Uterine Prolapse: What is Uterine Prolapse?
Uterine prolapse is a common condition among women, where the uterus slips out of its usual position. This displacement can lead to discomfort and disrupt daily activities. It’s essential to understand the causes, symptoms, and treatment options for managing this condition. Factors like childbirth, age, and weak pelvic floor muscles can contribute to its development.
Recognizing the signs and seeking medical attention can greatly improve the quality of life for those affected. Treatment options range from lifestyle changes to surgical interventions. Uterine prolapse is when the uterus moves out of its normal place, causing health issues. This happens when the muscles and ligaments that hold it in place weaken. As a result, the uterus can slide into the vaginal canal.
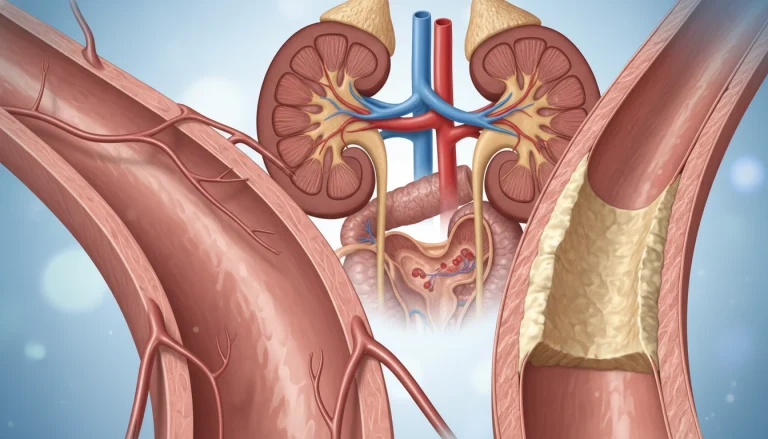
Definition and Basic Anatomy
The uterus is a key part of the female reproductive system. It’s held in place by muscles, ligaments, and fascia. When these tissues weaken, often due to childbirth, aging, or other factors, uterine prolapse can occur. Knowing the anatomy is key to understanding how this condition arises and its effects on women’s health.
Prevalence and Demographics
Many women experience uterine prolapse, mainly those who have had vaginal births. The condition’s prevalence grows with age, peaking during and after menopause. This is because estrogen levels drop, weakening the supportive tissues. Women who have had multiple vaginal deliveries are at higher risk, underscoring the need for postpartum care and maintaining pelvic floor health.
Types and Grades of Uterine Prolapse
Grasping the types and grades of uterine prolapse is key to accurate diagnosis. This condition, though complex, shows varying degrees of severity and presentation.
Classification System
The classification of uterine prolapse is based on its degree, assessed during a physical exam. The Pelvic Organ Prolapse Quantification (POP-Q) system is widely used. It measures vaginal and cervical points relative to the hymen, standardizing prolapse severity.
Healthcare providers use the POP-Q system to stage prolapse from Stage 0 (no prolapse) to Stage IV (complete prolapse). This staging is vital for treatment planning and clear communication of the diagnosis.
Severity Levels Explained
The severity of uterine prolapse is categorized into stages based on POP-Q measurements. These stages reveal the prolapse’s extent and its quality of life impact.
- Stage 0: No prolapse is observed.
- Stage I: The prolapse is minimal, and the leading edge of the prolapse remains above the level of the hymen.
- Stage II: The prolapse is more pronounced, with the leading edge at or just below the hymen.
- Stage III: The prolapse is significant, with the leading edge more than 1 cm below the hymen but not completely outside.
- Stage IV: Complete prolapse, where the entire vagina and uterus are outside the introitus.
Understanding these stages is critical for diagnosis and treatment planning. The severity level directs healthcare providers to the most suitable interventions, from conservative management to surgery.
Common Causes of Uterine Prolapse
Uterine prolapse is caused by a mix of factors that weaken the pelvic floor muscles and supportive tissues. Knowing these causes is key for prevention and treatment.
Pregnancy and Childbirth
Pregnancy and childbirth play a big role in uterine prolapse. Carrying a baby and giving birth can weaken the muscles and ligaments that hold the uterus in place.
