Thyroid Cancer: What is Thyroid Cancer
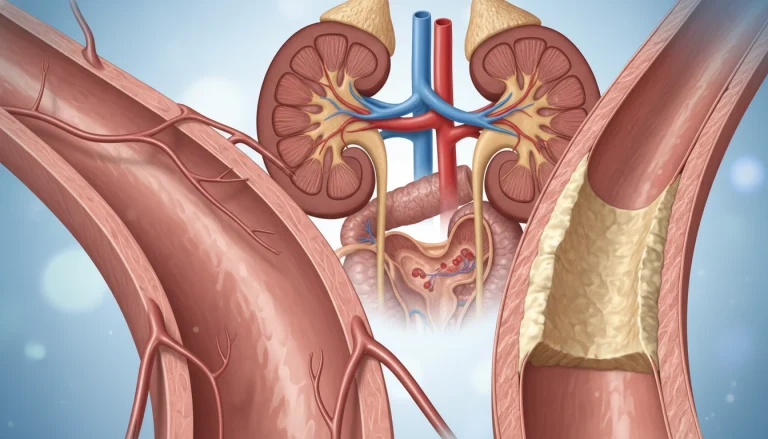
Thyroid cancer is a serious health condition that affects the thyroid gland, a vital part of the endocrine system. Diagnosing this condition involves a series of tests to determine the presence and extent of the disease. Effective treatment options are available, ranging from surgery to radioactive iodine therapy. Understanding these options and the recovery process is essential for patients and their families.
This guide offers a detailed look at thyroid cancer. It covers diagnosis, treatment, and what to expect during recovery. Our goal is to inform and support those affected by this condition. Thyroid cancer starts with understanding the thyroid gland’s role in our body. This butterfly-shaped organ is in the neck, around the trachea. It controls metabolism, growth, and development by making thyroid hormones.
The Thyroid Gland: Structure and Function
The thyroid gland has two lobes joined by an isthmus. It makes thyroxine (T4) and triiodothyronine (T3). These hormones are key for metabolic rate, nerve function, and muscle strength. The gland’s health is essential for our well-being.
Definition and Significance of Thyroid Cancer
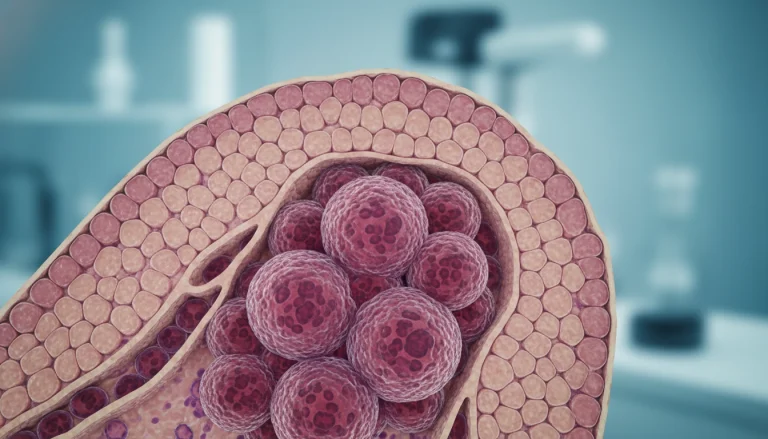
Thyroid cancer happens when thyroid cells grow abnormally, forming a malignant tumor. It’s a serious health issue because it can affect thyroid function and overall health. There are different types of thyroid cancer, based on cell type and aggressiveness.
Prevalence and Demographics
Thyroid cancer is rare but its incidence is rising. It’s more common in women and affects people aged 25 to 65. Knowing who is at risk helps in early detection and treatment.
Being aware of thyroid cancer’s prevalence and demographics is key. Early detection greatly improves treatment outcomes for those affected.
Types of Thyroid Cancer
Thyroid cancer encompasses a spectrum of malignancies originating from the thyroid gland. Each type has distinct characteristics and implications for treatment and management. Understanding these differences is essential for effective diagnosis and care.
