Type 1 Diabetes: What Is Type 1 Diabetes
Type 1 Diabetes is a chronic condition where the pancreas fails to produce enough insulin. This hormone is essential for glucose regulation in the body. This condition has a profound impact on individuals, affecting their daily lives. It requires careful management to maintain health and prevent complications.
Proper Diabetes Management involves monitoring blood glucose levels and administering insulin. Adopting a healthy lifestyle is also key to mitigating the condition’s effects. Effective management allows individuals with Type 1 Diabetes to lead active and fulfilling lives. This highlights the importance of awareness and proper care. Type 1 diabetes is a condition where the body can’t make insulin due to an autoimmune attack. It’s vital to grasp its underlying causes and how it differs from other diabetes types.
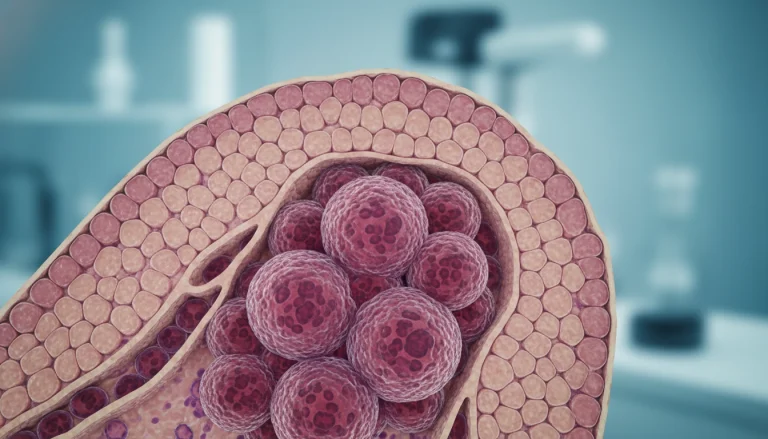
The Autoimmune Process
Type 1 diabetes occurs when the immune system mistakenly attacks the pancreas’s insulin-producing beta cells. This autoimmune response is complex, influenced by genetics and environmental factors.
Beta Cell Destruction
The loss of beta cells severely reduces insulin production. Insulin is key for glucose to enter cells. Without it, glucose builds up in the blood, causing high blood sugar.
Insulin Deficiency
Insulin deficiency is the outcome of beta cell loss. This requires taking insulin from outside to manage blood sugar levels. This is what sets Type 1 diabetes apart from other types.
Differences from Type 2 Diabetes
Type 1 diabetes is often mistaken for Type 2, but they are different. Type 2 is linked to insulin resistance and impaired insulin secretion, often seen in obesity and lack of exercise. Type 1, on the other hand, is an autoimmune disease causing complete insulin deficiency.
Managing Type 1 diabetes involves insulin therapy, blood glucose monitoring, and lifestyle changes. These efforts are aimed at keeping blood sugar levels in check.
Causes and Risk Factors
The exact cause of Type 1 diabetes is not fully understood. Yet, research has pinpointed several key risk factors. These factors are vital for early detection and prevention of the disease.
Genetic Predisposition
Genetic predisposition significantly influences Type 1 diabetes development. Those with a family history are at greater risk. Specific genetic markers, like HLA-A, HLA-B, and HLA-DR, are linked to higher susceptibility.
Environmental Triggers
Environmental factors also play a role in triggering Type 1 diabetes in those genetically predisposed. Viral infections and early dietary factors are two such triggers.
Viral Infections
Viral infections, such as coxsackievirus B, are associated with Type 1 diabetes onset. These viruses can initiate an autoimmune response, destroying insulin-producing cells in the pancreas.
Early Dietary Factors
Early dietary factors, including infant feeding practices, are under investigation as risk factors. Some research indicates that introducing certain foods, like cow’s milk or gluten, early may increase Type 1 diabetes risk.
Demographics and Prevalence
Type 1 diabetes can affect anyone, but it’s most common in children and young adults. Its prevalence varies globally, with higher rates in some European countries and North America. Recognizing these patterns aids in identifying at-risk populations and directing healthcare resources.
