Type 2 Diabetes: What Is Type 2 Diabetes?
Living with Type 2 Diabetes poses significant challenges, yet the right strategies can help manage symptoms and boost well-being. This condition impacts millions globally, affecting daily life profoundly. Managing Type 2 Diabetes effectively requires a blend of lifestyle adjustments, medication, and continuous monitoring. Grasping the condition and proactively addressing it can lower the risk of complications. This approach enhances one’s quality of life.
Improving well-being is central to managing this condition. By focusing on symptom management and adopting a healthy lifestyle, individuals can regain control over their health. This leads to a more fulfilling life. Type 2 diabetes is a chronic condition affecting millions globally. It’s vital to grasp its definition and implications for effective management. This metabolic disorder is marked by high blood sugar, insulin resistance, and impaired insulin secretion.
Definition and Prevalence in the United States
Type 2 diabetes is the most prevalent form, making up about 90% of diabetes cases. In the U.S., over 34 million people live with diabetes, with many undiagnosed. Factors like obesity, lack of physical activity, and unhealthy diets contribute to its prevalence. For those managing their weight, regional weight loss programs can offer support.
How Type 2 Differs from Type 1 and Gestational Diabetes
Type 2 diabetes contrasts sharply with Type 1, an autoimmune disease where the immune system attacks insulin-producing cells. Gestational diabetes emerges during pregnancy, caused by hormonal changes and insulin resistance. Recognizing these distinctions is essential for accurate diagnosis and treatment.
The Progressive Nature of the Condition
Type 2 diabetes progresses if not managed, worsening over time. Initially, the pancreas overproduces insulin to counteract insulin resistance. Eventually, it fails to meet the demand, resulting in elevated blood sugar levels. Early intervention and management are critical to slow this progression and avert complications.
The Science Behind Blood Sugar Regulation
Understanding how the body regulates blood sugar is key to managing Type 2 Diabetes. This process involves the teamwork of various organs and hormones. It’s a complex task.
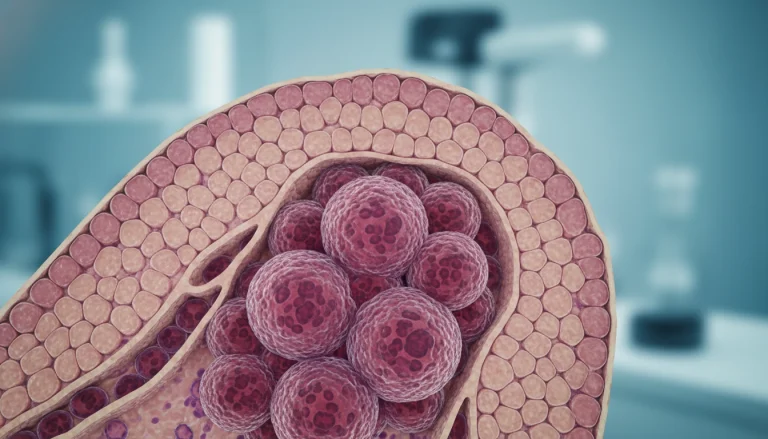
Insulin Resistance Explained
Insulin resistance occurs when the body’s cells don’t respond well to insulin. Insulin is a hormone from the pancreas that controls blood sugar. Without effective insulin action, glucose builds up in the blood.
This condition is a major factor in Type 2 Diabetes. It’s linked to obesity, lack of exercise, and a diet rich in saturated fats and sugars. Improving insulin resistance can be achieved through weight loss, more exercise, and better diet choices.
Beta Cell Dysfunction
Beta cells in the pancreas make insulin. In Type 2 Diabetes, these cells don’t work right, leading to less insulin. At first, the pancreas tries to keep up by making more insulin. But eventually, the beta cells get tired and can’t produce enough insulin.
Metabolic Mechanisms and Glucose Pathways
The ways our body handles glucose are complex. Glucose comes from carbs and gets into the blood. Then, insulin helps move glucose into cells, like the liver, muscles, and fat.