Papillary Thyroid Cancer
Papillary thyroid cancer is the most prevalent form, making up 80-85% of cases. It is named for its distinctive appearance under the microscope.
Characteristics and Variants
This cancer can manifest in several forms, including classical, follicular, and tall cell variants. These variations can affect prognosis and treatment strategies.
Typical Progression
Papillary thyroid cancer grows slowly and may spread to neck lymph nodes. Early detection significantly improves prognosis. It typically progresses through local invasion and lymph node metastasis.
Follicular Thyroid Cancer
Follicular thyroid cancer is the second most common, accounting for 10-15% of cases. It originates from the thyroid’s follicular cells.
Distinguishing Features
This cancer is identified by its follicular structure and absence of papillary thyroid cancer’s nuclear features. It tends to metastasize through the bloodstream more than lymph nodes.
Hurthle Cell Carcinoma
Hurthle cell carcinoma is a follicular cancer variant, recognized by the presence of Hurthle cells. Its unique characteristics set it apart from other thyroid cancers.
Medullary Thyroid Cancer
Medullary thyroid cancer arises from the parafollicular cells (C cells) of the thyroid gland. It represents 3-5% of cases and can be sporadic or familial.
Genetic mutations, such as in the RET gene, are common in medullary thyroid cancer. It produces calcitonin, a key tumor marker for diagnosis and monitoring.
Anaplastic Thyroid Cancer
Anaplastic thyroid cancer is a rare and aggressive form, making up 1-2% of cases. It grows rapidly and is often diagnosed at an advanced stage.
This cancer is challenging to treat due to its aggressive nature and resistance to conventional therapies. It predominantly affects older adults, with a poor prognosis.
Risk Factors for Thyroid Cancer
Understanding the risk factors for thyroid cancer is key to early detection and prevention. Several factors can raise an individual’s risk of developing thyroid cancer. Knowing these can help in taking preventive steps.
Genetic and Hereditary Factors
Genetic and hereditary factors significantly influence thyroid cancer development. Certain genetic syndromes and family history can increase risk.
Family History and Genetic Syndromes
A family history of thyroid cancer, often medullary thyroid cancer, significantly raises risk. Genetic syndromes like Multiple Endocrine Neoplasia type 2 (MEN2) also elevate thyroid cancer risk.
- Familial Medullary Thyroid Cancer (FMTC)
- Multiple Endocrine Neoplasia type 2 (MEN2)
- Familial Adenomatous Polyposis (FAP)
Genetic Testing Considerations
For those with a family history of thyroid cancer or related genetic syndromes, genetic testing is advised. It can identify mutations that heighten thyroid cancer risk.
Radiation Exposure
Childhood radiation exposure is a known risk factor for thyroid cancer. This includes radiation therapy to the head and neck area.
Other Contributing Factors
Dietary factors, such as iodine deficiency or excess, and environmental exposures also contribute to thyroid cancer risk.
- Iodine deficiency or excess
- Exposure to certain chemicals
- Hormonal influences
Signs and Symptoms of Thyroid Cancer
Understanding the signs and symptoms of thyroid cancer is key for early detection and effective treatment. Thyroid cancer can show itself in various ways, categorized into early warning signs and advanced symptoms.
Early Warning Signs
Early signs of thyroid cancer include a lump or swelling in the neck, often painless. Other signs are hoarseness or voice changes, difficulty swallowing, or breathing issues. These symptoms can be subtle and may not immediately suggest thyroid cancer. Yet, they require a medical check-up.
Advanced Symptoms
As thyroid cancer advances, more severe symptoms appear. These include enlarged lymph nodes in the neck, a persistent cough not caused by a cold, and neck or throat pain that may spread to the ears. These symptoms indicate a more serious stage of the disease, needing immediate medical care.
It’s vital to recognize these signs and symptoms for timely diagnosis and treatment. If you or someone you know is experiencing any of these symptoms, seeking a healthcare professional’s advice is essential.
