Ulcer: What Is an Ulcer?
An ulcer is a sore that forms on the skin or mucous membranes, leading to discomfort and pain. There are various types, such as peptic ulcers in the stomach or duodenum, and skin ulcers due to poor circulation or pressure. The symptoms and causes of ulcers differ by type. Common signs include pain, bleeding, and inflammation. Treatments range from medications that lower stomach acid to dressings and therapies that aid in wound healing.
It’s vital to understand the causes, symptoms, and ulcer treatments to manage and prevent these sores. By delving into the different facets of ulcers, individuals can make informed decisions about their care and relief. The term “ulcer” refers to a specific type of sore found on the stomach or duodenum’s inside lining. Ulcers are a common health issue, causing discomfort and serious complications if untreated.
Definition and Basic Concepts
Medical Definition
An ulcer is a break in the gastrointestinal tract’s mucosal lining. It can be caused by infection, certain medications, or stress. This condition leads to pain, discomfort, and severe complications.
Common Misconceptions
Many think ulcers are caused by stress or spicy food. But, this is not entirely true. Stress can worsen it, but the main cause is usually a bacterial infection or NSAIDs.
Impact on Quality of Life
Ulcers can greatly affect one’s quality of life. They cause chronic pain, discomfort, and can lead to severe complications like bleeding or stomach perforation. Effective management and treatment are key to mitigate these effects and improve well-being.
Understanding ulcers’ definition, causes, and impact is vital for both patients and healthcare providers. It helps manage the condition effectively and prevent long-term health issues.
Types of Ulcers
Understanding the different types of ulcers is key to accurate diagnosis and treatment. Each type varies by location, symptoms, and causes. They all have distinct characteristics.
Peptic Ulcers
Peptic ulcers are common and found in the stomach or the duodenum, the small intestine’s first part.
Characteristics and Prevalence
Peptic ulcers are open sores on the stomach or duodenum lining. They’re linked to Helicobacter pylori infection or NSAID use.
Unique Features
Peptic ulcers are known for their pain in the upper abdomen. This pain often subsides with food or antacids.
Gastric Ulcers
Gastric ulcers happen in the stomach lining. They’re caused by H. pylori infection, NSAID use, or factors that harm the stomach lining.
Duodenal Ulcers
Duodenal ulcers are in the duodenum. They’re linked to H. pylori infection. They cause pain, worse when the stomach is empty.
Other Types of Ulcers
There are ulcers beyond peptic ones, affecting the GI tract’s other parts.
Esophageal Ulcers
Esophageal ulcers are in the esophagus. They’re often due to GERD or infection.
Stress Ulcers
Stress ulcers happen with severe stress, like major surgery or trauma. They can be serious if not treated quickly.
Common Causes of Ulcer
Understanding the causes of ulcers is key to effective management and treatment. Ulcers are a complex condition with multiple factors at play.
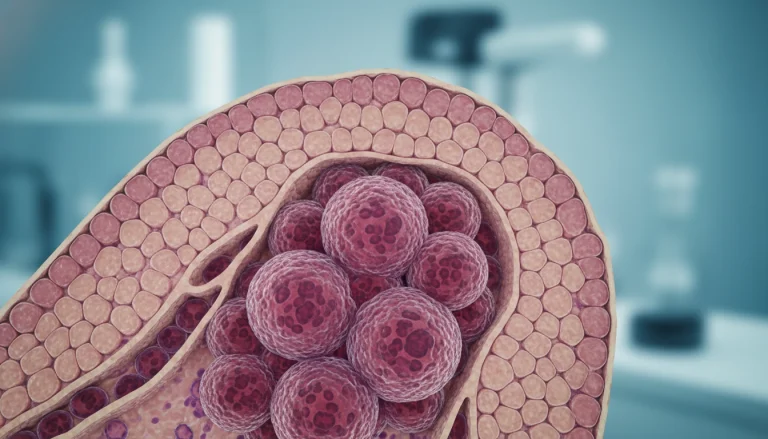
Helicobacter Pylori Infection
Helicobacter pylori (H. pylori) infection is a major cause of ulcers. This bacterium infects the stomach lining, causing inflammation and ulceration.
How H. Pylori Affects the Stomach
H. pylori infection damages the stomach lining. This makes it more susceptible to acid damage and reduces its healing ability.
Transmission and Prevalence
H. pylori infection is usually acquired in childhood. It can be spread through contaminated food or water. It’s more common in developing countries.
NSAIDs and Other Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) are another common cause of ulcers. Long-term use of NSAIDs irritates the stomach lining, leading to ulcer formation.
