Understanding the Thymus Gland and Its Function
Thymic malignancies are rare tumors that start in the thymus, a key organ for the immune system’s development. It’s vital to grasp the complexities of these cancers for patients and their families. Diagnosing and treating thymus gland cancer demands a detailed approach, involving several medical fields. This guide delves into the condition, discussing diagnosis, treatment choices, and support for those impacted.
This article seeks to enlighten readers on the management strategies for thymic malignancies. It highlights the critical role of a multidisciplinary care team. Grasping the thymus gland’s role is key to understanding our immune system’s development and response to threats. This gland is vital, mainly in childhood and adolescence, for the immune system’s function.
Anatomy and Location of the Thymus Gland
The thymus gland sits behind the sternum, in the chest’s anterior part, and is most active in youth. Its location is strategic, enabling it to play a critical role in early life. It facilitates the maturation of T-lymphocytes.
Role in Immune System Development
The thymus gland matures T-lymphocytes, a vital white blood cell for cell-mediated immunity. It selects and matures T-cells, which then fight infections throughout the body.
- T-lymphocyte maturation
- Cell-mediated immunity
- Immune system development
Natural Involution Process with Age
With age, the thymus gland naturally shrinks and becomes less active. This decline in function is a normal aging process. Yet, it affects the immune system’s effectiveness in older age.
In summary, the thymus gland is essential for the immune system’s development, mainly in early life. Its function and changes over time are vital for understanding Thymus Gland Cancer.
Thymus Gland Cancer: Types and Classifications
Thymic malignancies encompass a wide range of cancers originating in the thymus gland. Accurate diagnosis and classification are essential. The complexity of these cancers demands a deep understanding of their various types and characteristics.
Definition and Overview
Thymus gland cancer involves malignancies that develop from the thymus’s epithelial cells or other components. These cancers exhibit a wide range of behaviors, from slow-growing tumors to aggressive malignancies.
Types of Thymic Malignancies
The main categories of thymic malignancies include thymoma, thymic carcinoma, and thymic neuroendocrine tumors. Each category has unique pathological features and implications for prognosis.
Thymoma
Thymomas originate from the thymus’s epithelial cells. They are often linked to autoimmune conditions, such as myasthenia gravis.
Thymic Carcinoma
Thymic carcinomas are more aggressive than thymomas, with a higher metastasis rate. They are distinguished by their invasive growth and cytological atypia.
Thymic Neuroendocrine Tumors
These rare tumors stem from the thymus’s neuroendocrine cells. They can vary from low-grade to high-grade malignancies, with different prognostic outcomes.
Prevalence and Epidemiology
Thymus gland cancer is relatively rare, making up a small fraction of mediastinal tumors. Its prevalence differs across various populations, with certain types more prevalent in specific age groups or genders.
- Thymoma is the most common type of thymic malignancy.
- Thymic carcinoma is less common but more aggressive.
- Thymic neuroendocrine tumors are rare and often have a poor prognosis.
Grasping the epidemiology and types of thymic malignancies is vital for early detection and effective management of these complex cancers.
