post-operative instructions can help minimize the risk of these complications.
When to Seek Emergency Care
Patients should seek immediate medical attention for severe symptoms such as heavy bleeding that doesn’t stop with pressure, difficulty breathing, or signs of infection like fever or increasing pain. Recognizing these warning signs early can prevent serious complications.
In summary, while septoplasty is generally a safe procedure, it’s vital to understand the possible risks and complications for a successful outcome. Being aware of common side effects, serious complications, and when to seek emergency care empowers patients to navigate their recovery with confidence.
Benefits and Expected Outcomes of Septoplasty
Septoplasty corrects nasal septum deviation, leading to better breathing, sleep, and daily activities. This surgery aims to enhance life quality for those with nasal septum deviation.
Improvement in Breathing Function
Septoplasty significantly improves nasal breathing. It corrects the deviated septum, reducing nasal congestion and obstruction. This makes breathing easier.
Improved breathing is vital for overall health. It ensures adequate oxygen intake for bodily functions. Enhanced breathing also lowers respiratory complication risks and boosts well-being.
Impact on Sleep Quality and Daily Activities
Septoplasty profoundly impacts sleep quality. It improves nasal airflow, reducing sleep disturbances like snoring and sleep apnea. This leads to more restful sleep.
Enhanced breathing and sleep quality also boost daily activities. Patients often report increased energy and the ability to engage in physical activities without fatigue or shortness of breath.
Patient Satisfaction and Success Rates
Studies indicate septoplasty has a high success rate in patient satisfaction. Most patients report significant symptom improvements and enhanced quality of life post-procedure.
The procedure’s success is due to careful patient selection, precise surgical techniques, and thorough post-operative care. While individual results vary, the overall patient satisfaction rate is high.
Cost and Insurance Considerations in the United States
Understanding the financial aspects of septoplasty is essential. It involves knowing the average costs, insurance guidelines, and financial assistance options. This knowledge is vital for those considering septoplasty to correct a deviated nasal septum.
Average Costs for Septoplasty
The cost of septoplasty varies due to several factors. These include location, surgeon expertise, and procedure complexity. On average, septoplasty in the United States costs between $3,000 and $8,000. This includes surgeon fees, anesthesia, and facility charges.
Additional costs may include pre-operative tests, post-operative care, and medications. It’s important to discuss these costs with your surgeon for a detailed estimate.
Insurance Coverage Guidelines and Requirements
Insurance coverage for septoplasty varies by provider and policy. It is typically covered if medically necessary, such as breathing difficulties or health issues.
- Verify your insurance coverage before scheduling the surgery.
- Understand the requirements for pre-authorization.
- Keep records of your correspondence with the insurance provider.
Financial Assistance Options and Payment Plans
For those without sufficient insurance or facing financial constraints, various options are available. Healthcare providers may offer financing or sliding scale fees based on income.
Navigating Insurance Pre-Authorization
The insurance pre-authorization process can be complex. It involves submitting a request to your insurance provider with necessary documentation from your healthcare provider.
- Contact your insurance provider to understand their pre-authorization requirements.
- Work with your surgeon’s office to prepare the necessary documentation.
- Follow up with the insurance company to ensure timely processing of your request.
Living with a Corrected Nasal Septum: Long-Term Care and Considerations
After septoplasty, patients often see a marked improvement in their quality of life. The correction of the nasal septum deviation is a significant factor. It’s vital to maintain the surgery’s benefits through proper long-term care. This ensures the nasal passages stay healthy.
Understanding that nasal septum correction is just the beginning is essential. Patients must be aware of the possibility of future nasal problems. Preventive measures are key. Regular nasal hygiene, like saline irrigations, helps keep the passages clean and lowers complication risks.
Those who have had septoplasty should be cautious of their surroundings. Avoiding irritants like tobacco smoke and strong smells is critical to prevent nasal inflammation. Using humidifiers during dry weather can also aid in maintaining nasal health.
Regular visits to an ear, nose, and throat (ENT) specialist are necessary. They help monitor the healing process and address any issues quickly. Following these long-term care guidelines ensures patients can fully benefit from their septoplasty. It helps maintain optimal nasal health.
FAQ
Q: What is septoplasty?
A: Septoplasty is a surgical procedure aimed at correcting a deviated nasal septum. This is the cartilage and bone dividing the nasal cavity into two nostrils. The surgery aims to improve breathing, reduce nasal congestion, and alleviate related issues.
Q: How long does it take to recover from septoplasty?
A: Recovery from septoplasty varies, but most return to normal activities in one to two weeks. Swelling and bruising usually subside within a few days to a week. Full recovery can take several weeks to a few months.
Q: Will septoplasty change the appearance of my nose?
A: Septoplasty is mainly for correcting functional issues, not for changing the nose’s appearance. Yet, it might be combined with rhinoplasty, a cosmetic procedure, in some cases.
Q: Is septoplasty covered by insurance?
A: Septoplasty is often covered by insurance if it’s medically necessary. This includes correcting a deviated septum causing breathing difficulties or chronic sinus infections. Coverage varies by provider and policy.
Q: What are the possible risks and complications of septoplasty?
A: Septoplasty carries risks like bleeding, infection, and adverse reactions to anesthesia. Possible complications include nasal septal perforation, persistent nasal obstruction, and changes in the sense of smell.
Q: Can septoplasty be performed on children?
A: Yes, septoplasty can be performed on children. The decision is made on a case-by-case basis, considering the child’s age, health, and the severity of their nasal septum deviation.
Q: How is septoplasty performed?
A: Septoplasty is performed under general anesthesia or local anesthesia with sedation. The surgeon makes an incision on one side of the nasal septum, removes or repositions the deviated parts, and then closes the incision. It can be done using traditional or endoscopic techniques.
Q: What can I expect during the recovery period after septoplasty?
A: Expect nasal congestion, swelling, and bruising during recovery. Your doctor may prescribe pain medication and recommend nasal saline irrigations. It’s critical to follow post-operative instructions carefully for a smooth recovery.