Trigeminal Neuralgia is a chronic pain condition that affects the trigeminal nerve. It causes intense shock-like or stabbing pain in parts of the face. This condition can significantly impact a person’s quality of life, making everyday activities challenging. Understanding the causes, symptoms, and treatments of this condition is key to managing its effects. The trigeminal nerve is responsible for sensation in the face and motor functions such as chewing. When this nerve is damaged or compressed, it can lead to the development of Trigeminal Neuralgia.
By exploring the various aspects of this condition, individuals can better navigate their diagnosis and treatment options. This can ultimately improve their overall well-being.
Understanding Trigeminal Neuralgia
To grasp trigeminal neuralgia, one must understand its definition, clinical importance, and historical background. This condition impacts the trigeminal nerve, which controls facial sensations. It can cause severe, debilitating pain.
Definition and Clinical Significance
Trigeminal neuralgia is marked by intense, shock-like or stabbing pain in the face. Its clinical significance is evident in its impact on the quality of life for those affected. It often necessitates a detailed management plan. The diagnosis is based on clinical presentation and ruling out other facial pain causes.
The pain from trigeminal neuralgia can be triggered by simple actions like eating, talking, or even light touch to the face. Recognizing its clinical significance is key to developing effective treatment strategies.
Historical Perspective and Evolution of Understanding
Trigeminal neuralgia has been documented for centuries, with the first descriptions appearing in the 18th century. The understanding of this condition has grown, from initial pain descriptions to today’s knowledge of its pathophysiology.
Neuroimaging and neurosurgery advancements have been vital in this evolution. They have enabled more accurate diagnoses and treatments. The historical context is essential for understanding current management approaches to trigeminal neuralgia.
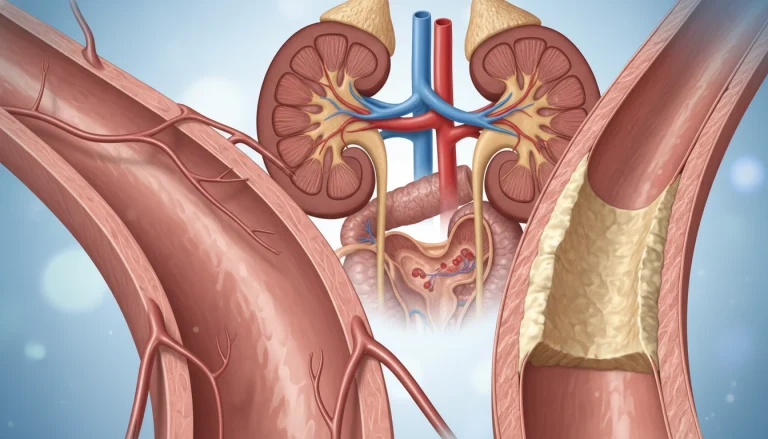
Anatomy of the Trigeminal Nerve
Grasping the trigeminal nerve’s anatomy is key to diagnosing and treating trigeminal neuralgia. This nerve, the fifth cranial nerve, is complex. It handles both sensory and motor functions of the face.
Structure and Functional Importance
The trigeminal nerve consists of a large sensory root and a smaller motor root. The sensory root transmits sensory data from the face to the brain. The motor root, on the other hand, controls the muscles of mastication. This dual role makes the trigeminal nerve essential for facial sensation and motor control.
Distribution and Innervation Patterns
The trigeminal nerve splits into three main divisions: the ophthalmic, maxillary, and mandibular divisions. Each division has unique innervation patterns and sensory distribution areas.
Ophthalmic Division (V1)
The ophthalmic division covers the eye and surrounding areas, including the forehead and nose. It’s responsible for their sensory innervation.
Maxillary Division (V2)
The maxillary division innervates the mid-face region. This includes the maxillary sinus and upper teeth.
Mandibular Division (V3)
The mandibular division has both sensory and motor functions. It innervates the lower face, including the lower teeth, and controls the muscles of mastication.
Knowing these divisions and their innervation patterns is vital for diagnosing and managing trigeminal neuralgia effectively.