Stress and Lifestyle Factors
Stress and certain lifestyle factors contribute to ulcer development. Stress increases stomach acid production, worsening ulcer symptoms.
Other Contributing Factors
Other factors include smoking, excessive alcohol consumption, and a diet high in spicy or acidic foods. These can also contribute to ulcer development.
By understanding these causes, individuals can take steps to prevent ulcers and manage their symptoms effectively.
Risk Factors for Developing an Ulcer
Understanding the risk factors for ulcers is key to prevention and early treatment. Several factors can raise an individual’s risk of developing an ulcer.
Age and Gender Considerations
Age significantly impacts ulcer risk, with risks rising after 60. Men are more prone to duodenal ulcers, while gastric ulcers affect both genders more evenly.
Family History and Genetics
A family history of ulcers can elevate an individual’s risk, hinting at a genetic link. Genetic factors can influence the stomach’s ability to resist acid.
Medical Conditions That Increase Risk
Certain medical conditions, like Zollinger-Ellison syndrome, greatly increase ulcer risk. Conditions such as Crohn’s disease and liver disease also contribute to ulcer development.
Behavioral Risk Factors
Behavioral factors are critical in ulcer development. Key risk factors include:
-
-
Smoking
-
Smoking severely impairs the stomach lining’s protective abilities.
-
-
Alcohol Consumption
-
Excessive alcohol can irritate and damage the stomach lining, raising ulcer risk.
-
-
Poor Diet
-
A diet rich in spicy or fatty foods can irritate the stomach, potentially increasing ulcer risk.
By grasping these risk factors, individuals can proactively lower their ulcer risk.
Recognizing Ulcer Symptoms
It’s vital to understand the symptoms of an ulcer to seek timely medical help. Ulcers can show a range of symptoms, from mild to severe. Recognizing these signs early can greatly improve treatment outcomes.
Common Symptoms
Ulcer symptoms vary but often include specific patterns of abdominal pain and digestive issues. These symptoms can significantly impact an individual’s quality of life.
Abdominal Pain Patterns
Abdominal pain is a hallmark symptom of an ulcer. This pain is usually in the upper abdomen and can feel burning or gnawing. It may occur at night, between meals, or when the stomach is empty.
Digestive Symptoms
Besides abdominal pain, ulcers can cause digestive symptoms like nausea, vomiting, and loss of appetite. These symptoms can lead to weight loss and nutritional deficiencies if not addressed.
General Discomfort
General discomfort, including bloating and belching, can also be associated with ulcers. These symptoms can be uncomfortable and may worsen over time if the ulcer is not treated.
Warning Signs of Complications
Certain symptoms can indicate complications of an ulcer, such as bleeding or perforation. Warning signs include severe abdominal pain, vomiting blood, and black tarry stools.
Symptoms That Require Immediate Medical Attention
Seek immediate medical attention if symptoms such as severe abdominal pain, signs of bleeding (vomiting blood or black tarry stools), or difficulty breathing occur. These could be indicative of serious complications.
- Severe abdominal pain
- Vomiting blood or coffee ground-like material
- Black tarry stools
- Difficulty breathing
Diagnosing an Ulcer
To accurately diagnose an ulcer, healthcare professionals use a variety of diagnostic tools and methods. The diagnostic process is key to identifying ulcers and determining the right treatment plan.
Physical Examination and Medical History
A thorough physical examination and detailed medical history are essential initial steps in diagnosing an ulcer. Healthcare providers look for signs and symptoms that may indicate the presence of an ulcer, such as abdominal pain or tenderness.
Laboratory Tests
Laboratory tests play a vital role in diagnosing ulcers. These tests help identify the cause of the ulcer and rule out other conditions.
-
-
Blood Tests
-
Blood tests can detect the presence of Helicobacter pylori antibodies, indicating an active or past infection.
-
-
Stool Tests
-
Stool tests can identify the presence of H. pylori antigens, confirming an active infection.
-
-
Breath Tests
-
Breath tests detect carbon dioxide produced by H. pylori bacteria, indicating an active infection.
Endoscopy and Imaging Procedures
Endoscopy is a direct visualization technique that allows healthcare providers to examine the inside of the stomach and duodenum for ulcers. Imaging procedures like X-rays may also be used to identify ulcers and complications.

Differential Diagnosis
Differential diagnosis involves ruling out other conditions that may present with similar symptoms to ulcers, such as gastritis or stomach cancer. Accurate diagnosis is critical for effective treatment.