Recognizing the Symptoms
Type 1 Diabetes often presents with distinct symptoms that, when recognized early, can lead to prompt medical intervention. Early detection is key for effective management and prevention of serious complications.
Early Warning Signs
The onset of Type 1 Diabetes can be marked by several early warning signs. These include the classic “three Ps” and other common symptoms.
The Classic “Three Ps”
The “three Ps” – polyuria (frequent urination), polydipsia (increased thirst), and polyphagia (increased hunger) – are hallmark symptoms. Polyuria occurs due to the body’s attempt to flush out excess glucose, leading to dehydration and increased thirst.
Other Common Symptoms
Other symptoms include unexplained weight loss, fatigue, and blurred vision. These occur due to the body’s inability to use glucose for energy.
Diabetic Ketoacidosis (DKA)
A serious complication of Type 1 Diabetes is diabetic ketoacidosis (DKA), a condition that requires immediate medical attention.
Warning Signs of DKA
Warning signs include nausea, vomiting, abdominal pain, and fruity-smelling breath. These symptoms indicate that the body is producing high levels of ketones.
When to Seek Emergency Care
If symptoms of DKA are observed, it’s vital to seek emergency care promptly. DKA can lead to severe complications if not treated in a timely manner.
Diagnosis Process
The diagnosis of Type 1 Diabetes involves a detailed process, using various blood tests to confirm its presence. These tests help distinguish it from other diabetes types.
Blood Tests and Criteria
Blood tests are essential in diagnosing Type 1 Diabetes. They identify specific markers and glucose levels in the blood.
Fasting Plasma Glucose
The Fasting Plasma Glucose (FPG) test measures blood glucose after an overnight fast. High levels indicate diabetes.
Antibody Testing
Antibody testing detects autoantibodies linked to Type 1 Diabetes. Finding these antibodies confirms the diagnosis.
A1C Testing
A1C testing shows average blood glucose levels over 2-3 months. It’s not exclusive to Type 1 but is useful for glucose control insights.
Differentiating from Other Diabetes Types
Distinguishing Type 1 Diabetes from Type 2 is vital for proper treatment. Type 1 is marked by autoantibodies and a quick onset, often in the young.
Healthcare providers use clinical presentation, family history, and test results to accurately diagnose.
Insulin Therapy Fundamentals
Managing Type 1 Diabetes effectively requires insulin therapy. This involves giving insulin to mimic the pancreas’s natural production. It’s essential for controlling blood sugar, preventing complications, and keeping individuals with Type 1 Diabetes healthy.
Types of Insulin
There are various types of insulin, each with unique onset and duration. Knowing these differences is vital for creating an effective insulin plan.
Rapid-Acting Insulin
Rapid-acting insulin starts working within 15 minutes, peaks in about 1 hour, and lasts 2 to 4 hours. It’s taken before meals to manage blood sugar spikes after eating.
Long-Acting Insulin
Long-acting insulin has a minimal peak and maintains steady activity for 20-42 hours. It provides background insulin throughout the day or night.
Intermediate and Mixed Insulins
Intermediate-acting insulin starts in 1 to 2 hours, peaks in 4 to 12 hours, and lasts 12 to 18 hours. Mixed insulins combine different types for quick onset and longer action.
Delivery Methods
The method of insulin delivery greatly affects therapy effectiveness. Various devices cater to different needs and preferences.
Insulin Pens
Insulin pens are portable, prefilled, and convenient. They’re ideal for those needing multiple daily injections.
Insulin Pumps
Insulin pumps deliver insulin continuously throughout the day. They can be programmed for bolus doses at meals, providing flexibility and precision.
Smart Insulin Delivery Systems
Smart insulin systems combine continuous glucose monitoring with insulin pumps. They automatically adjust insulin based on real-time glucose levels. This represents a major leap in Type 1 Diabetes management.
Dosing and Timing Strategies
Choosing the right dose and timing of insulin is key to good blood sugar control. Meal composition, physical activity, and current blood glucose levels influence insulin doses.