Epidemiology of Trigeminal Neuralgia
Trigeminal neuralgia’s prevalence and distribution are illuminated by epidemiological data. This knowledge is vital for pinpointing risk factors, allocating healthcare resources, and crafting specific interventions.
Global Prevalence and Incidence Rates
Trigeminal neuralgia is deemed rare, with an incidence rate of 4-13 per 100,000 annually. Estimated prevalence hovers around 15-27 per 100,000. These figures underscore the condition’s rarity yet highlight its substantial impact on those it affects.
Demographic Distribution and Risk Patterns
Trigeminal neuralgia’s demographic patterns reveal specific risk factors. Age, gender, geographic location, and ethnicity are all critical considerations.
Age and Gender Considerations
Primarily affecting older adults, with most cases occurring post-50, trigeminal neuralgia shows a gender bias. Women are slightly more prone to the condition than men.
Geographic and Ethnic Variations
Research hints at geographic and ethnic disparities in trigeminal neuralgia incidence. Further investigation is necessary to solidify these findings.
Pathophysiology and Underlying Mechanisms
To grasp the pathophysiology of Trigeminal Neuralgia, we must explore both neurovascular compression and neural changes. This condition’s complexity stems from various factors influencing its development and progression.
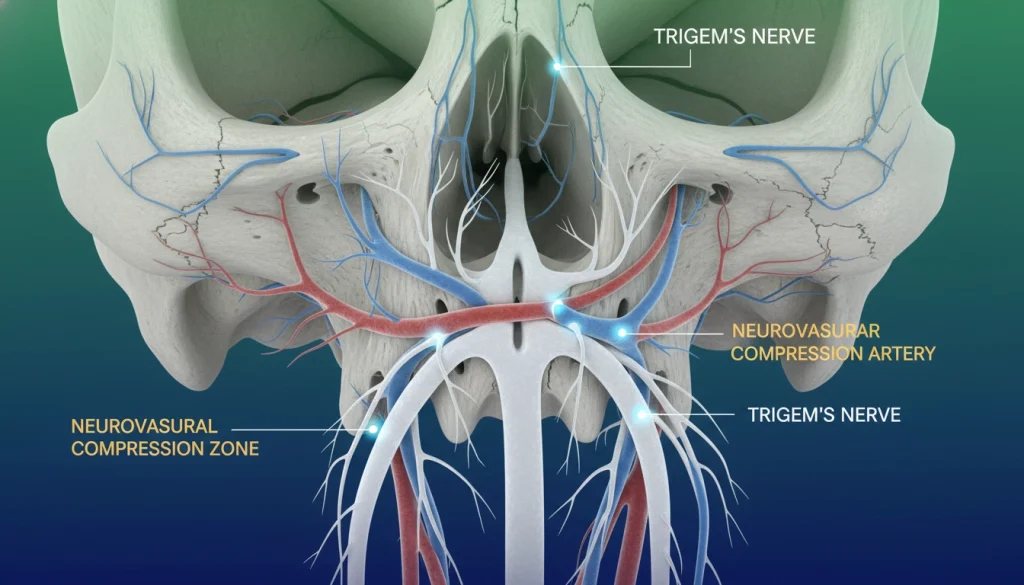
Neurovascular Compression Theory
The neurovascular compression theory is a leading explanation for Trigeminal Neuralgia. It suggests that the trigeminal nerve’s compression by blood vessels causes the pain characteristic of the condition.
- Compression usually happens at the nerve’s root entry zone.
- Arteries or veins can cause this compression.
- This compression damages the myelin sheath, disrupting nerve function.
Demyelination and Neural Hyperexcitability
Demyelination and neural hyperexcitability are key in Trigeminal Neuralgia’s pathophysiology. Demyelination is the loss of the myelin sheath around nerve fibers, causing abnormal signal transmission.
- Demyelination can stem from neurovascular compression or other causes.
- Myelin loss leads to hyperexcitability of the trigeminal nerve.
- This hyperexcitability is a major contributor to the pain episodes patients experience.