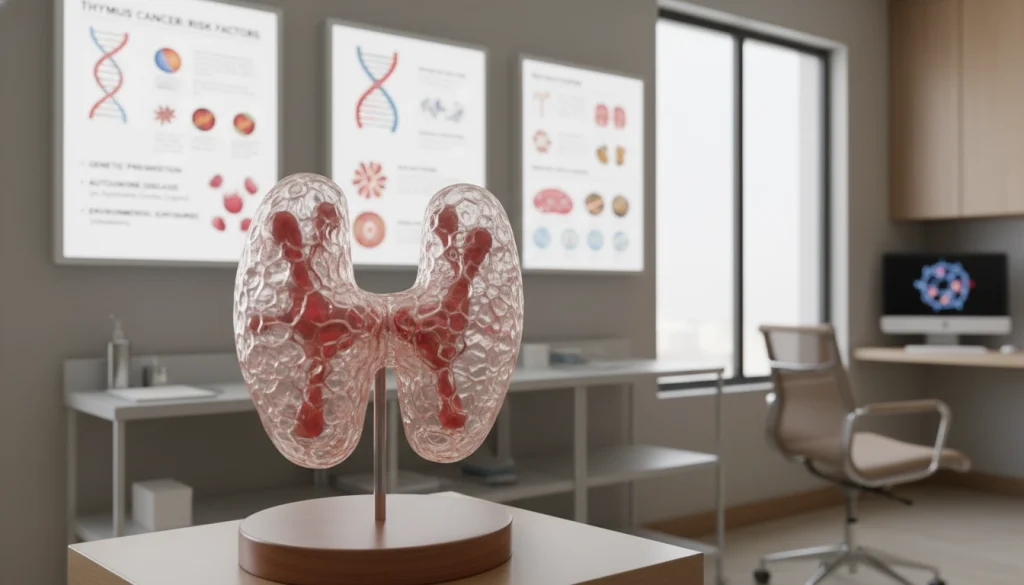
Risk Factors and Causes
The onset of Thymus Gland Cancer is shaped by genetic, environmental, and medical elements. Grasping these risk factors is key to spotting those at higher risk. It also aids in crafting early detection and prevention plans.
Genetic Predispositions
Genetic predispositions significantly influence Thymus Gland Cancer development. Syndromes like Multiple Endocrine Neoplasia Type 1 (MEN1) raise thymic tumor risk. Studies indicate genetic mutations can lead to thymic cell malignancy.
Environmental Factors
Environmental exposures are linked to Thymus Gland Cancer. The precise mechanisms are unclear, but certain chemicals and radiation may heighten risk. Further research is essential to understand environmental impacts on thymic cancer.
Associated Medical Conditions
Certain medical conditions elevate Thymus Gland Cancer risk. Myasthenia Gravis, an autoimmune disease, often co-occurs with thymoma. Other conditions, like hypogammaglobulinemia and red cell aplasia, are also associated with thymic malignancies.
Identifying these risk factors and associated conditions is vital for early diagnosis and management of Thymus Gland Cancer. Continued research is needed to fully grasp the complex interplay between genetics, environment, and medicine in this disease.
Signs and Symptoms
Thymus gland cancer presents in various ways, including symptoms and paraneoplastic syndromes. These signs can greatly affect diagnosis and treatment.
Common Presenting Symptoms
Patients often show symptoms related to the tumor’s chest location. These include chest pain, cough, and shortness of breath. The tumor can also compress or invade nearby structures, causing superior vena cava syndrome or dysphagia.
Paraneoplastic Syndromes
Thymus gland cancer is linked to several paraneoplastic syndromes. These are conditions caused by the immune system reacting to the tumor. They can greatly impact a patient’s quality of life and may be the first sign of the disease.
Myasthenia Gravis
Myasthenia gravis is a neuromuscular disorder causing muscle weakness and fatigue. It’s a common paraneoplastic syndrome linked to thymus gland cancer.
Pure Red Cell Aplasia
Pure red cell aplasia severely impairs red blood cell production. This leads to severe anemia and requires immediate treatment.
Hypogammaglobulinemia
Hypogammaglobulinemia is a deficiency in antibody production. It makes patients more prone to infections. Managing this condition often involves immunoglobulin replacement therapy.
When to Seek Medical Attention
It’s vital for those with persistent or severe symptoms to see a doctor. Early diagnosis and treatment can greatly improve outcomes for thymus gland cancer patients.
Diagnostic Procedures
The diagnostic process for thymic cancer is thorough, involving several key steps. These steps help determine the presence and extent of the disease. Accurate diagnosis is essential for creating an effective treatment plan.
Physical Examination and Medical History
A detailed physical examination and medical history are the first steps in diagnosing thymus gland cancer. Healthcare providers search for signs and symptoms that may indicate thymic malignancy. These include chest pain, cough, or difficulty breathing.