Diagnosing Thyroid Cancer
The process of diagnosing thyroid cancer involves several steps. It begins with physical examinations and progresses to more detailed tests.
Physical Examination Techniques
A thorough physical examination is key in the early detection of thyroid cancer. Healthcare providers look for signs such as thyroid nodules, gland enlargement, or neck lymph node swelling.
During the examination, the healthcare provider may use palpation. This method assesses the size, consistency, and tenderness of the thyroid gland and any nodules present.
Blood Tests and Thyroid Function Assessment
Blood tests are used to assess thyroid function and detect abnormalities. Key tests include measurements of thyroid-stimulating hormone (TSH), free thyroxine (FT4), and free triiodothyronine (FT3) levels.
While blood tests cannot definitively diagnose thyroid cancer, they help evaluate thyroid function. They identify issues that may require further investigation.
Imaging Studies
Imaging studies are vital in diagnosing thyroid cancer. They provide detailed images of the thyroid gland and surrounding structures.
Ultrasound
Ultrasound is often the first imaging modality used to evaluate thyroid nodules. It assesses the size, number, and characteristics of nodules, guiding further management decisions.
CT, MRI, and PET Scans
Computed Tomography (CT), Magnetic Resonance Imaging (MRI), and Positron Emission Tomography (PET) scans are used to assess disease extent. They are used when cancer spread is suspected.
Radioiodine Scans
Radioiodine scans detect thyroid tissue and cancer cells that absorb iodine. They help in diagnosing and staging thyroid cancer.
Biopsy Procedures
Biopsy procedures are essential for definitively diagnosing thyroid cancer. Fine-needle aspiration biopsy (FNAB) is commonly used to sample cells from thyroid nodules.
The sampled cells are then examined cytologically. This determines the presence of cancer cells, guiding treatment decisions.
Diagnosing thyroid cancer requires a holistic approach. It integrates findings from physical examination, laboratory tests, imaging studies, and biopsy procedures.
- Physical examination techniques help identify thyroid abnormalities.
- Blood tests assess thyroid function.
- Imaging studies provide detailed images of the thyroid gland.
- Biopsy procedures confirm the presence of cancer cells.
Thyroid Cancer Staging and Classification
Grasping the stage of thyroid cancer is essential for predicting outcomes and selecting the best treatment. The staging process examines the tumor’s size, lymph node involvement, and distant metastasis presence.
TNM Classification System
The TNM classification system is a common method for staging thyroid cancer. It assesses three critical aspects: the primary Tumor’s size and extent (T), lymph Node involvement (N), and distant Metastasis (M). Each factor receives a score based on the cancer’s specifics.
The tumor’s (T) classification depends on its size and invasion of surrounding tissues. Lymph node (N) involvement is evaluated by the presence and location of cancerous nodes. Distant metastasis (M) assesses whether the cancer has spread to other body parts.
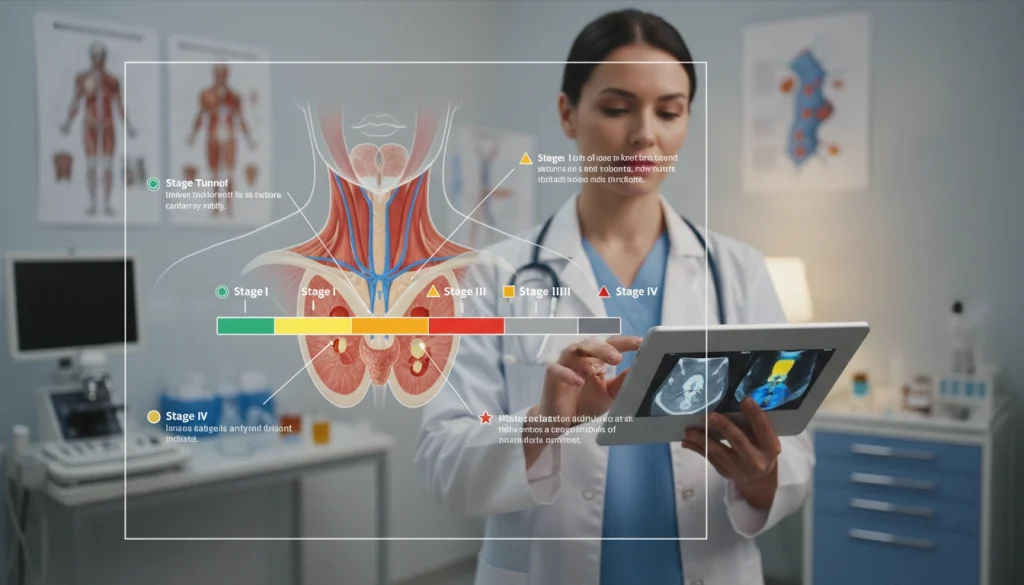
Stage Grouping and Prognostic Implications
Using the T, N, and M scores, an overall stage is assigned to the thyroid cancer, typically from Stage I to Stage IV. This stage grouping aids clinicians in predicting patient outcomes and planning treatments.