Understanding these mechanisms is vital for developing effective treatments for Trigeminal Neuralgia. By tackling both neurovascular compression and neural changes, healthcare professionals can provide more effective care.
Causes and Risk Factors
The etiology of Trigeminal Neuralgia can be broadly categorized into primary and secondary forms, each with distinct characteristics. Understanding these causes is essential for appropriate management and treatment.
Primary (Classical) Trigeminal Neuralgia
Primary Trigeminal Neuralgia, also known as classical Trigeminal Neuralgia, is typically caused by neurovascular compression. This compression occurs when a blood vessel presses against the trigeminal nerve, leading to pain. The compression damages the myelin sheath surrounding the nerve, causing the nerve to malfunction.
Secondary Trigeminal Neuralgia
Secondary Trigeminal Neuralgia results from identifiable causes other than neurovascular compression. The causes can be categorized into several types:
- Multiple Sclerosis-Related TN
- Tumor-Associated TN
- Post-Traumatic and Post-Herpetic TN
Multiple Sclerosis-Related TN
In some cases, Trigeminal Neuralgia is associated with multiple sclerosis, a chronic disease affecting the central nervous system. Demyelination plaques in multiple sclerosis can affect the trigeminal nerve, leading to neuralgia.
Tumor-Associated TN
Tumors, such as those located at the cerebellopontine angle, can compress the trigeminal nerve, causing neuralgia. Meningiomas and acoustic neuromas are examples of tumors that can lead to Trigeminal Neuralgia.
Post-Traumatic and Post-Herpetic TN
Trauma to the face or head can result in Trigeminal Neuralgia. Herpes zoster infection (shingles) affecting the trigeminal nerve can also lead to post-herpetic neuralgia, a form of Trigeminal Neuralgia.
Understanding these causes is critical for determining the appropriate treatment plan.
Clinical Presentation of Trigeminal Neuralgia
Trigeminal neuralgia is characterized by distinct pain patterns, essential for diagnosis and treatment. Healthcare providers must grasp these patterns to craft effective management plans.
Characteristic Pain Patterns
The pain of trigeminal neuralgia is severe and stabbing, akin to an electric shock. It predominantly affects one side of the face, making it unilateral.
Quality and Intensity of Pain
The pain is sharp and stabbing, with an intensity that can be overwhelming. It’s so severe, it can hinder daily activities.
Duration and Frequency of Attacks
Attacks can last from seconds to minutes, with periods of relief in between. The frequency varies widely among individuals.
Refractory Periods
After an attack, a refractory period ensues where pain cannot be triggered. The length of this period varies.
Trigger Factors and Trigger Zones
Trigger factors are key in trigeminal neuralgia, causing pain attacks with specific stimuli. Common areas include the face, around the nose and mouth.
Recognizing and understanding these triggers is vital for managing the condition effectively.
Diagnostic Approach and Evaluation
Accurate diagnosis of Trigeminal Neuralgia requires a detailed clinical history, thorough examination, and neuroimaging. This multi-faceted approach is essential for distinguishing Trigeminal Neuralgia from other conditions with similar symptoms.
Clinical History and Examination
A detailed clinical history is key for diagnosing Trigeminal Neuralgia. Patients often report sudden, severe, stabbing pain on one side of the face. This pain can be triggered by everyday activities like eating, talking, or even light touch. A thorough neurological examination is also vital. It helps assess for any sensory or motor deficits and identifies trigger zones.
- Assess pain characteristics, including location, duration, and intensity
- Identify trigger factors and trigger zones
- Evaluate for any neurological deficits
Neuroimaging Techniques
Neuroimaging is critical in diagnosing Trigeminal Neuralgia, mainly to rule out secondary causes like tumors or vascular abnormalities. Magnetic Resonance Imaging (MRI) is the preferred imaging modality.
MRI Protocol for Trigeminal Neuralgia
The MRI protocol for Trigeminal Neuralgia includes high-resolution sequences to visualize the trigeminal nerve and its surroundings. This may involve 3D T1-weighted and T2-weighted images.