Imaging Studies
Imaging studies are vital in diagnosing and staging thymus gland cancer. They include:
-
CT Scan
A CT scan provides detailed cross-sectional images of the chest. It helps identify tumors in the thymus gland.
-
MRI
MRI offers high-resolution images. It can differentiate between various types of thymic tumors and assess their extent.
-
PET Scan
PET scans assess the metabolic activity of tumors. They detect any spread to other parts of the body.
Biopsy Techniques
A biopsy is essential for confirming thymus gland cancer diagnosis. Various biopsy techniques, including needle biopsy and surgical biopsy, are used. They obtain tissue samples for pathological examination.
Laboratory Tests
Laboratory tests, including blood tests and histopathological examination of biopsy samples, are critical. They diagnose thymic malignancies and determine their specific type and characteristics.
Staging and Classification Systems
Accurate staging is key for predicting prognosis and treatment in Thymus Gland Cancer patients. Staging systems help doctors gauge the disease’s extent and its likely impact on patient outcomes.
Several staging and classification systems are employed in Thymus Gland Cancer. Each offers valuable insights into the disease’s nature.
Masaoka-Koga Staging System
The Masaoka-Koga staging system is a leading classification for Thymus Gland Cancer. It categorizes tumors by the extent of invasion and spread.
- Masaoka-Koga Stage I: Encapsulated tumor with no invasion
- Masaoka-Koga Stage II: Tumor with invasion into surrounding tissues
- Masaoka-Koga Stage III: Tumor with invasion into neighboring organs
- Masaoka-Koga Stage IV: Tumor with distant metastasis
TNM Classification
The TNM classification system, developed by the American Joint Committee on Cancer (AJCC), is another widely used staging system. It categorizes tumors based on the size and extent of the primary tumor (T), lymph node involvement (N), and distant metastasis (M).
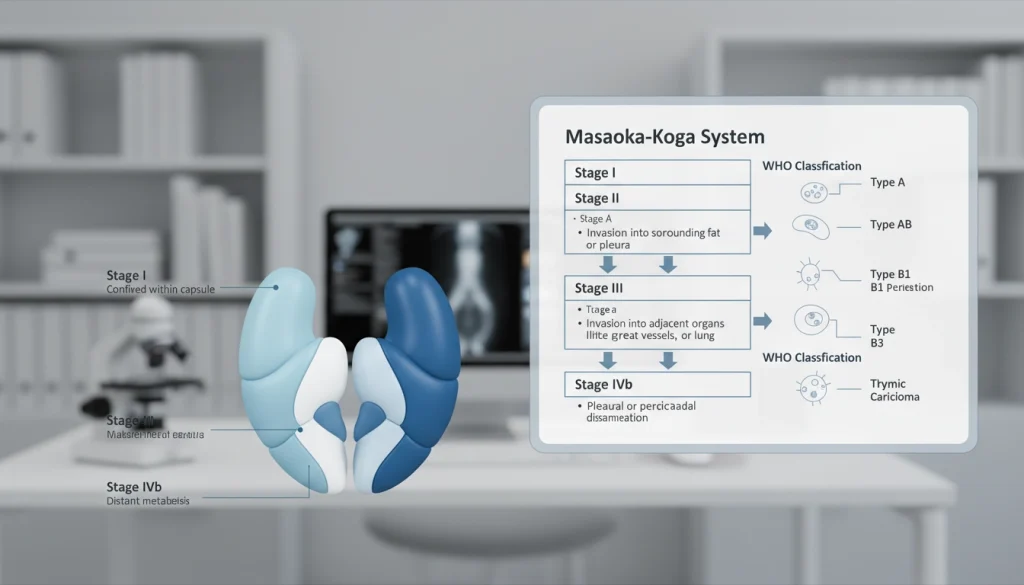
WHO Histological Classification
The World Health Organization (WHO) histological classification system categorizes Thymus Gland Cancer based on its histological characteristics. This system aids clinicians in understanding the tumor’s behavior and its likely response to treatment.