Stages I and II generally indicate a better prognosis, with higher survival rates and possibly less aggressive treatments needed. In contrast, stages III and IV signify more severe disease, requiring more intensive treatments like surgery, radioactive iodine therapy, and external beam radiation therapy.
Understanding thyroid cancer’s stage and classification is critical for both healthcare professionals and patients. It influences treatment choices and offers insights into the likely prognosis.
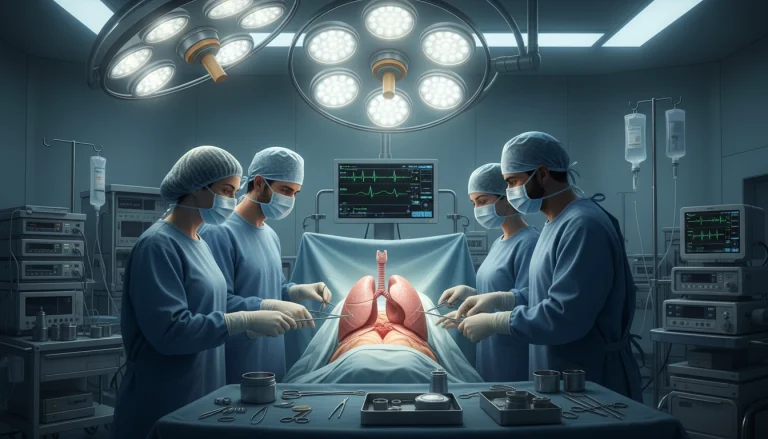
Surgical Management of Thyroid Cancer
The surgical management of thyroid cancer includes various procedures. These include thyroid lobectomy and total thyroidectomy, each suited for different scenarios. The choice of surgery depends on the cancer’s type and stage, along with the patient’s health.
Thyroid Lobectomy: Procedure and Indications
Thyroid lobectomy removes one lobe of the thyroid gland. It’s often advised for those with small, low-risk papillary thyroid cancers. It’s also considered for thyroid nodules that might be cancerous but haven’t been confirmed.
Total Thyroidectomy: Technique and Considerations
Total thyroidectomy removes the entire thyroid gland. It’s recommended for larger tumors, multifocal disease, or high-risk features. The surgery requires careful planning due to the patient’s anatomy and the risk of complications.
Lymph Node Dissection Approaches
Lymph node dissection is often done with thyroidectomy, when lymph nodes are involved. The extent of dissection can vary. It can range from a limited sampling to a full dissection of neck compartments.
Recovery and Postoperative Care
Postoperative care is vital for a smooth recovery after thyroid surgery.
Hospital Stay and Immediate Recovery
Most patients are discharged on the same day or the next. Immediate care includes watching for bleeding or airway issues. It also involves managing pain effectively.
Long-term Surgical Recovery
Long-term recovery involves managing thyroid hormone replacement and follow-up. Patients are also advised on managing long-term complications like hypocalcemia or vocal cord issues.