In Type 2 Diabetes, these pathways get disrupted, causing high blood sugar. Knowing how these mechanisms work is vital for finding treatments that address insulin resistance, beta cell issues, and glucose handling.
Risk Factors for Type 2 Diabetes
Type 2 Diabetes risk is shaped by genetics, lifestyle, and environment. Knowing these factors helps individuals prevent the disease and seek timely diagnosis and treatment.
Genetic Predisposition
Genetics significantly influence Type 2 Diabetes development. Those with a family history are more prone to it.
Lifestyle Contributors
Lifestyle choices greatly impact Type 2 Diabetes risk. Diet and physical activity levels are key contributors.
Diet and Nutrition
A diet rich in processed foods, sugars, and unhealthy fats raises Type 2 Diabetes risk. Important dietary factors include:
- High consumption of sugary beverages
- Frequent intake of refined grains
- Low intake of fiber-rich foods
Physical Inactivity
Physical inactivity is a major risk factor. Regular exercise helps manage blood sugar and maintain weight.
Physical activity offers several benefits, such as:
- Improved insulin sensitivity
- Enhanced glucose uptake by muscles
- Better overall cardiovascular health
Age, Ethnicity, and Other Unmodifiable Factors
Age, ethnicity, and certain unchangeable factors also influence Type 2 Diabetes risk. These include:
Specifically:
- Risk increases after the age of 45
- Certain ethnic groups are at higher risk, including African Americans, Hispanics/Latinos, and American Indians
- History of gestational diabetes or polycystic ovary syndrome (PCOS) also increases risk

Recognizing the Warning Signs
The symptoms of Type 2 Diabetes can be subtle, but knowing what to look for can make a significant difference. Early detection is key to managing the condition effectively.
Common Symptoms
Type 2 Diabetes often presents with mild symptoms that can be easily overlooked. Common symptoms include:
- Increased thirst and urination
- Fatigue
- Blurred vision
- Slow healing of cuts and wounds
- Frequent infections
When to See a Doctor
If you’re experiencing several of these symptoms, it’s vital to consult a healthcare professional. Early diagnosis can significantly impact the management of Type 2 Diabetes.
Prediabetes: The Warning Stage
Prediabetes is a condition where blood sugar levels are higher than normal but not high enough to be classified as diabetes. It’s a warning sign that Type 2 Diabetes could develop.
Reversing Prediabetes
Fortunately, prediabetes can often be reversed through lifestyle changes. These include:
- Adopting a healthier diet
- Increasing physical activity
- Losing weight if necessary
Diagnosis and Testing Methods
Accurate diagnosis of Type 2 Diabetes is essential for effective management. Several testing methods are employed to achieve this. These tests assess blood glucose levels, providing insights into the body’s glucose regulation.
A1C Test Explained
The A1C test is a key diagnostic tool. It measures average blood glucose levels over 2-3 months. This is done by assessing glucose bound to hemoglobin in red blood cells. An A1C level of 6.5% or higher indicates diabetes.
Fasting Blood Glucose and Oral Glucose Tolerance Tests
Alongside the A1C test, fasting blood glucose (FBG) and oral glucose tolerance tests (OGTT) are used. The FBG test measures glucose after an overnight fast. The OGTT evaluates how well the body regulates glucose after a sugary drink.
Interpreting Your Test Results
Understanding test results is vital for diagnosis. For the A1C test, a level below 5.7% is normal, 5.7% to 6.4% indicates prediabetes, and 6.5% or higher suggests diabetes. For FBG, a level of 126 mg/dL or higher is diagnostic of diabetes.
Screening Recommendations by Age and Risk
Screening recommendations vary by age, risk factors, and health conditions. Adults aged 45 and older should be screened for Type 2 Diabetes. Earlier screening is advised for those with risk factors like obesity, family history, or physical inactivity.