Understanding insulin therapy basics, including types, delivery methods, and dosing, helps individuals with Type 1 Diabetes manage their condition better. This improves their quality of life.
Blood Glucose Monitoring
Blood glucose monitoring is essential for managing Type 1 Diabetes. It allows individuals to adjust their insulin, diet, and exercise. This monitoring keeps blood glucose levels in check, lowering the risk of diabetes complications.
Traditional Fingerstick Methods
Fingerstick blood glucose monitoring involves pricking the finger to get a blood sample. This sample is then analyzed with a glucometer. Despite its widespread use, this method has drawbacks. It can be painful and may yield inaccurate results if not done correctly.
- Requires lancets and test strips
- Provides immediate blood glucose reading
- Can be inconvenient for frequent testing
Continuous Glucose Monitoring (CGM)
Continuous Glucose Monitoring (CGM) is an alternative to traditional methods. CGM uses a small sensor under the skin to track glucose levels continuously, day and night.
How CGM Works
CGM systems have a tiny sensor inserted under the skin to measure glucose. This sensor connects to a transmitter, sending data to a receiver or a smartphone app. It offers real-time glucose readings.
Benefits and Limitations
CGM reduces the need for fingerstick testing and provides detailed glucose data. It also alerts users to high or low glucose levels. Yet, CGM can be pricey, and some may experience skin irritation or inaccuracies in glucose readings.
Insurance Coverage
Insurance coverage for CGM varies by provider and policy. Many plans cover CGM for Type 1 Diabetes, mainly for those with frequent hypoglycemic events or trouble reaching target glucose ranges.

Target Ranges and Data Interpretation
Understanding target glucose ranges and interpreting monitoring data is key to managing diabetes. Target ranges vary but generally include fasting glucose of 70-130 mg/dL and postprandial levels under 180 mg/dL.
- Review glucose data regularly
- Adjust insulin doses based on glucose trends
- Identify patterns of hypo/hyperglycemia
Nutrition Management for Type 1 Diabetes
For those with Type 1 Diabetes, grasping the nuances of nutrition management is essential. It’s the key to maintaining stable blood sugar levels. Effective nutrition planning is vital for optimal glucose control and reducing diabetes-related complications.
Carbohydrate Counting
Carbohydrate counting is a meal planning method that focuses on carb intake. It’s critical for Type 1 Diabetes management, as it directly affects blood glucose levels.
Insulin-to-Carb Ratios
Understanding insulin-to-carb ratios is key for calculating the right insulin dose based on carbs. These ratios differ among individuals and can evolve over time, necessitating ongoing monitoring and adjustments.
Reading Food Labels
Accurate reading of food labels is vital for carbohydrate counting. It involves grasping serving sizes, total carb content, and recognizing hidden sugars in processed foods.
Glycemic Index and Load
The glycemic index (GI) measures how quickly foods raise blood sugar. Foods with a low GI digest slowly, leading to a gradual blood sugar increase. Glycemic load (GL) considers both GI and carb amount in a serving, giving a fuller picture of a food’s blood glucose impact.
Meal Planning Strategies
Effective meal planning is critical for Type 1 Diabetes management. It involves balancing carb intake with insulin dosing and considering food glycemic index.
Balanced Plate Method
The balanced plate method divides your plate into sections: half for veggies, a quarter for protein, and a quarter for carbs. This method helps in achieving a balanced meal that supports blood glucose control.
Timing of Meals
The timing of meals and snacks is key for stable blood glucose levels. It’s important to align meal times with insulin dosing to avoid hypoglycemia or hyperglycemia.
By adopting these nutrition management strategies, individuals with Type 1 Diabetes can better control their blood glucose. This improvement enhances their overall quality of life.
Exercise and Physical Activity Guidelines
For those with Type 1 Diabetes, adding exercise to their daily life can bring significant health benefits. Regular physical activity boosts cardiovascular health and insulin sensitivity. It also improves overall well-being.