- Having multiple pregnancies raises the risk.
- Vaginal delivery, if complicated or assisted, strains pelvic floor muscles.
- Poor recovery after childbirth can also weaken support.
Aging and Menopause
Aging and menopause are also major factors in uterine prolapse. As women get older, the muscles and tissues that support the pelvic organs naturally weaken.
Menopause makes this condition worse because estrogen levels drop. Estrogen is key for keeping pelvic floor tissues strong and elastic.
Other Contributing Factors
Other factors can also increase the risk of uterine prolapse.
- Chronic coughing or straining raises abdominal pressure.
- Being overweight adds extra strain on the pelvic floor.
- Genetic predisposition can affect the strength and resilience of pelvic support tissues.
These factors can individually or together raise the risk of uterine prolapse. This shows why a full approach to prevention and management is vital.
Risk Factors for Developing Uterine Prolapse
The onset of uterine prolapse is influenced by genetics, lifestyle, and medical conditions. Recognizing these factors is key to spotting those at higher risk. It also helps in taking preventive steps.
Genetic Predisposition
Genetics significantly impact the risk of uterine prolapse. Women with a family history of pelvic floor issues are more prone to it. This is due to inherent weaknesses in the connective tissue supporting the pelvic organs.
Lifestyle Factors
Lifestyle choices greatly influence the risk of uterine prolapse.
- Pregnancy and childbirth, and multiple vaginal deliveries, strain pelvic floor muscles.
- Chronic coughing, heavy lifting, and obesity increase intra-abdominal pressure, stressing the pelvic floor.
- A sedentary lifestyle weakens muscles supporting the pelvic organs.
Medical Conditions
Certain medical conditions raise the risk of uterine prolapse. Conditions that increase intra-abdominal pressure, like chronic constipation or pelvic tumors, strain pelvic floor muscles. Conditions affecting connective tissue, such as Ehlers-Danlos syndrome, also increase risk.
Healthcare providers can offer specific advice and interventions to women at higher risk. This can potentially lower the incidence of uterine prolapse.
Recognizing Symptoms of Uterine Prolapse
Identifying the signs of uterine prolapse is key to managing it well. This condition happens when the uterus moves out of its usual spot. The symptoms can change based on how severe the prolapse is.
Physical Symptoms
Physical signs are often the first things women notice about uterine prolapse. They might feel a heavy or pulling sensation in the pelvis. Or, they might feel like something is falling out of the vagina.
In more serious cases, the prolapse can be seen as a bulge or protrusion. This can cause discomfort and impact daily life.
Urinary and Bowel Symptoms
Uterine prolapse can also affect how you go to the bathroom. Some women might leak urine or have trouble emptying their bladder.
They might also get urinary tract infections more often. Bowel issues can include constipation or trouble passing stool.
Sexual Function Impact
Uterine prolapse can also affect sex. Women might feel pain or discomfort during sex.
They might also have a lower sex drive or find it hard to reach orgasm. It’s important to address these issues for better sexual health.
Knowing these symptoms can help women get medical help early. This can stop the prolapse from getting worse and improve treatment results.
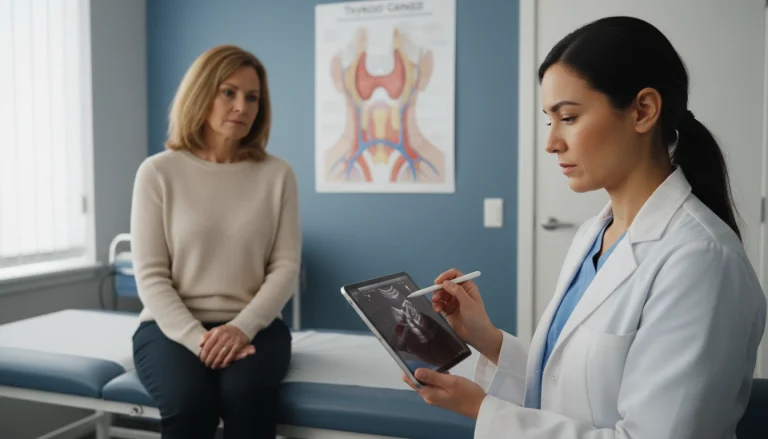
Diagnosis Process
Diagnosing uterine prolapse requires a thorough physical examination and sometimes additional tests. A healthcare provider will first review the patient’s medical history. This helps identify any factors that might contribute to the condition.