Medication Options for Blood Sugar Control
Managing Type 2 Diabetes requires effective blood sugar control. Various medications are available to help achieve this goal. The choice of medication depends on several factors. These include the patient’s health status, the presence of other medical conditions, and the specific characteristics of the medication.
Oral Medications: Types and Functions
Oral medications are often the first line of treatment for Type 2 Diabetes. They work through different mechanisms to help lower blood glucose levels.
Metformin as First-Line Treatment
Metformin is commonly prescribed as the initial medication for Type 2 Diabetes. It is effective in lowering glucose production by the liver and improving insulin sensitivity.
Other Medication Classes
Other classes of oral medications include sulfonylureas, which stimulate insulin release. DPP-4 inhibitors help the body produce more insulin and reduce glucose production. SGLT2 inhibitors prevent the kidneys from reabsorbing glucose back into the blood.
Injectable Medications Beyond Insulin
For some patients, injectable medications beyond insulin may be prescribed. GLP-1 receptor agonists help lower blood sugar. They enhance insulin secretion, suppress glucagon release, and slow gastric emptying.
Insulin Therapy: When and How It’s Used
Insulin therapy may be recommended for patients with Type 2 Diabetes when other treatments are not sufficient. It involves administering insulin via injection or pump. This helps glucose enter the cells.
Emerging Drug Treatments
Research is ongoing into new and emerging treatments for Type 2 Diabetes. Novel oral and injectable medications target different aspects of the disease process.
Nutritional Strategies for Managing Type 2 Diabetes
Managing Type 2 Diabetes effectively requires a holistic nutritional approach. A well-planned diet helps keep blood sugar levels in check. This improves health and lowers the risk of complications.
Carbohydrate Counting and Glycemic Index
Carbohydrate counting is key for managing Type 2 Diabetes. It tracks carbs at each meal to control blood glucose. The glycemic index (GI) ranks foods by their blood sugar impact. Foods with a low GI digest slowly, causing gradual blood glucose increases.
Knowing the GI of different foods aids in making better choices. Whole grains, non-starchy veggies, and most fruits have low GI. In contrast, white bread, sugary snacks, and some fruits like watermelon have high GI.
Meal Planning and Portion Control
Meal planning is critical for stable blood sugar levels. It involves a balanced diet rich in nutrient-dense foods. Portion control is also essential, ensuring food amounts support a healthy weight and blood glucose.
Using measuring cups or a food scale helps gauge portion sizes accurately. Regular, spaced meals and snacks also aid in blood sugar management.
Beneficial Foods and Eating Patterns
Choosing a healthy eating pattern significantly impacts Type 2 Diabetes management. Certain diets are more beneficial.
Mediterranean Diet Approach
The Mediterranean diet focuses on whole grains, fruits, veggies, lean proteins, and healthy fats like olive oil. It’s linked to better blood sugar control and heart health.
Plant-Based Options
Plant-based diets, rich in plant-derived foods, are also beneficial. They’re high in fiber, vitamins, and minerals, and low in saturated fats. This diet improves insulin sensitivity and overall health.
Foods to Limit or Avoid
Some foods can harm blood sugar control and health. It’s wise to limit or avoid sugary drinks, refined grains, and foods high in saturated and trans fats. These can cause blood glucose spikes, leading to weight gain and heart disease risk.
By adopting these nutritional strategies, individuals with Type 2 Diabetes can manage their condition better. This improves their overall well-being.
The Critical Role of Exercise
Regular physical activity is a cornerstone in managing Type 2 Diabetes. It not only controls blood glucose levels but also boosts overall health and well-being.
How Physical Activity Affects Blood Glucose
Physical activity directly impacts blood glucose levels. When you exercise, your muscles use glucose for energy, lowering blood glucose. Regular exercise also enhances insulin sensitivity, making it easier for glucose to enter cells.
Recommended Exercise Types and Duration
The American Diabetes Association suggests at least 150 minutes of moderate-intensity aerobic exercise weekly. This should be spread over at least three days. Incorporating strength training on two or more days a week can also improve glucose control.