Prognostic Implications of Staging
The staging and classification systems used in Thymus Gland Cancer offer critical prognostic insights. Patients with early-stage disease generally have better outcomes than those with advanced disease. Grasping the staging and classification of Thymus Gland Cancer is vital for crafting effective treatment plans and improving patient outcomes. For more information on cancer treatment and management, visit Acibadem International.
Treatment Options
Treatment for thymus gland cancer involves a multifaceted approach. It combines various modalities to achieve optimal outcomes. The choice of treatment depends on several factors. These include the stage of cancer, histological type, and the patient’s overall health.
Surgical Approaches
Surgery plays a critical role in treating thymic malignancies. The primary goal is to remove the tumor completely. This includes any affected surrounding tissues.
Complete Resection
Complete resection is considered the gold standard for early-stage thymic tumors. It involves removing the entire tumor. This is done along with a margin of healthy tissue around it.
Minimally Invasive Techniques
Minimally invasive surgical techniques, such as video-assisted thoracoscopic surgery (VATS) and robotic-assisted surgery, are gaining popularity. These approaches offer smaller incisions. They also reduce postoperative pain and quicken recovery times.
Radiation Therapy
Radiation therapy is often used in conjunction with surgery or as a standalone treatment for thymic cancer. It helps control local disease. It also alleviates symptoms.
Chemotherapy Protocols
Chemotherapy is typically used for advanced or metastatic thymic cancer. Various chemotherapy regimens have been developed. These often combine multiple drugs to target cancer cells effectively.
Targeted Therapies
Targeted therapies are designed to target specific molecular abnormalities in cancer cells. These treatments are being explored for thymic malignancies. They offer potentially more effective and less toxic options.
Immunotherapy Developments
Immunotherapy, which harnesses the body’s immune system to fight cancer, is an area of active research in thymic malignancies. Various immunotherapeutic approaches are being investigated. These include checkpoint inhibitors and other novel strategies.
The treatment of thymus gland cancer requires a multidisciplinary approach. It involves surgeons, medical oncologists, radiation oncologists, and other specialists. By combining these various treatment modalities, healthcare providers can offer personalized care plans. These plans are tailored to each patient’s unique needs and condition.
Specialized Treatment Centers and Expert Consultation
Dealing with thymus gland cancer treatment is complex. This makes seeking expert advice at specialized centers vital. Patients gain a lot from the care teams and advanced treatments at these places.
Finding Thymic Cancer Specialists
Finding the right specialist is key in thymus gland cancer treatment. Look for oncologists and surgeons with a focus on thymic cancers. Professional groups and cancer support can offer great advice.
Comprehensive Cancer Centers
Comprehensive cancer centers provide a wide range of services. They have top-notch diagnostic tools, care teams, and access to clinical trials. These centers are ready to tackle thymus gland cancer’s complexities.
Second Opinion Considerations
Getting a second opinion is common in cancer care. It helps confirm diagnoses and explore other treatment paths. Many specialized centers offer second opinions, giving a detailed review of your case.
International Treatment Options
Some patients might consider international treatment options. Certain countries have centers skilled in rare cancers like thymus gland cancer. But, it’s important to research the qualifications and experience of international providers.
Managing Associated Autoimmune Conditions
Dealing with thymus gland cancer requires more than just treating the cancer. It also means managing autoimmune conditions like Myasthenia Gravis and paraneoplastic syndromes. These conditions can greatly affect a patient’s life quality and treatment success.
Treatment of Myasthenia Gravis
Myasthenia Gravis often comes with thymus gland cancer. Treatment usually involves a mix of medications to control symptoms. Sometimes, removing the thymus gland surgically is also considered.
- Medications such as anticholinesterases and immunosuppressants are commonly used.