Advanced Imaging Modalities
Advanced imaging techniques, such as Diffusion Tensor Imaging (DTI) and Magnetic Resonance Angiography (MRA), offer additional insights. They help understand the integrity of the trigeminal nerve and its relationship with adjacent vascular structures.
Differential Diagnosis Considerations
When diagnosing Trigeminal Neuralgia, it’s important to consider other conditions with similar facial pain. These include dental problems, temporomandibular joint disorders, and other neuropathic pain conditions. A thorough clinical evaluation and appropriate neuroimaging can help differentiate these conditions.
- Dental pain
- Temporomandibular joint disorder
- Other neuropathic pain conditions
Classification Systems for Trigeminal Neuralgia
Accurate classification of trigeminal neuralgia is essential for effective patient care and research. Classification systems help clinicians and researchers categorize the condition. They understand its various forms and develop appropriate treatment plans. Over the years, several classification systems have been developed to diagnose and manage trigeminal neuralgia.
International Headache Society Classification
The International Headache Society (IHS) classification system is widely recognized and used in diagnosing trigeminal neuralgia. It categorizes trigeminal neuralgia under the category of painful cranial neuropathies. The IHS classification provides specific diagnostic criteria, including the presence of paroxysmal pain and trigger factors.
It also differentiates between classical and secondary trigeminal neuralgia. This differentiation is critical for determining the underlying cause and guiding treatment.
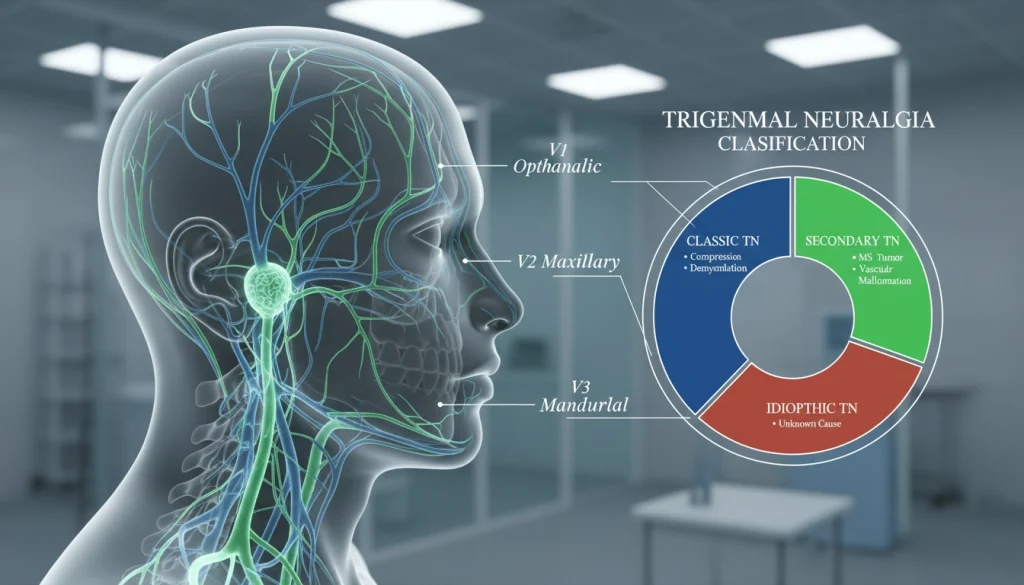
Burchiel Classification and Other Systems
The Burchiel classification is another significant system used to categorize trigeminal neuralgia. It differentiates between trigeminal neuralgia types based on clinical characteristics. These include the presence of trigeminal pain and neurological deficits.
Other classification systems, like the one proposed by the International Association for the Study of Pain, also provide valuable frameworks. These systems complement each other, providing a more complete understanding of diagnosing and managing the condition.
Pharmacological Management Strategies
Effective management of Trigeminal Neuralgia often begins with pharmacological options. The primary goal is to reduce or eliminate the pain associated with this condition.
First-Line Anticonvulsant Medications
Anticonvulsants are the first line of treatment for Trigeminal Neuralgia. They work by stabilizing the neural membrane and reducing the excitability of neurons.