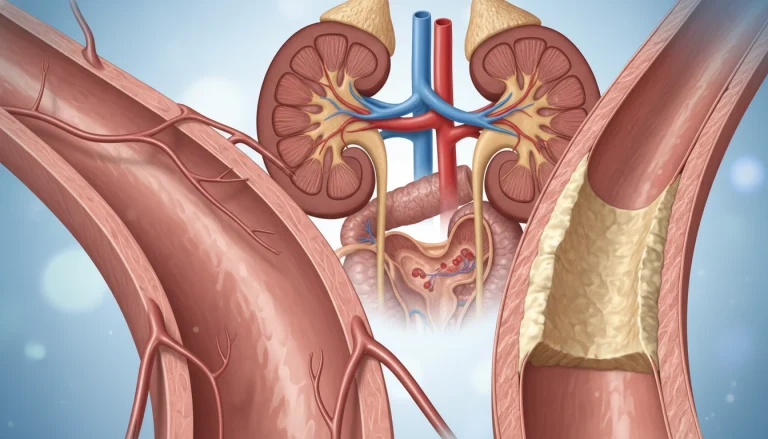
Potential Complications of Untreated Ulcers
Untreated ulcers can lead to severe and potentially life-threatening complications. It is vital to understand these risks to appreciate the importance of timely medical intervention.
Bleeding
Bleeding is a common complication, occurring when the ulcer erodes into a blood vessel. This can result in significant blood loss, requiring immediate medical attention. Symptoms include vomiting blood or black tarry stools.
Perforation
A perforated ulcer occurs when the ulcer penetrates through the stomach or duodenal wall, spilling contents into the abdominal cavity. This condition is a medical emergency, often presenting with severe abdominal pain. It requires surgical intervention.
Obstruction
Long-standing ulcers can cause narrowing of the stomach or duodenal passage, leading to obstruction. Symptoms include severe vomiting, abdominal pain, and significant weight loss. Treatment often involves addressing the underlying cause and may include surgical options.
Long-term Health Implications
Chronic ulcers can have long-term health implications, including an increased risk of stomach cancer. Managing ulcers effectively is critical to prevent these complications and ensure overall health.
- Regular medical check-ups can help monitor ulcer conditions.
- Adhering to prescribed treatments is vital for preventing complications.
- Lifestyle modifications can support ulcer management and overall health.
Medical Treatments for Ulcer
Ulcer treatment focuses on healing the ulcer, preventing complications, and reducing recurrence risk. It involves various medical interventions. The treatment choice depends on the ulcer type and cause.
Antibiotics for H. Pylori
Antibiotics are key for ulcers caused by H. pylori infection. They eliminate the bacteria, lowering recurrence risk.
Common Antibiotic Regimens
A combination of two antibiotics and a proton pump inhibitor (PPI) treats H. pylori. Amoxicillin and clarithromycin are common choices.
Treatment Duration and Efficacy
Antibiotic treatment lasts 7 to 14 days. Follow-up tests confirm H. pylori eradication, assessing treatment success.
Proton Pump Inhibitors
Proton pump inhibitors (PPIs) are vital in ulcer treatment. They reduce stomach acid, creating a healing-friendly environment.
H2 Receptor Blockers
H2 receptor blockers decrease stomach acid production differently than PPIs. They treat ulcers and are an option for those who can’t take PPIs.
Other Prescription Medications
Other drugs protect the stomach lining and aid healing, alongside antibiotics and acid reducers.
Antacids
Antacids neutralize stomach acid, providing quick ulcer symptom relief. They are available over-the-counter.
Cytoprotective Agents
Cytoprotective agents protect the stomach lining, aiding ulcer healing.
Bismuth Subsalicylate
Bismuth subsalicylate has antimicrobial properties. It’s used in H. pylori treatment, often with antibiotics.
Understanding medical treatments helps individuals with ulcers develop effective treatment plans with their healthcare providers.
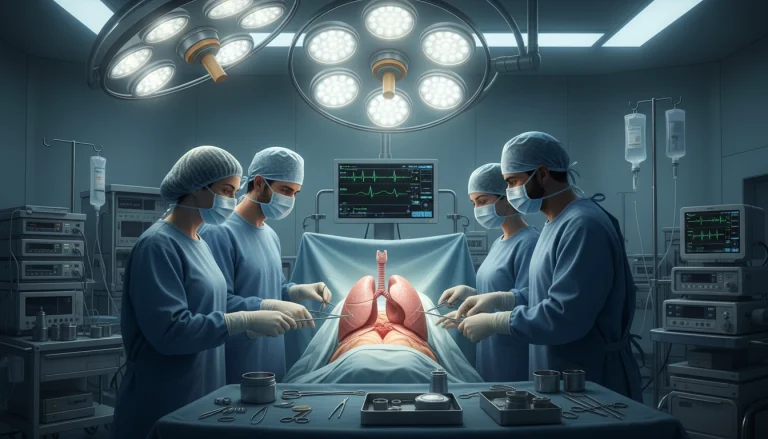
Surgical Interventions for Severe Cases
When ulcers are severe and don’t respond to medication, surgery is often the next step. This is usually for complications like severe bleeding, perforation, or obstruction.