- Thymectomy (surgical removal of the thymus gland) may be recommended for some patients.
- Plasmapheresis and intravenous immunoglobulin may be used in severe cases.
Addressing Other Paraneoplastic Syndromes
Other paraneoplastic syndromes, such as pure red cell aplasia and hypogammaglobulinemia, can also occur. Managing these conditions requires a detailed approach, including:
- Identifying and treating the underlying cause.
- Managing symptoms with appropriate medications.
- Monitoring for complications and adjusting treatment as necessary.
Integrated Care Approaches
An integrated care approach is key for managing thymus gland cancer and related autoimmune conditions. It involves teamwork between oncologists, neurologists, and other specialists. This ensures a holistic care plan.
Through integrated care, healthcare providers can enhance patient outcomes and improve their quality of life.
Prognosis and Survival Rates
The prognosis for thymus gland cancer varies based on several key factors. It’s vital for patients and their families to grasp these factors. They influence survival rates and help navigate the challenges ahead.
Factors Affecting Prognosis
Several factors are critical in determining thymus gland cancer prognosis. These include the stage at diagnosis, the tumor’s histological type, and the patient’s overall health. The Masaoka-Koga staging system is commonly used to predict outcomes.
- Stage at Diagnosis: Early-stage thymus gland cancer generally has a better prognosis than advanced stages.
- Histological Type: The type of thymic malignancy, such as thymoma or thymic carcinoma, affects treatment outcomes.
- Patient’s Health: Pre-existing health conditions can influence a patient’s ability to undergo certain treatments.
Survival Statistics by Stage and Type
Survival statistics for thymus gland cancer are categorized by stage and histological type. Patients with early-stage disease generally have higher survival rates. For example, the five-year survival rate for localized thymic tumors is significantly higher than for those with distant metastasis.
Quality of Life Considerations
Quality of life is a critical aspect of managing thymus gland cancer. Treatment plans aim to improve survival rates and maintain quality of life. This includes managing symptoms, minimizing treatment side effects, and providing supportive care.
Long-term Outlook
The long-term outlook for patients with thymus gland cancer depends on various factors. These include response to treatment and the presence of any associated autoimmune conditions. Regular follow-up care is essential to monitor for recurrence and manage any long-term effects of treatment.
Understanding the factors that influence prognosis and survival rates helps patients navigate their treatment journey. It enables them to make informed decisions about their care.
Recovery and Follow-up After Treatment
The journey doesn’t end with treatment; Thymus Gland Cancer patients must navigate a detailed recovery and follow-up plan. This phase is critical for detecting any issues early and improving outcomes.
Post-surgical Rehabilitation
Post-surgical rehabilitation is key in the recovery process. It helps patients regain strength and manage post-operative complications. A structured rehabilitation program includes physical therapy, nutritional counseling, and psychological support.
- Physical therapy to regain strength and mobility
- Nutritional counseling to optimize diet and recovery
- Psychological support to cope with the emotional aspects of cancer treatment
Surveillance Protocols
Surveillance protocols are vital for monitoring the patient’s condition and detecting recurrence early. These protocols involve regular imaging studies, laboratory tests, and follow-up appointments with healthcare providers.
- Regular CT scans or MRI to monitor for recurrence
- Laboratory tests to check for tumor markers or other signs of cancer
- Follow-up appointments with oncologists and surgeons
Managing Long-term Side Effects
Managing long-term side effects is a critical aspect of post-treatment care. Patients may face fatigue, pain, and emotional and cognitive challenges. Effective management strategies can significantly improve quality of life.
- Medications to manage pain and other symptoms
- Lifestyle modifications to reduce fatigue and improve overall well-being
- Support groups and counseling to address emotional and psychological needs
Recurrence Monitoring
Monitoring for recurrence is an ongoing process that requires vigilance and a proactive approach. Patients should be aware of recurrence signs and symptoms. They should report any concerns to their healthcare team promptly.