Carbamazepine and Oxcarbazepine
Carbamazepine is considered the gold standard for treating Trigeminal Neuralgia. Oxcarbazepine, a derivative of carbamazepine, offers a similar efficacy profile with potentially fewer side effects.
Dosing Strategies and Monitoring
Dosing starts low and is gradually increased until pain relief is achieved or side effects become limiting. Regular monitoring of blood counts and liver function is necessary.
Second-Line and Adjunctive Medications
For patients who do not respond to first-line treatments or experience significant side effects, second-line and adjunctive medications are considered.
Gabapentin and Pregabalin
- Gabapentin is used off-label for Trigeminal Neuralgia.
- Pregabalin, with its similar mechanism, is also considered.
Baclofen and Muscle Relaxants
Baclofen can be used alone or in combination with anticonvulsants for additive effect.
Tricyclic Antidepressants
Though primary use is for depression, tricyclic antidepressants can also manage neuropathic pain.
Managing Medication Side Effects
Managing side effects is critical for maintaining patient compliance. Common side effects include drowsiness, dizziness, and ataxia.
Adjusting dosages or switching medications can mitigate these effects.
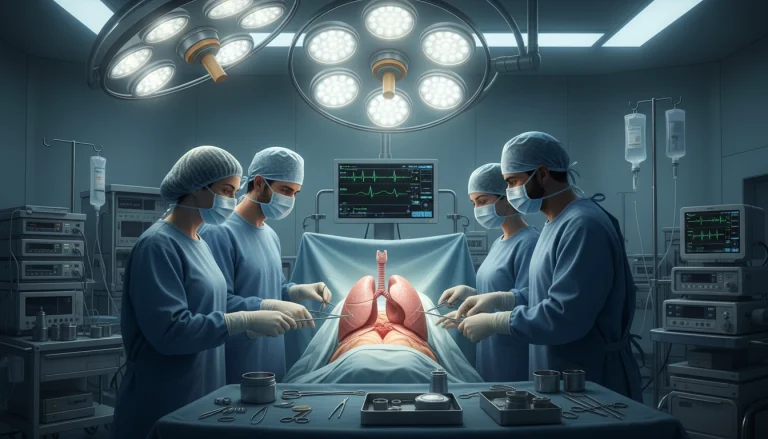
Surgical Interventions for Trigeminal Neuralgia
Trigeminal Neuralgia treatment has evolved to include various surgical interventions. These can offer substantial pain relief for patients who do not respond to or cannot tolerate medical therapy.
Microvascular Decompression
Microvascular decompression is a surgical procedure that relieves compression on the trigeminal nerve. This compression is often caused by blood vessels that come into contact with the nerve.
Surgical Technique
The procedure involves a craniotomy to access the trigeminal nerve. The surgeon then identifies and gently moves the compressing blood vessel away from the nerve. A cushion is often placed between them to prevent further contact.
Outcomes and Recurrence Rates
Microvascular decompression provides significant pain relief in most patients. Yet, recurrence rates vary, with some studies indicating a recurrence rate of up to 30% over 10 years.
Potential Complications
Potential complications include infection, hearing loss, and facial numbness. Serious complications are rare but can be significant.
Percutaneous Ablative Procedures
Percutaneous ablative procedures involve creating a lesion on the trigeminal nerve to disrupt pain signals. These procedures are less invasive than microvascular decompression.
Glycerol Rhizotomy
Glycerol rhizotomy involves injecting glycerol into the trigeminal cistern to damage the nerve and reduce pain.
Radiofrequency Thermocoagulation
This procedure uses a heated electrode to create a lesion on the trigeminal nerve, providing pain relief.
Balloon Microcompression
Balloon microcompression involves inflating a balloon to compress the trigeminal nerve, creating a lesion that disrupts pain signals.
Stereotactic Radiosurgery (Gamma Knife)
Stereotactic radiosurgery, also known as Gamma Knife, delivers a high dose of radiation to the trigeminal nerve. This creates a lesion that can provide pain relief.
The procedure is non-invasive and can be beneficial for patients who are not good candidates for more invasive surgeries.