Benefits of Regular Exercise
Regular exercise greatly enhances the lives of those with Type 1 Diabetes. It leads to better glycemic control, improved cardiovascular health, and enhanced mental well-being. Exercise also aids in weight management and increases muscle strength.
Managing Blood Sugar During Activity
It’s vital to manage blood sugar levels during exercise to avoid hyperglycemia and hypoglycemia. Knowing how different exercises affect blood glucose is essential for effective management.
Pre-Exercise Strategies
Before starting any exercise, it’s important to check blood glucose levels. Adjusting insulin doses or consuming carbohydrates beforehand can prevent hypoglycemia. Proper planning is critical, more so for intense or long activities.
Post-Exercise Adjustments
After exercising, it’s necessary to monitor blood glucose levels to see if adjustments are needed. Post-exercise hypoglycemia can happen hours later, so ongoing monitoring is key. Adjusting food intake or insulin dosing may be necessary to keep blood glucose stable.
Sports and Competitive Athletics
Individuals with Type 1 Diabetes can engage in sports and competitive athletics with the right planning and management. It’s important to understand how to adjust insulin regimens and nutrition plans based on the activity’s demands. Many athletes with Type 1 Diabetes compete at high levels, showing that diabetes doesn’t limit athletic achievement.
By taking a proactive stance on exercise and physical activity, individuals with Type 1 Diabetes can enjoy the benefits of being active while effectively managing their blood sugar levels.
Preventing and Managing Complications
Complications from Type 1 Diabetes can be severe, but with proper management, many can be prevented or delayed. Understanding both short-term and long-term complications is key. Taking proactive steps is essential to mitigate them.
Short-term Complications
Short-term complications include hypoglycemia and hyperglycemia, both serious if not managed promptly.
Hypoglycemia
Hypoglycemia, or low blood sugar, occurs when glucose levels drop below normal. Symptoms include shakiness, sweating, and confusion. Prompt treatment with glucose or glucagon is essential to prevent severe outcomes.
Hyperglycemia
Hyperglycemia, or high blood sugar, results from insufficient insulin or insulin resistance. It can lead to diabetic ketoacidosis (DKA), a potentially life-threatening condition. Recognizing symptoms early and adjusting insulin doses can help manage hyperglycemia.
Long-term Health Risks
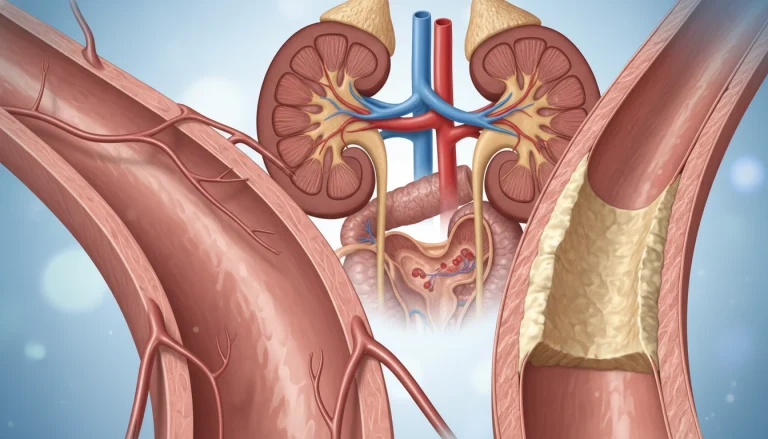
Long-term complications of Type 1 Diabetes can affect various body systems, leading to microvascular and macrovascular complications.
Microvascular Complications
Microvascular complications include diabetic retinopathy, nephropathy, and neuropathy. Regular monitoring and maintaining tight blood glucose control can reduce the risk of these complications.
Macrovascular Complications
Macrovascular complications involve the larger blood vessels and can lead to cardiovascular disease, including heart attacks and strokes. Managing risk factors such as hypertension and high cholesterol is critical.