Radioactive Iodine (RAI) Therapy
Radioactive Iodine (RAI) therapy is a key treatment for thyroid cancer. It uses the thyroid gland’s natural iodine affinity. This method targets and destroys thyroid cancer cells, both those left after surgery and those that have spread.
Mechanism of Action
RAI therapy works by exploiting the thyroid gland’s iodine absorption. Administered radioactive iodine is absorbed by thyroid tissue, including cancer cells. The radioactive part then emits radiation, damaging the DNA of cancer cells and leading to their destruction.
Preparation Protocol
Preparation for RAI therapy includes several steps for effectiveness and safety. Patients follow a low-iodine diet before treatment to increase thyroid cell uptake. They also stop thyroid hormone replacement to raise TSH levels, aiding in radioactive iodine absorption.
Administration Process
The therapy involves swallowing a capsule or liquid with radioactive iodine. The dose is tailored to the patient’s condition and cancer spread. Afterward, patients are watched for side effects and precautions are taken to limit radiation exposure to others.
Side Effects and Safety Precautions
While RAI therapy is mostly safe, side effects can include sialadenitis, taste changes, and reproductive system issues. It’s vital to follow safety measures to reduce radiation exposure to family, caregivers, and the public. This includes hygiene guidelines, restrictions on close contact, and handling of bodily fluids.
External Beam Radiation Therapy
External Beam Radiation Therapy (EBRT) is a vital treatment for thyroid cancer, mainly in advanced stages. It uses high-energy beams from outside the body to target and destroy cancer cells.
Indications for External Radiation
EBRT is often advised for thyroid cancer patients who have had surgery but face a high risk of recurrence or remaining disease. It’s also considered for those with tumors that cannot be removed or who haven’t responded to other treatments.
- High-risk patients after surgery
- Inoperable tumors
- Residual disease
Treatment Planning and Delivery
The EBRT process starts with treatment planning. A team of radiation oncologists and physicists create a personalized plan. They use imaging studies to locate the tumor precisely and determine the best dosage and beam angles.

Managing Radiation Side Effects
EBRT is effective but can lead to side effects like fatigue, skin irritation, and difficulty swallowing. It’s essential to manage these side effects to maintain the patient’s quality of life. This can involve medication, dietary changes, and rest.
Understanding EBRT’s indications, treatment process, and side effects helps both patients and healthcare providers make informed decisions. This is key in thyroid cancer treatment.
Systemic Therapies for Advanced Thyroid Cancer
Systemic therapies have become essential in managing advanced thyroid cancer. They target cancer that has spread beyond the thyroid gland. This approach offers a more complete way to handle the disease.
Targeted Therapy Options
Targeted therapy has transformed the treatment of advanced thyroid cancer. It focuses on specific molecular targets involved in cancer cell growth and progression.
Tyrosine Kinase Inhibitors
Tyrosine kinase inhibitors (TKIs) have shown great promise in treating advanced thyroid cancer. Drugs like sorafenib and lenvatinib have been approved for treating radioactive iodine-refractory differentiated thyroid cancer.
Other Targeted Agents
Other targeted agents are also being explored for advanced thyroid cancer treatment. These include drugs targeting the BRAF mutation, common in papillary thyroid cancer.
Conventional Chemotherapy Approaches
Chemotherapy has traditionally been used for advanced thyroid cancer, though its effectiveness varies. It’s considered when targeted therapies are not suitable or have failed.
Emerging and Investigational Treatments
The treatment landscape for advanced thyroid cancer is constantly evolving. New therapies, like immunotherapies and combination regimens, are showing promise. These include checkpoint inhibitors and pairing different targeted therapies.
As research delves deeper into thyroid cancer’s molecular basis, new systemic therapies are expected. These advancements aim to improve outcomes for patients with advanced disease.
Thyroid Hormone Replacement Therapy
Thyroid hormone replacement therapy is a key part of treating thyroid cancer. It’s essential for those who’ve had thyroid surgery. It helps replace lost thyroid function, aiming to restore normal hormone levels. These hormones are vital for metabolism, growth, and development.