- Provides pain relief without the need for open surgery
- Can be effective for patients with certain health conditions
- May have fewer complications compared to other surgical options
Complementary and Alternative Treatment Approaches
Integrating complementary and alternative therapies into the management of Trigeminal Neuralgia can significantly enhance treatment outcomes. These methods offer relief and improve the quality of life for those affected by this condition.
Physical and Manual Therapies
Physical and manual therapies are gaining recognition for their role in managing Trigeminal Neuralgia. Techniques like massage, chiropractic care, and physical therapy can help by reducing muscle tension and improving nerve function.
- Massage therapy to relax facial muscles
- Chiropractic adjustments to improve nerve function
- Physical therapy to enhance overall well-being
Mind-Body Interventions and Neuromodulation
Mind-body interventions and neuromodulation techniques offer additional strategies for managing Trigeminal Neuralgia. These approaches focus on the interplay between the brain and the body to reduce pain and improve function.
Acupuncture and Acupressure
Acupuncture and acupressure involve stimulating specific points on the body to promote healing and pain relief. These techniques can be effective in reducing the frequency and severity of Trigeminal Neuralgia episodes.
Biofeedback and Relaxation Techniques
Biofeedback and relaxation techniques, such as meditation and deep breathing, help individuals manage stress and reduce pain. By gaining control over physiological responses, patients can better cope with their symptoms.
Transcutaneous Electrical Nerve Stimulation
Transcutaneous Electrical Nerve Stimulation (TENS) is a non-invasive technique that applies electrical currents to the affected area, providing pain relief by interrupting pain signals to the brain.
Living with Trigeminal Neuralgia
Managing Trigeminal Neuralgia (TN) demands a holistic approach. It includes lifestyle changes, pain control, and emotional support. By effectively managing TN, one can greatly enhance their quality of life.
Daily Management and Lifestyle Modifications
Effective daily management of TN involves several lifestyle adjustments. These changes can help reduce the occurrence and intensity of episodes.
Dietary Considerations
Staying away from trigger foods and maintaining a balanced diet is key. Some people find that specific foods or drinks can trigger or worsen their symptoms.
Environmental Adaptations
Adapting to the environment, like avoiding cold winds or extreme temperatures, can also be helpful.
Oral and Facial Care Strategies
Good oral hygiene and gentle facial care are important. They help avoid triggers related to touch or pressure.

Coping Strategies and Pain Management Techniques
Coping with TN involves a mix of pain management and emotional support. Techniques like relaxation, meditation, and cognitive-behavioral therapy can help manage the condition’s psychological effects.
By adopting these strategies and collaborating with healthcare professionals, individuals with TN can manage their condition better. This leads to improved overall well-being.
Psychological Impact and Support Resources
Living with Trigeminal Neuralgia profoundly affects one’s mental state, highlighting the importance of strong support systems. The unpredictable nature of pain episodes and the difficulty in managing them can lead to severe mental health issues.
Mental Health Considerations and Comorbidities
Those with Trigeminal Neuralgia often face anxiety, depression, and other mental health problems. The fear of pain can severely impact their quality of life.
Research indicates a high rate of mental health disorders among Trigeminal Neuralgia patients. This underlines the necessity for care that addresses both physical and psychological needs.
Support Groups and Patient Resources
Support groups are vital for patients dealing with Trigeminal Neuralgia. They offer a space to share experiences, receive support, and learn about managing the condition.
Online Communities and Organizations
Online forums and organizations focused on Trigeminal Neuralgia provide essential resources. They include support networks and educational materials, helping patients connect with others who share their experiences.
Educational Materials and Self-Management Tools
Educational materials and self-management tools empower patients to manage their condition. They aid in understanding the condition, managing pain, and improving overall well-being.
By utilizing these support resources, patients with Trigeminal Neuralgia can better manage their condition and enhance their mental health.
Special Populations and Considerations
Special populations, including the elderly and pregnant women, face unique challenges in managing trigeminal neuralgia. These groups need tailored approaches due to their distinct physiological conditions and comorbidities.