Physical Examination
A physical exam is key in diagnosing uterine prolapse. The healthcare provider will conduct a pelvic exam to gauge the prolapse’s severity. They may ask the patient to cough or strain. This helps observe the prolapse’s extent in different positions.

Imaging and Additional Tests
Though a physical exam is often enough, imaging tests like ultrasound or MRI might be needed. These help rule out other conditions and assess the prolapse’s extent. Urodynamic tests may also be done to check bladder function and urinary symptoms related to the prolapse.
Healthcare providers use findings from both the physical exam and diagnostic tests to accurately diagnose uterine prolapse. They then create a suitable treatment plan based on these results.
Conservative Treatment Options
Uterine prolapse can be managed through various conservative treatment methods. These non-surgical options help alleviate symptoms and improve quality of life. They are ideal for those who wish to avoid surgery or are not immediate candidates for it.
Pelvic Floor Exercises
Pelvic floor exercises, also known as Kegel exercises, are a cornerstone in managing uterine prolapse. These exercises strengthen the muscles that support the pelvic organs. This can potentially reduce the severity of prolapse symptoms. To perform Kegel exercises effectively:
- Identify the correct muscles by stopping the flow of urine midstream.
- Contract these muscles for 5-10 seconds, then release for the same duration.
- Repeat this process 10-15 times, several times a day.
Consistency is key, as noticeable improvements may take several weeks to months.
Pessaries and Support Devices
Pessaries are removable devices inserted into the vagina to support the prolapsed uterus. They come in various shapes and sizes, and a healthcare provider can help determine the most suitable type. Pessaries can be an effective short-term or long-term solution, providing immediate relief from prolapse symptoms. Regular follow-up with a healthcare provider is necessary to ensure proper fit and to clean the device.
Lifestyle Modifications
In addition to specific treatments, certain lifestyle modifications can help manage uterine prolapse symptoms. These include:
- Maintaining a healthy weight to reduce pressure on the pelvic floor.
- Avoiding heavy lifting and bending.
- Engaging in regular, gentle exercise to improve overall pelvic health.
These changes can complement other conservative treatments, making them more effective.
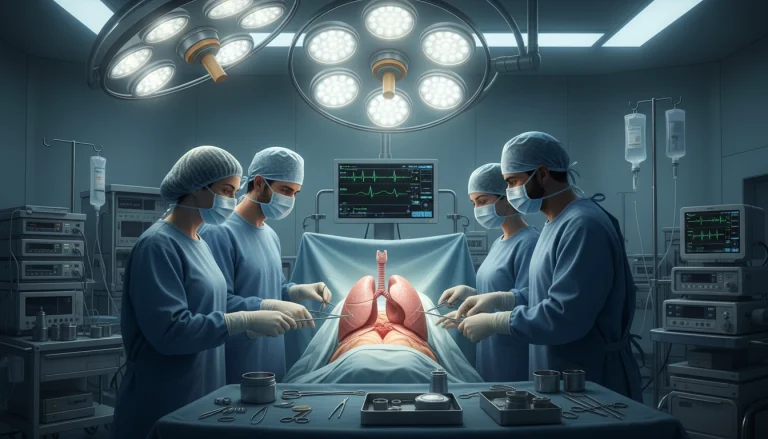
Surgical Interventions for Uterine Prolapse
The surgical management of uterine prolapse involves various procedures. Each is tailored to address specific aspects of the condition. These interventions are considered when conservative treatments fail or when the prolapse is severe.
Reconstructive Procedures
Reconstructive surgery aims to restore the normal anatomy of the pelvic organs. This can include procedures like hysterectomy (removal of the uterus). Additional repairs, such as sacrocolpopexy or sacrohysteropexy, may be done to suspend the vaginal vault or uterus to the sacrum.