The Importance of Hormone Replacement
Thyroid hormone replacement is critical because the thyroid regulates metabolism. Without enough hormones, patients may feel tired, gain weight, and face metabolic problems. This therapy ensures normal metabolic functions and overall health.
Medication Management
Effective medication management is vital for thyroid hormone replacement. Patients usually take synthetic thyroid hormone, like levothyroxine. It’s made to mimic the thyroid’s natural hormone. Dosage is adjusted based on blood tests to keep hormone levels in check.
Monitoring and Adjusting Hormone Levels
Regular monitoring is key to adjusting medication dosage. Blood tests check thyroid-stimulating hormone (TSH) and other hormone levels. Healthcare providers use these results to fine-tune the dosage, ensuring the patient’s thyroid function is supported.
Understanding the role of thyroid hormone replacement therapy is essential. Working closely with healthcare providers helps patients manage their condition. This improves their quality of life significantly.
Follow-up Care and Surveillance Protocols
Effective follow-up care is essential for thyroid cancer patients. It ensures the success of their treatment and catches any recurrence early. A thorough follow-up plan includes regular check-ups, diagnostic tests, and monitoring for recurrence or metastasis signs.
Short-term Monitoring
After treatment, patients undergo short-term monitoring. This involves regular physical exams, thyroid function tests, and imaging like ultrasound or CT scans. Such close watch helps spot immediate complications or early recurrence signs.
Patients are also watched for treatment side effects, like hypothyroidism or hypoparathyroidism. These are managed as needed.
Long-term Surveillance Strategies
Long-term surveillance for thyroid cancer patients includes regular follow-up visits. These are usually every 6-12 months, based on the patient’s risk and treatment response. For those who had total thyroidectomy, serum thyroglobulin (Tg) measurements and ultrasound exams are key. They help monitor for neck recurrences.

Detecting and Managing Recurrence
Detecting recurrence early is vital for effective management. Surveillance protocols aim to catch recurrence early, when it’s more treatable. If recurrence is found, treatment options like surgery, radioactive iodine therapy, or external beam radiation therapy may be considered.
Patients are also taught to recognize recurrence signs and symptoms. This empowers them to seek medical help quickly if they notice any concerning changes.
Living With Thyroid Cancer
Living with thyroid cancer is a journey filled with emotional, psychological, and physical challenges. The diagnosis can trigger a mix of emotions, from fear and anxiety to determination and resilience. It’s a path that requires strength and support.
Emotional and Psychological Impact
The emotional and psychological impact of thyroid cancer is profound. Patients often experience a range of emotions, including shock, denial, anger, and sadness. The uncertainty surrounding the disease and its treatment can cause significant distress.
Seeking support from mental health professionals, family, and friends is essential. It’s important for patients to express their feelings and seek help when needed.
Support Resources and Patient Communities
Support resources are vital for patients dealing with thyroid cancer. Patient communities, both online and offline, offer a space to share experiences, advice, and support.
- Online forums and social media groups dedicated to thyroid cancer
- Local support groups and cancer organizations
- Professional counseling services
These resources help patients feel less isolated and more empowered to manage their condition.
Lifestyle Adjustments and Coping Strategies
Lifestyle adjustments are often necessary for patients undergoing treatment for thyroid cancer. This can include dietary changes, managing fatigue, and adapting to new physical limitations.
Coping strategies, such as mindfulness, meditation, and yoga, can also be beneficial. They help manage stress and improve overall well-being.
By making informed lifestyle choices and utilizing available support resources, patients can improve their quality of life while living with thyroid cancer.
Prognosis and Survival Rates for Thyroid Cancer
The prognosis for thyroid cancer varies significantly based on several key factors. Understanding these factors is essential for patients and healthcare providers. It helps determine the most appropriate treatment plan and predict outcomes.