When Surgery Is Necessary
Surgery is needed when an ulcer causes a complication that can’t be fixed with medication. This includes severe bleeding that can’t be stopped with endoscopy, perforation of the stomach or duodenum, or blockage of the stomach or intestine due to scarring.
Types of Surgical Procedures
Several surgical methods can treat severe ulcers, each with its own use and benefits.
Vagotomy
Vagotomy involves cutting the vagus nerve to lower stomach acid production.
Antrectomy
Antrectomy removes the lower stomach part (antrum), which makes stomach acid.
Pyloroplasty
Pyloroplasty widens the pyloric channel, helping food move from the stomach to the small intestine.

Recovery and Post-Surgical Care
Recovering from ulcer surgery requires careful diet management, monitoring for complications, and sometimes lifestyle changes to prevent future issues. Patients are usually advised to gradually return to normal activities and eating habits.
Dietary Management for Ulcer Patients
Managing diet is key in ulcer care, affecting both healing and symptom relief. A balanced diet can ease symptoms, aid in healing, and enhance life quality for ulcer patients.
Foods to Include
Choosing the right foods is vital for ulcer patients. Certain groups offer significant benefits.
High-Fiber Options
High-fiber foods like whole grains, fruits, and vegetables soothe the digestive system. They also promote healing.
Probiotic-Rich Foods
Probiotics in yogurt, kefir, and fermented vegetables boost gut health. They aid in recovery.
Anti-inflammatory Foods
Foods with anti-inflammatory properties, like omega-3s in fish and flaxseeds, reduce inflammation. They promote healing.
Foods to Avoid
Some foods can worsen ulcer symptoms and hinder healing. It’s important to know and avoid these.
Common irritants include spicy foods, citrus fruits, and caffeinated drinks. They can irritate the stomach lining and worsen symptoms.
Meal Planning and Eating Habits
Effective meal planning and healthy eating habits are essential for managing ulcers. Eating smaller, more frequent meals can ease symptoms.
Avoiding late-night eating and choosing gentle, easily digestible foods supports healing.
Nutritional Supplements
In some cases, nutritional supplements are recommended to support ulcer healing. Supplements like vitamin and mineral complexes can fill dietary gaps.
Lifestyle Modifications to Support Healing
Effective ulcer management requires specific lifestyle changes to aid in the healing process. By adopting these modifications, individuals can significantly improve their overall health. This also reduces the risk of ulcer recurrence.
Stress Management Techniques
Stress can worsen ulcer symptoms, making stress management critical in ulcer care. Techniques like mindfulness, relaxation exercises, and therapy are essential to manage stress effectively.
Mindfulness and Meditation
Mindfulness and meditation practices have been shown to reduce stress levels and promote relaxation.
Relaxation Exercises
Relaxation exercises, including deep breathing and progressive muscle relaxation, can help calm the mind and body.
Therapy Options
Cognitive-behavioral therapy (CBT) and other forms of talk therapy can provide individuals with tools to manage stress effectively.
Sleep Hygiene
Maintaining good sleep hygiene is essential for overall health and supports ulcer healing. This includes establishing a consistent sleep schedule, creating a restful sleep environment, and avoiding stimulants before bedtime.
Physical Activity Recommendations
Regular physical activity can help reduce stress and promote healing. Gentle exercises such as walking or yoga are recommended.
Avoiding Harmful Substances
Avoiding substances like tobacco and excessive alcohol can help prevent further irritation to the stomach lining. It supports the healing process.
Natural and Home Remedies for Ulcer Relief
Alongside traditional treatments, natural and home remedies offer relief for ulcer patients. These methods can complement medical treatments, helping manage symptoms and aid in healing.
Herbal Treatments
Herbal remedies have been a cornerstone in traditional medicine for centuries, addressing various health concerns, including ulcers. Key herbs for ulcer relief include:
- Licorice Root
- Aloe Vera
- Cabbage Juice
Licorice Root
Licorice root is renowned for its anti-inflammatory properties. It helps soothe the stomach lining, reducing ulcer symptoms effectively.