These surgeries can be performed through different routes. Options include abdominal, vaginal, or laparoscopic approaches. Each has its own benefits and complications.
Obliterative Procedures
Obliterative surgery, like colpocleisis, involves closing off the prolapsed vagina. It’s usually reserved for older women who are not sexually active. This procedure results in the loss of vaginal function.
It’s a less invasive option with a quicker recovery. This makes it an attractive choice for some patients.
Minimally Invasive Approaches
Minimally invasive surgical techniques, including laparoscopy and robotic-assisted surgery, offer benefits. These include smaller incisions, less pain, and faster recovery times. They can be used for various reconstructive procedures.
Recovery and Expectations
Recovery from uterine prolapse surgery varies by procedure. Patients can expect some discomfort. There may also be restrictions on heavy lifting and strenuous activities for several weeks.
Understanding the risks and benefits of each surgical option is key. It’s essential for making an informed decision.
Complications of Untreated Uterine Prolapse
Uterine prolapse, if left untreated, can lead to serious physical and psychological issues. It’s vital for women to understand these complications to seek timely medical help.
Physical Complications
Untreated uterine prolapse can cause significant physical problems. These include:
- Chronic pelvic pain and discomfort
- Urinary incontinence and recurrent urinary tract infections
- Difficulty with bowel movements and possible fecal incontinence
- Ulceration or infection of the prolapsed uterus
These physical issues can greatly affect a woman’s daily life and overall health.
Psychological Impact
The psychological effects of untreated uterine prolapse are profound. Women may face:
- Anxiety and depression due to chronic discomfort and pain
- Embarrassment and self-consciousness about their condition
- Impact on body image and self-esteem
- Strain on sexual relationships due to discomfort or pain
Dealing with uterine prolapse is not just about physical relief. It’s also about addressing its psychological toll.
Emotional and Psychological Aspects
Uterine prolapse is more than a physical issue; it deeply affects a woman’s emotional and psychological well-being. It can alter her quality of life, causing emotional distress beyond physical discomfort.
Impact on Body Image and Self-Esteem
Uterine prolapse can significantly impact a woman’s body image and self-esteem. It may lead to feelings of insecurity and low confidence. Women might feel self-conscious about their bodies, affecting their:
- Participation in social activities
- Anxiety in intimate relationships
- Mental well-being
The physical symptoms of uterine prolapse, such as discomfort or pain, can worsen these feelings.
Coping Strategies
It’s essential to develop effective coping strategies for managing uterine prolapse’s emotional impact. Some strategies include:
- Seeking support from healthcare providers or support groups
- Engaging in stress-reducing activities, such as meditation or yoga
- Practicing open communication with partners and loved ones about the condition
Mental Health Support
Mental health support is vital for managing uterine prolapse. Women should seek professional help if they experience symptoms of anxiety or depression.
Treatment options may include counseling, therapy, or other mental health support. Addressing both physical and emotional aspects of uterine prolapse can improve a woman’s quality of life.
Prevention Strategies
To prevent uterine prolapse, a multi-faceted approach is necessary. It involves maintaining pelvic floor health and considering pregnancy and delivery factors. By focusing on these areas, women can lower their risk of uterine prolapse significantly.
Pelvic Floor Health Maintenance
Keeping the pelvic floor healthy is key to preventing uterine prolapse. This can be done through:
- Regular pelvic floor exercises, such as Kegel exercises, to strengthen the muscles supporting the uterus.
- Avoiding heavy lifting and bending to reduce strain on the pelvic floor.
- Maintaining a healthy weight to decrease pressure on the pelvic organs.
These practices not only help prevent uterine prolapse but also contribute to overall pelvic health.
Pregnancy and Delivery Considerations
Pregnancy and childbirth are significant factors in the development of uterine prolapse. To mitigate this risk:
- Regular prenatal care is essential to monitor the health of both mother and baby.
- A healthcare provider should be consulted regarding the best delivery options, as cesarean delivery may be recommended in some cases to reduce the risk of prolapse.