Aerobic Exercise Benefits
Aerobic exercises, like walking, cycling, or swimming, boost cardiovascular health and increase insulin sensitivity. These activities help lower blood glucose levels and enhance overall fitness.
Strength Training Importance
Strength training, including weightlifting or resistance band exercises, builds muscle mass and boosts insulin sensitivity. This type of exercise is vital for metabolic health.
Starting Safely: Exercise Precautions
Before starting any new exercise, consult your healthcare provider, even with no underlying health conditions. Monitoring blood glucose levels before, during, and after exercise is key to preventing hypoglycemia or hyperglycemia.
Weight Management Approaches
Weight management is key to managing Type 2 Diabetes. It can greatly affect blood glucose levels, leading to better health outcomes.
Impact on Blood Glucose
Reducing weight, mainly around the belly, boosts insulin sensitivity. This lowers blood glucose levels. Research indicates that losing 5-10% of initial body weight can significantly improve glycemic control.

Sustainable Weight Management
Effective weight management requires long-term lifestyle changes, not quick fixes. It involves dietary adjustments, more physical activity, and behavioral shifts.
- Eating a balanced diet with lots of vegetables, fruits, and whole grains.
- Staying active through activities like walking or swimming.
- Controlling portion sizes to avoid overeating.
Considering Bariatric Surgery
Bariatric surgery is an option for some to lose a lot of weight. This surgery can lead to significant weight loss and lower blood glucose levels.
Maintaining Long-term Success
Staying motivated is essential for long-term weight management success. Setting realistic goals, tracking progress, and getting support from healthcare professionals or support groups are key strategies.
- Set achievable weight loss goals.
- Regularly track weight and measurements.
- Engage with a support group for ongoing motivation.
By using these strategies, individuals with Type 2 Diabetes can maintain a healthy weight. This improves their overall health and reduces the risk of complications.
Monitoring Blood Glucose Effectively
For those with type 2 diabetes, monitoring blood glucose is essential for health. Regular checks reveal how diet, exercise, and meds affect glucose levels.
Traditional Testing vs. Continuous Glucose Monitoring
There are two main ways to monitor blood glucose: traditional testing and continuous glucose monitoring (CGM). Traditional testing uses a glucometer to check levels by pricking a finger.
CGM systems, in contrast, offer real-time data all day and night. They track glucose continuously, helping spot patterns and trends missed by traditional methods.
Understanding Your Numbers
Knowing what your blood glucose numbers mean is vital for managing diabetes. The American Diabetes Association suggests these target ranges:
- Before meals: 80-130 mg/dL
- After meals (peak): <180 mg/dL
These targets can change based on age, health, and how long you’ve had diabetes.
Tracking Patterns and Making Adjustments
Tracking blood glucose patterns helps make better diabetes care choices. By analyzing these patterns, you can see when to tweak diet, exercise, or meds.
For example, if morning glucose is often high, it might be time to adjust evening meds or snacks.
Technology Tools for Diabetes Management
Technology has greatly improved diabetes care, with tools beyond CGM systems. These include:
- Mobile apps for tracking glucose, meds, and diet
- Smart insulin pens that log doses
- Telehealth for remote doctor visits
These tools help manage diabetes better, providing insights and support.
Preventing and Managing Complications
Managing Type 2 Diabetes effectively means focusing on preventing complications that can severely impact one’s quality of life. While controlling blood sugar levels is vital, it’s equally critical to address the complications that can arise from the condition.
Cardiovascular Disease Risk Reduction
Those with Type 2 Diabetes face a higher risk of cardiovascular disease. To manage this risk, it’s essential to maintain healthy blood pressure and cholesterol levels. Regular physical activity and a balanced diet also play a significant role.