Research and Clinical Trials
Research and clinical trials are driving progress in thymus gland cancer treatment. These efforts are vital for finding new treatments and improving existing ones. They help identify effective strategies against this disease.
Current Research Directions
Research is concentrated on several fronts. It includes studying thymic tumors at a molecular level, exploring immunotherapy, and developing targeted treatments. Scientists are also delving into the genetic causes of thymus gland cancer. This knowledge is key to understanding the disease’s development and progression.
Promising Experimental Therapies
Several experimental therapies hold promise for thymus gland cancer treatment. These include:
- Immunotherapies, like checkpoint inhibitors, which boost the immune system’s fight against cancer.
- Targeted therapies that target specific genetic changes in thymic tumors.
- Advanced chemotherapy regimens and combination treatments aimed at better outcomes and survival rates.

How to Find and Participate in Clinical Trials
Patients looking to join clinical trials can explore various resources. These include:
- ClinicalTrials.gov, a vast database of global clinical trials.
- Cancer centers and research institutions focused on thymus gland cancer.
- Patient advocacy groups that offer support and information for trial participation.
Future Treatment Perspectives
The future of thymus gland cancer treatment looks promising. Ongoing and future clinical trials will shape this progress. As research evolves, patients can expect more targeted and effective treatments. This could significantly enhance their quality of life and treatment outcomes.
Moving Forward: Resources and Support for Patients and Families
Patients and families dealing with Thymus Gland Cancer can find significant help from various resources and support services. Overcoming the hurdles of thymic malignancies requires access to dependable information and support networks. This is essential for navigating the challenges they face.
Several organizations provide support groups, educational materials, and online forums. These allow patients to connect with others facing similar challenges. Such resources are vital for emotional support, practical advice, and a sense of community.
Information sources like the National Cancer Institute and the Thymic Cancer Association offer the latest on treatment options, clinical trials, and research. Using these resources empowers patients and families to make informed decisions about their care. This knowledge is key to their well-being.
By tapping into these resources and support services, patients and families can better manage the complexities of Thymus Gland Cancer. This helps them on their journey towards recovery and beyond.
FAQ
Q: What is Thymus Gland Cancer?
A: Thymus Gland Cancer, also known as thymic malignancy, is a rare cancer type. It starts in the thymus gland, located behind the sternum. This gland is vital for the immune system’s development.
Q: What are the different types of Thymus Gland Cancer?
A: Thymus Gland Cancer includes thymoma, thymic carcinoma, and thymic neuroendocrine tumors. Each type has unique characteristics and implications for prognosis.
Q: What are the symptoms of Thymus Gland Cancer?
A: Symptoms include chest pain, cough, and difficulty swallowing. Shortness of breath is also common. Paraneoplastic syndromes like myasthenia gravis and hypogammaglobulinemia can occur.
Q: How is Thymus Gland Cancer diagnosed?
A: Diagnosis involves physical exams, medical history, and imaging studies. CT, MRI, and PET scans are used. Biopsy and lab tests help confirm the presence and extent of the cancer.
Q: What are the treatment options for Thymus Gland Cancer?
A: Treatments include surgery, radiation, and chemotherapy. Targeted and immunotherapy are also options. A team approach is often necessary for effective care.
Q: What is the prognosis for Thymus Gland Cancer?
A: Prognosis varies based on stage, histology, and patient characteristics. Survival rates differ by cancer stage and type.
Q: Are there any clinical trials for Thymus Gland Cancer?
A: Yes, clinical trials are ongoing. They explore new treatments and therapies, including experimental and immunotherapy options.
Q: Where can I find support and resources for Thymus Gland Cancer?
A: Support and resources are available. This includes support groups, cancer centers, and online information. These help navigate thymic malignancies.
Q: How can I find a specialist for Thymus Gland Cancer?
A: Finding specialists is possible. Start with your primary care physician or search online. Contact cancer centers for multidisciplinary care options.