Factors Influencing Prognosis
Several elements influence the prognosis of thyroid cancer. These include:
- The type of thyroid cancer
- The stage at diagnosis
- The patient’s age and overall health
- The presence of genetic mutations
- The response to initial treatment
Papillary thyroid cancer generally has a more favorable prognosis compared to anaplastic thyroid cancer. Early-stage diagnosis significantly improves the prognosis. Advanced stages pose greater challenges.
Survival Statistics by Cancer Type and Stage
Survival rates for thyroid cancer are typically categorized based on the type and stage of the cancer. The overall 5-year survival rate for thyroid cancer is high, mainly for papillary and follicular types.
Here are some general survival statistics:
| Cancer Type | Stage | 5-Year Survival Rate |
|---|---|---|
| Papillary | Localized | Almost 100% |
| Follicular | Regional | 70-90% |
| Medullary | Distant | 40-60% |
| Anaplastic | Advanced | Less than 10% |
These statistics highlight the importance of early detection. They also show the varying prognoses associated with different thyroid cancer types and stages.
The Future of Thyroid Cancer Care: Research Breakthroughs and Hope
The field of thyroid cancer care is rapidly advancing, thanks to ongoing Thyroid Cancer Research. Recent discoveries have shed light on the genetic and molecular causes of thyroid cancer. This knowledge is leading to the development of new treatments and therapies.
Targeted therapies are at the forefront of research, aiming to destroy cancer cells while sparing healthy tissue. Several drugs have shown great promise in clinical trials. They offer hope to patients with advanced or resistant thyroid cancer.
Advances in diagnostic techniques are also on the horizon. These will enable earlier detection and more accurate staging of thyroid cancer. Improved imaging and biomarker identification will enhance treatment planning and patient outcomes.
As research delves deeper into thyroid cancer’s complexities, the medical community is dedicated to applying these findings in clinical settings. Collaboration between researchers, clinicians, and patients is key. It drives progress and improves the lives of those battling thyroid cancer.
FAQ
Q: What is thyroid cancer?
A: Thyroid cancer is a form of cancer that impacts the thyroid gland. This gland, shaped like a butterfly, is in the neck. It produces hormones that control growth and development.
Q: What are the different types of thyroid cancer?
A: There are four main types of thyroid cancer: papillary, follicular, medullary, and anaplastic. Each type has its own characteristics and treatment methods.
Q: What are the risk factors for developing thyroid cancer?
A: Several factors increase the risk of thyroid cancer. These include genetic predispositions, radiation exposure, and demographic traits. Being female and aged 25 to 65 are significant risk factors.
Q: What are the signs and symptoms of thyroid cancer?
A: Signs of thyroid cancer include a neck lump or swelling, difficulty swallowing, hoarseness, and neck pain. Many cases, though, show no symptoms at all.
Q: How is thyroid cancer diagnosed?
A: Diagnosing thyroid cancer involves physical exams, blood tests, and imaging studies. These include ultrasound, CT, MRI, and PET scans. A biopsy is also used to confirm the diagnosis.
Q: What are the treatment options for thyroid cancer?
A: Treatments for thyroid cancer include surgery, radioactive iodine therapy, and external beam radiation. Systemic therapies like targeted therapy and chemotherapy are also used.
Q: What is the role of thyroid hormone replacement therapy in managing thyroid cancer?
A: Thyroid hormone replacement therapy is vital for patients after thyroid surgery. It replaces the hormones the thyroid gland would normally produce. This helps regulate metabolism and prevents hypothyroidism.
Q: How is thyroid cancer staged, and what does it mean for treatment and prognosis?
A: Thyroid cancer staging uses the TNM system. It considers tumor size, lymph node involvement, and metastasis. This information guides treatment and predicts prognosis.
Q: What is the prognosis for thyroid cancer, and what are the survival rates?
A: Thyroid cancer prognosis varies by type and stage. Survival rates range from 80% to over 95% for certain types and stages.
Q: What are the latest developments in thyroid cancer research and treatment?
A: Research focuses on new treatments like targeted and immunotherapies. It also aims to improve diagnostic techniques and understand thyroid cancer’s genetic and molecular mechanisms.