- Monitor blood pressure regularly
- Maintain a healthy lipid profile
- Engage in regular physical activity
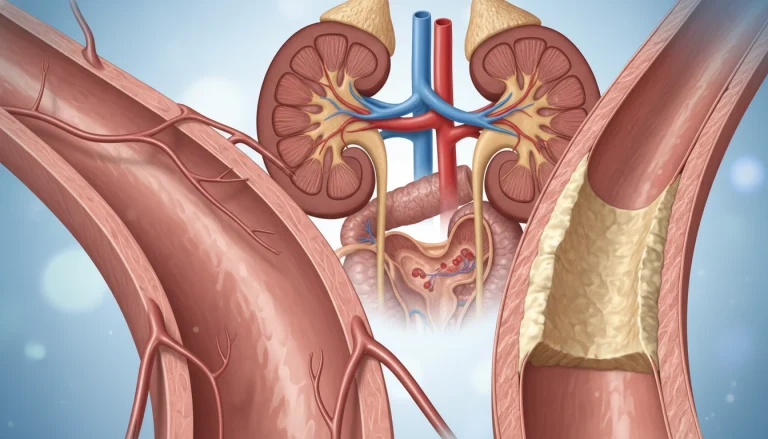
Protecting Kidney Function
Type 2 Diabetes can lead to diabetic nephropathy, a major cause of chronic kidney disease. To protect kidney function, it’s important to control blood sugar and blood pressure levels. Regular monitoring of kidney function is also necessary.
- Control blood sugar levels
- Manage blood pressure
- Have regular kidney function tests
Eye Health and Vision Preservation
Diabetic retinopathy poses a significant risk for those with Type 2 Diabetes, potentially causing vision loss. Regular eye exams and controlling blood sugar levels are key to preserving vision.
Nerve Damage and Foot Care
Nerve damage (neuropathy) can result from prolonged high blood sugar levels, affecting sensation in the feet. Proper foot care is essential to prevent complications such as ulcers.
Daily Foot Inspection Routine
Inspecting your feet daily for any signs of damage or infection is critical. Look for cuts, blisters, redness, or swelling.
When to Seek Medical Attention
If you notice any signs of infection or damage, or if you experience pain or numbness, seek medical attention promptly.
Mental Health and Diabetes Distress
Managing Type 2 Diabetes goes beyond just controlling blood sugar levels. It also involves dealing with the mental strain it brings. The constant need to monitor and manage the condition can lead to burnout, anxiety, and depression.
Recognizing Depression and Anxiety
It’s vital to recognize the signs of depression and anxiety in those with Type 2 Diabetes. Symptoms include persistent sadness, loss of interest in activities, changes in appetite, and trouble sleeping. Anxiety shows as worry, restlessness, or feeling constantly on edge.

Coping Strategies and Support
Coping with the mental health aspects of Type 2 Diabetes requires a multi-faceted approach. This includes:
- Seeking support from family, friends, or support groups
- Practicing stress-reducing techniques such as meditation or yoga
- Engaging in regular physical activity
- Maintaining a healthy diet
When to Seek Professional Help
If feelings of depression or anxiety persist, seeking professional help is essential. Mental health professionals can offer strategies and therapies tailored to the individual’s needs. They help cope with diabetes distress.
Building Resilience with Chronic Illness
Building resilience is critical in managing the mental health challenges of Type 2 Diabetes. It involves developing coping skills, setting realistic goals, and maintaining a positive outlook. By doing so, individuals can better navigate their condition’s complexities.
Building Your Diabetes Care Team
Managing type 2 diabetes effectively requires a skilled and collaborative care team. A well-structured team offers complete care, better treatment outcomes, and a higher quality of life for those with diabetes.
Essential Healthcare Providers
A diabetes care team includes several critical healthcare professionals. These are:
- Primary care physicians who oversee overall health
- Endocrinologists who specialize in diabetes care
- Registered dietitians who provide nutritional guidance
- Certified diabetes educators who offer valuable insights into managing the condition
Working Effectively with Your Team
To maximize your diabetes care team’s benefits, open and honest communication is key. This means:
- Sharing your health goals and concerns
- Asking questions about your treatment plan
- Reporting any changes in your condition or symptoms
Self-Advocacy in Healthcare Settings
Being an active participant in your care is vital. This involves understanding your treatment options, knowing your rights as a patient, and seeking a second opinion when needed.