Trigeminal Neuralgia in the Elderly
The elderly are disproportionately affected by trigeminal neuralgia, with prevalence rates rising with age. Age-related changes, such as vascular alterations and cognitive decline, complicate diagnosis and treatment. It’s vital to consider comorbid conditions and concurrent medications when managing this condition in older adults.
Trigeminal Neuralgia in Pregnancy and Other Special Situations
Trigeminal neuralgia in pregnancy adds extra challenges due to the limited use of certain medications. Alternative management strategies, like careful medication selection and adjusting treatment plans postpartum, are essential. Other special situations, such as multiple sclerosis or patients with previous surgical interventions, also demand nuanced management approaches.
Current Research and Emerging Therapies
The field of Trigeminal Neuralgia management is rapidly advancing. Ongoing research is uncovering new therapeutic options. As our knowledge of the condition grows, innovative treatments are being developed to meet patient needs.
Novel Pharmacological Approaches
New pharmacological agents are a key area of research. Pregabalin and gabapentin are being studied for their effectiveness in managing pain. The exploration of cannabinoids and other compounds is also underway.
Advances in Surgical Techniques and Neuromodulation
Surgical techniques are also undergoing significant improvements. Microvascular decompression and stereotactic radiosurgery are being refined to offer better results. Neuromodulation therapies, like peripheral nerve stimulation, are emerging as viable options for those who don’t respond to traditional treatments.
These advancements highlight the dedication to enhance patient care and outcomes in Trigeminal Neuralgia management.
The Path Forward: Integrating Care for Optimal Outcomes
Managing Trigeminal Neuralgia effectively requires a holistic approach. This involves combining medical, surgical, and supportive strategies. Such integration enables healthcare providers to deliver the best results for patients.
Understanding the condition’s causes, symptoms, and diagnostic methods is key. Treatment plans, whether through medication or surgery, must be customized for each patient. This ensures the most effective care.
An integrated care model ensures patients get the right treatment. This could be medication, surgery, or alternative therapies. This approach not only relieves symptoms but also enhances the patient’s overall well-being.
By adopting an integrated care model, healthcare providers can offer top-notch, patient-focused care. This addresses the complex needs of those with Trigeminal Neuralgia, leading to the best possible outcomes.
FAQ
Q: What is Trigeminal Neuralgia?
A: Trigeminal Neuralgia is a chronic pain condition affecting the trigeminal nerve. It causes intense pain in the face.
Q: What are the symptoms of Trigeminal Neuralgia?
A: Symptoms include sudden, severe, stabbing pain on one side of the face. This pain is often triggered by everyday activities like eating, talking, or brushing teeth.
Q: What causes Trigeminal Neuralgia?
A: The exact cause is often unknown. It’s believed to be related to compression of the trigeminal nerve by a blood vessel or other structural issues.
Q: How is Trigeminal Neuralgia diagnosed?
A: Diagnosis is based on clinical history, physical examination, and neuroimaging techniques like MRI. These are used to rule out other causes.
Q: What are the treatment options for Trigeminal Neuralgia?
A: Treatment options include medications like carbamazepine and surgical interventions such as microvascular decompression. Complementary therapies like acupuncture are also considered.
Q: Can Trigeminal Neuralgia be cured?
A: While there is no definitive cure, many people experience significant relief with treatment. Some may have periods of remission.
Q: How does Trigeminal Neuralgia affect daily life?
A: Trigeminal Neuralgia can significantly impact daily activities. It causes pain that interferes with eating, speaking, and social interactions.
Q: Are there any support resources for Trigeminal Neuralgia patients?
A: Yes, there are support groups, online communities, and organizations. They provide information, emotional support, and self-management tools.
Q: Can Trigeminal Neuralgia occur in children or during pregnancy?
A: While rare, Trigeminal Neuralgia can occur in children and during pregnancy. It requires special consideration in management and treatment.
Q: What is the role of lifestyle modifications in managing Trigeminal Neuralgia?
A: Lifestyle modifications, including dietary changes and stress management, can help alleviate symptoms. They improve quality of life.