Regular Screening and Prevention
Regular screening for complications is a critical aspect of Type 1 Diabetes management. Annual check-ups with healthcare providers, including eye exams and kidney function tests, can help detect issues early. Preventive measures, such as maintaining a healthy diet and exercising regularly, also play a key role in managing the disease.
By understanding the complications and taking proactive steps, individuals with Type 1 Diabetes can lead active and fulfilling lives.
Living Well with Type 1 Diabetes
Managing Type 1 Diabetes demands a holistic approach, integrating medical care with mental and emotional health. A successful strategy includes insulin therapy, lifestyle adjustments, and psychological support. This approach ensures a balanced management of the condition.
Mental Health Considerations
The mental health impact of Type 1 Diabetes is significant. The constant monitoring of blood glucose, insulin administration, and maintaining a healthy lifestyle can be overwhelming. These tasks contribute to stress and emotional strain.
Diabetes Distress
Diabetes distress is a common issue, where individuals feel overwhelmed by diabetes management. It can cause frustration, anxiety, and burnout. This distress is a major concern for those living with Type 1 Diabetes.
Coping Strategies
Developing effective coping strategies is essential for managing diabetes distress. Mindfulness, meditation, and cognitive-behavioral therapy are valuable tools. They help individuals manage stress and enhance their mental well-being.
Building a Support System
A strong support system is critical for those with Type 1 Diabetes. This includes family, friends, healthcare providers, and support groups. Such a network provides emotional support, practical assistance, and a sense of community.
This support significantly enhances an individual’s ability to manage their condition effectively. It offers a sense of security and understanding.
Navigating Social Situations
Managing social situations with Type 1 Diabetes can be challenging. It requires careful planning and awareness of one’s needs.
Alcohol and Diabetes
For individuals with Type 1 Diabetes, alcohol consumption must be carefully managed. It’s important to monitor blood glucose levels closely and adjust insulin doses as needed. This ensures safety and prevents complications.
Dining Out
Dining out can be difficult due to the unpredictability of food content and portion sizes. Planning ahead, choosing familiar foods, and communicating with restaurant staff can help manage these challenges. This approach ensures a safe and enjoyable dining experience.
Special Considerations Across Life Stages
Type 1 Diabetes brings unique challenges at different life stages, demanding personalized management strategies. As people grow, their needs and situations evolve, necessitating adjustments in their care plans.
Children and Adolescents with Type 1 Diabetes
Managing Type 1 Diabetes in kids and teens requires addressing their specific needs, from diet to mental health support. Effective management in these critical years is vital for their health now and in the future.
School Management Plans
Creating a detailed school management plan is key for kids with Type 1 Diabetes. It should outline blood glucose monitoring, insulin administration, and handling low blood sugar, ensuring school staff can support the child’s needs.
Developmental Considerations
As children grow, their diabetes management evolves. It’s vital to consider their developmental stages when planning care. Adjusting insulin and monitoring strategies is necessary to accommodate growth and lifestyle changes.
Pregnancy and Diabetes Management
For women with Type 1 Diabetes, pregnancy demands careful planning and management to safeguard the health of both mother and baby. Pre-pregnancy planning and close monitoring during pregnancy are essential for effective diabetes care.
Preconception Planning
Preconception planning involves optimizing blood glucose control to reduce risks. This includes reviewing medications, planning diets, and discussing pregnancy-related risks with healthcare providers.
Monitoring During Pregnancy
During pregnancy, it’s critical to monitor blood glucose levels closely to maintain tight control. This may involve more frequent glucose checks and adjusting insulin dosing to meet pregnancy’s changing needs.
Aging with Type 1 Diabetes
As individuals with Type 1 Diabetes age, they may encounter new challenges, including complications and the impact of aging on diabetes management. Regular health checks and adapting their care plan can help manage these challenges.
Advances in Type 1 Diabetes Research
Innovative research is reshaping the future of Type 1 Diabetes management. Studies and technological breakthroughs are unveiling new insights and tools for those affected. This progress is a beacon of hope for a better tomorrow.