Insurance Navigation and Resource Access
Navigating insurance coverage and accessing resources can be daunting. Your care team can guide you through your benefits and connect you with support services, such as:
- Diabetes support groups
- Educational programs
- Financial assistance programs
Empowering Your Journey with Type 2 Diabetes
Managing Type 2 Diabetes effectively requires a proactive and informed approach. Understanding the condition, its risk factors, and management strategies empowers individuals. This knowledge allows them to take control of their Type 2 Diabetes journey.
A healthy lifestyle is key, including a balanced diet and regular physical activity. These habits can significantly impact blood sugar levels. Nutritional strategies, such as carbohydrate counting and meal planning, are also critical in managing the condition.
Monitoring blood glucose levels and adjusting treatment plans is vital. With the right tools and support, individuals can navigate Type 2 Diabetes challenges. This improves their overall well-being.
Staying informed and working closely with healthcare providers is essential. Individuals can develop a personalized plan for managing Type 2 Diabetes. This enhances their quality of life and empowers their journey with the condition.
FAQ
Q: What is Type 2 Diabetes?
A: Type 2 Diabetes is a chronic condition affecting how the body processes blood sugar (glucose). It’s marked by insulin resistance, where cells don’t respond well to insulin, and impaired insulin secretion.
Q: What are the risk factors for developing Type 2 Diabetes?
A: Risk factors include genetic predisposition, obesity, and a sedentary lifestyle. A diet rich in saturated fats and sugar, age over 45, certain ethnicities, and a history of gestational diabetes or delivering a baby over 4 kg also increase risk.
Q: How is Type 2 Diabetes diagnosed?
A: Diagnosis often involves the A1C test, fasting blood glucose test, or oral glucose tolerance test. An A1C level of 6.5% or higher, a fasting glucose level of 126 mg/dL or higher, or a 2-hour glucose level of 200 mg/dL or higher during an oral glucose tolerance test indicates diabetes.
Q: Can Type 2 Diabetes be reversed?
A: While Type 2 Diabetes cannot be “cured,” it can be managed and sometimes reversed through significant lifestyle changes. These include weight loss, dietary changes, and increased physical activity. Prediabetes, a precursor to Type 2 Diabetes, can often be reversed with these interventions.
Q: What are the common symptoms of Type 2 Diabetes?
A: Common symptoms include increased thirst and urination, fatigue, blurred vision, slow healing of cuts and wounds, and frequent infections. Some people may not experience noticeable symptoms, even in the early stages.
Q: How does diet affect Type 2 Diabetes management?
A: Diet is key in managing Type 2 Diabetes. A balanced diet low in saturated fats, added sugars, and salt, and high in fiber, fruits, and vegetables helps control blood sugar levels. Carbohydrate counting and understanding the glycemic index of foods can also be beneficial.
Q: What is the role of exercise in managing Type 2 Diabetes?
A: Regular physical activity lowers blood sugar levels, improves insulin sensitivity, and aids in weight loss. Both aerobic exercise and strength training are recommended, aiming for at least 150 minutes of moderate-intensity aerobic exercise per week.
Q: How often should I monitor my blood glucose levels?
A: Blood glucose monitoring frequency varies based on the individual’s treatment plan and diabetes management type. Those using insulin may need to monitor more frequently, while diet and exercise management may require less frequent monitoring.
Q: What are the possible complications of Type 2 Diabetes?
A: Complications include cardiovascular disease, kidney damage (nephropathy), eye damage (retinopathy), nerve damage (neuropathy), and foot damage. Managing blood sugar levels and other risk factors can help prevent or delay these complications.
Q: How can I manage stress and mental health with Type 2 Diabetes?
A: Managing stress and maintaining good mental health is essential. Techniques like mindfulness, meditation, and yoga can help reduce stress. Seeking support from healthcare professionals, support groups, and loved ones is also important for overall well-being.