- Postpartum pelvic floor rehabilitation can help restore the strength and function of the pelvic floor muscles.
By being informed and proactive during pregnancy and delivery, women can reduce their risk of uterine prolapse.
Living with Uterine Prolapse
Understanding how to live with uterine prolapse is key to reducing its impact and improving well-being. This condition can greatly affect daily life. Yet, with the right strategies, women can manage their symptoms effectively.
Daily Management Techniques
Effective daily management of uterine prolapse involves several techniques. Pelvic floor exercises, such as Kegel exercises, strengthen the muscles supporting the uterus. Lifestyle adjustments like maintaining a healthy weight, avoiding heavy lifting, and managing chronic coughing also help reduce strain on the pelvic floor.
Support devices like pessaries can offer relief and support to the prolapsed uterus. These devices come in various shapes and sizes and are typically fitted by a healthcare provider.

Support Resources
Living with uterine prolapse can be challenging, both physically and emotionally. Support resources, including online forums, support groups, and counseling services, offer valuable guidance and emotional support. Connecting with others who face similar challenges can be incredibly helpful.
Communication with Healthcare Providers
Open and honest communication with healthcare providers is essential for managing uterine prolapse effectively. Regular check-ups and discussing any symptom changes or concerns are vital. Patients should feel empowered to ask questions and seek a second opinion if needed.
When to Seek Medical Attention
Knowing when to seek medical help for uterine prolapse is key to managing the condition effectively. If you feel a heaviness or pulling in your pelvis, or notice a bulge in your vagina, see a healthcare provider. These signs indicate a need for professional evaluation.
Visiting a doctor is necessary if you struggle to empty your bladder or bowels, experience urinary incontinence, or have persistent pelvic pain. Women with uterine prolapse may also find sex uncomfortable. This discomfort can greatly affect your quality of life.
Timely medical attention is vital. It lets healthcare providers evaluate the prolapse’s severity and suggest the right treatment. This can range from non-surgical methods to surgery. Early action can prevent further issues and improve your health outcomes.
If you’re showing any of these symptoms or have concerns about uterine prolapse, make an appointment with your healthcare provider. Discussing your situation will help determine the best treatment for you.
FAQ About Uterine Prolapse
Q: What is uterine prolapse?
A: Uterine prolapse occurs when the uterus slips into the vagina. This happens when the muscles and ligaments that hold it in place weaken. As a result, the uterus descends.
Q: What are the symptoms of uterine prolapse?
A: Symptoms include feeling a heaviness or pulling in the pelvis. You might also experience vaginal bleeding or discharge. Difficulty with urination or bowel movements and discomfort during sex are common.
Q: What causes uterine prolapse?
A: Several factors contribute to uterine prolapse. Pregnancy and childbirth are major causes. Aging and menopause also play a role. Certain medical conditions that weaken the pelvic muscles and ligaments are additional factors.
Q: How is uterine prolapse diagnosed?
A: Diagnosis involves a physical exam, including a pelvic exam. Imaging tests like ultrasound or MRI might be used to assess the prolapse’s extent.
Q: What are the treatment options for uterine prolapse?
A: Treatment options vary. Conservative methods include pelvic floor exercises and using pessaries or support devices. Surgical options include reconstructive or obliterative procedures.
Q: Can uterine prolapse be prevented?
A: Prevention is possible to some extent. Maintaining pelvic floor health through exercises and managing weight can help. Avoiding heavy lifting is also beneficial. Proper care during pregnancy and delivery is key.
Q: How does uterine prolapse affect daily life?
A: It can make daily activities uncomfortable. It may affect urinary and bowel habits and sexual function. Lifestyle adjustments and treatment are necessary to manage the condition.
Q: What are the complications of untreated uterine prolapse?
A: Untreated prolapse can lead to physical complications like ulcers or infections. It can also cause psychological impacts, including anxiety and depression. Seeking medical care can prevent these issues.
Q: When should I seek medical attention for uterine prolapse?
A: Seek medical attention if symptoms worsen or persist. Look for signs of infection or significant discomfort affecting daily life or sexual function.