Artificial Pancreas Technology
Artificial pancreas technology marks a major leap in Type 1 Diabetes care. It automates insulin delivery, monitoring glucose levels and adjusting insulin doses continuously. Research indicates that it can enhance glycemic control and lower hypoglycemia risks.

Immunotherapy Approaches
Immunotherapy seeks to alter the immune system’s response to prevent it from attacking the pancreas. The focus is on developing vaccines and therapies to potentially halt or reverse Type 1 Diabetes progression.
Stem Cell Research
Stem cell research holds out hope for regenerating or replacing damaged pancreatic cells. Scientists are working to use stem cells to restore insulin production in Type 1 Diabetes patients. Though experimental, this research could lead to a cure in the future.
These breakthroughs in Type 1 Diabetes research are setting the stage for more effective management and potentially life-changing treatments. As research advances, we can expect significant improvements in care and outcomes for those with Type 1 Diabetes.
Resources and Support for Your Diabetes Journey
Managing Type 1 Diabetes is a lifelong journey that requires access to reliable resources and support. Individuals with this condition can benefit from various diabetes resources. These include educational materials, support groups, and online forums.
The American Diabetes Association (ADA) is a prominent organization that offers extensive information on diabetes management. This includes nutrition planning, exercise guidelines, and blood glucose monitoring. The ADA also provides resources for families and caregivers. They help navigate the challenges of supporting a loved one with Type 1 Diabetes.
Support for diabetes is also available through online communities and local support groups. Here, individuals can share their experiences, ask questions, and receive guidance from others who understand the condition. These networks play a vital role in helping people with Type 1 Diabetes stay informed and motivated.
By leveraging these diabetes resources and support networks, individuals can better manage their condition. They can improve their quality of life and stay up-to-date with the latest research and advancements in diabetes care.
FAQ
Q: What is Type 1 Diabetes?
A: Type 1 Diabetes is a chronic autoimmune condition. It occurs when the pancreas fails to produce enough insulin. Insulin is essential for glucose to enter cells and provide energy.
Q: What are the symptoms of Type 1 Diabetes?
A: Symptoms include frequent urination, increased thirst, and hunger. Other signs are fatigue, blurred vision, and slow healing of cuts and wounds.
Q: How is Type 1 Diabetes diagnosed?
A: Diagnosis involves blood tests. These include fasting plasma glucose, antibody testing, and A1C testing. They assess blood glucose levels and autoimmune antibodies.
Q: What is the difference between Type 1 and Type 2 Diabetes?
A: Type 1 Diabetes is an autoimmune condition where the body doesn’t produce insulin. Type 2 Diabetes is characterized by insulin resistance and impaired insulin secretion. It’s often linked to lifestyle factors.
Q: How is Type 1 Diabetes managed?
A: Management includes insulin therapy through various methods. This includes insulin pens, pumps, or smart delivery systems. It also involves blood glucose monitoring and lifestyle adjustments. These include nutrition management and regular physical activity.
Q: What are the risks associated with Type 1 Diabetes?
A: Risks include short-term complications like hypoglycemia and hyperglycemia. Long-term complications include microvascular and macrovascular issues. Examples are diabetic retinopathy, nephropathy, and cardiovascular disease.
Q: Can Type 1 Diabetes be prevented?
A: Currently, there’s no known prevention for Type 1 Diabetes. Research into genetic predisposition, environmental triggers, and interventions is ongoing.
Q: How does Type 1 Diabetes affect mental health?
A: Living with Type 1 Diabetes can impact mental health. It can lead to diabetes distress, anxiety, and depression. This highlights the need for coping strategies and support systems.
Q: What are the latest advancements in Type 1 Diabetes research?
A: Advances include artificial pancreas technology and immunotherapy. These aim to halt autoimmune destruction of beta cells. Stem cell research is also underway for insulin-producing cell regeneration.
Q: Where can I find resources and support for managing Type 1 Diabetes?
A: Resources include diabetes organizations, support groups, and educational materials. Healthcare providers specializing in diabetes care offer valuable guidance and community support.