Aloe Vera
Aloe vera juice is known for its anti-inflammatory and healing properties. It aids in reducing inflammation and promoting healing in the digestive tract, alleviating ulcer symptoms.
Cabbage Juice
Cabbage juice is packed with vitamins and minerals. These nutrients protect the stomach lining and support healing.
Dietary Supplements
Dietary supplements are vital in managing ulcer symptoms. Probiotics, vitamin C, and zinc supplements promote healing and reduce inflammation.
Evidence-Based Alternative Approaches
Alternative methods like acupuncture and stress management have shown efficacy in reducing ulcer symptoms. These approaches can enhance overall well-being when used alongside conventional treatments.
Preventing Ulcer Recurrence
Preventing ulcer recurrence is key to long-term health after treatment. It requires a mix of medication, lifestyle changes, and ongoing monitoring.
Long-term Medication Management
Many patients need ongoing medication to avoid ulcers coming back. This might include antibiotics to kill H. pylori or PPIs to lower stomach acid.
Sticking to the medication plan is essential. Patients should keep in close touch with their doctor to tweak dosages or switch meds as needed.
Regular Medical Check-ups
Regular doctor visits are critical for tracking healing and catching early signs of ulcers. These visits also let doctors tweak treatment plans.
At these check-ups, patients should share any symptoms or worries, no matter how small. Early action can greatly improve results.
Lifestyle Maintenance
Maintaining a healthy lifestyle is vital in preventing ulcers from coming back. This includes eating right, managing stress, and avoiding harmful substances like tobacco and too much alcohol.
- Eating a balanced diet rich in fruits, vegetables, and whole grains
- Avoiding spicy or acidic foods that can irritate the stomach lining
- Managing stress through techniques like meditation or yoga
Early Intervention Strategies
Early action is key to dealing with any signs of ulcer recurrence. Patients should know the symptoms to look out for and seek help if they feel unusual discomfort or pain.
Combining long-term medication, regular doctor visits, healthy living, and quick action can greatly lower the risk of ulcers coming back. This helps keep overall health in check.
The Road to Recovery: Managing Your Ulcer for Long-term Health
Effectively managing an ulcer is key to long-term health and preventing its return. Understanding the causes, symptoms, and treatment options empowers individuals to take charge of their condition. This can significantly enhance their quality of life.
Ulcer management involves a multifaceted approach. This includes medical treatments, lifestyle changes, and dietary adjustments. For ulcers caused by H. pylori, proton pump inhibitors and antibiotics are often prescribed. Stress management, through practices like meditation and yoga, can also aid in symptom relief and healing.
A diet rich in fiber, fruits, and vegetables is beneficial for ulcer recovery. It’s important to avoid foods and substances that can irritate the stomach, such as spicy foods, caffeine, and NSAIDs. Regular health check-ups are vital for monitoring progress and making necessary adjustments to treatment plans.
By implementing these strategies and maintaining a healthy lifestyle, individuals can achieve long-term health and lower the risk of ulcer recurrence. Effective management of ulcers allows people to live active, healthy lives, unencumbered by the symptoms of ulcers.
FAQ
Q: What is an ulcer?
A: An ulcer is a sore that forms on the lining of the esophagus, stomach, or small intestine. It’s often caused by acid or bacterial infection.
Q: What are the common symptoms of an ulcer?
A: Symptoms include abdominal pain, nausea, vomiting, loss of appetite, and bleeding.
Q: How is an ulcer diagnosed?
A: Diagnosis involves a physical exam, medical history, lab tests, endoscopy, and imaging.
Q: What are the complications of untreated ulcers?
A: Untreated ulcers can cause bleeding, perforation, obstruction, and long-term health issues.
Q: How are ulcers treated?
A: Treatment includes antibiotics for H. pylori, proton pump inhibitors, H2 blockers, and prescription meds. Lifestyle and dietary changes are also key.
Q: Can ulcers be prevented?
A: Yes, by avoiding NSAIDs, smoking, and excessive alcohol. A healthy diet and lifestyle also help prevent ulcers.
Q: What lifestyle changes can help manage ulcers?
A: Stress management, good sleep, exercise, and avoiding harmful substances aid in ulcer management and healing.
Q: Are there any natural remedies for ulcer relief?
A: Natural remedies like licorice root, aloe vera, and cabbage juice may help. But their effectiveness varies.
Q: How can ulcer recurrence be prevented?
A: Prevent recurrence with long-term medication, regular check-ups, lifestyle maintenance, and early intervention.