Understanding Ventricular Septal Defect (VSD)
A Ventricular Septal Defect (VSD) is a congenital heart condition where an opening exists in the septum between the heart’s two ventricles. This opening allows blood to flow from one ventricle to the other. Such a defect can lead to various complications if not addressed. Having a VSD can have a significant impact on one’s health, mainly if it remains untreated. It is essential to understand the causes, symptoms, and treatment options for VSD. This knowledge is vital for effective management and care.
This article aims to provide a detailed overview of VSD. It covers its diagnosis and treatment options. Our goal is to educate readers about this critical heart condition. To grasp the intricacies of Ventricular Septal Defect (VSD), one must explore cardiac anatomy and its anomalies. VSD is a congenital condition marked by an opening in the septum, which divides the heart’s two ventricles. This opening allows blood to flow from one ventricle to the other, potentially causing cardiac complications.
Definition and Basic Cardiac Anatomy
The heart consists of four chambers: the right and left atria, and the right and left ventricles. The ventricles are the heart’s main pumping chambers, with the septum separating them. A Ventricular Septal Defect occurs when there’s an abnormal opening in this septum. The size and location of this opening can vary. Understanding cardiac anatomy is key to understanding how VSD impacts heart function.
Prevalence and Epidemiology
Ventricular Septal Defect is a common congenital heart defect, affecting about 2-5 per 1000 live births. Its epidemiology shows it can occur alone or with other cardiac anomalies or genetic syndromes. Research indicates that VSD prevalence can differ by geographical location and population demographics.
Types of Ventricular Septal Defects
VSDs are categorized into four main types: perimembranous, muscular, inlet, and outlet defects. These classifications are based on the location of the defect within the ventricular septum. The septum is the wall between the heart’s two ventricles.
Perimembranous VSDs
Perimembranous VSDs are the most prevalent type. They are situated near the junction of the aortic, mitral, and tricuspid valves. These defects often coexist with other congenital heart issues, making diagnosis complex due to their location.
Muscular VSDs
Muscular VSDs occur within the muscular part of the ventricular septum. They can be single or multiple, earning the nickname “Swiss cheese” septum for multiple defects. Muscular VSDs are more likely to close on their own compared to other types.
Inlet VSDs
Inlet VSDs are found near the inlet of the ventricles, close to the atrioventricular valves. They are commonly linked with atrioventricular septal defects. These defects can be part of more complex congenital heart diseases.
Outlet VSDs
Outlet VSDs are located in the uppermost part of the ventricular septum, near the semilunar valves. They can be associated with aortic valve abnormalities, such as prolapse or regurgitation. This is due to their proximity to the aortic valve.
Identifying the specific type of VSD is essential for tailoring the treatment plan and predicting complications. Each type has unique characteristics and clinical implications. Accurate diagnosis is critical.
Pathophysiology of VSDs
Understanding the pathophysiology of Ventricular Septal Defects (VSDs) is key to diagnosing and treating this common congenital heart condition. A VSD disrupts the heart’s normal function, causing significant changes in blood flow.
Normal Heart Function
The heart acts as a highly efficient pump, ensuring blood circulates throughout the body. It consists of four chambers: the right and left atria, and the right and left ventricles. The ventricles are separated by the ventricular septum, preventing direct blood flow between them. In a healthy heart, blood moves from the right ventricle to the lungs for oxygenation and then to the rest of the body from the left ventricle.
Altered Hemodynamics in VSD
In individuals with VSD, an abnormal opening in the ventricular septum allows blood to flow between the left and right ventricles. This leads to left-to-right shunting, where oxygen-rich blood from the left ventricle mixes with oxygen-poor blood in the right ventricle. This results in increased blood volume being pumped to the lungs, potentially causing pulmonary congestion and hypertension over time. The severity of these changes depends on the size and location of the VSD.
The altered hemodynamics in VSD can lead to various clinical manifestations, including heart failure, pulmonary hypertension, and arrhythmias. Understanding these changes is essential for managing the condition effectively.
Causes and Risk Factors
Ventricular Septal Defect (VSD) is a prevalent congenital heart defect. It stems from genetic and environmental factors. Grasping these causes is vital for timely diagnosis and treatment of VSD.
Genetic Factors
Genetics significantly influence VSD development. Research indicates that a family history of congenital heart defects raises the risk. Specific genetic syndromes, like Down syndrome, also elevate this risk.
Environmental Factors
Environmental exposures during pregnancy can also contribute to VSD. Maternal alcohol use and exposure to certain chemicals are linked to higher congenital heart defect rates.
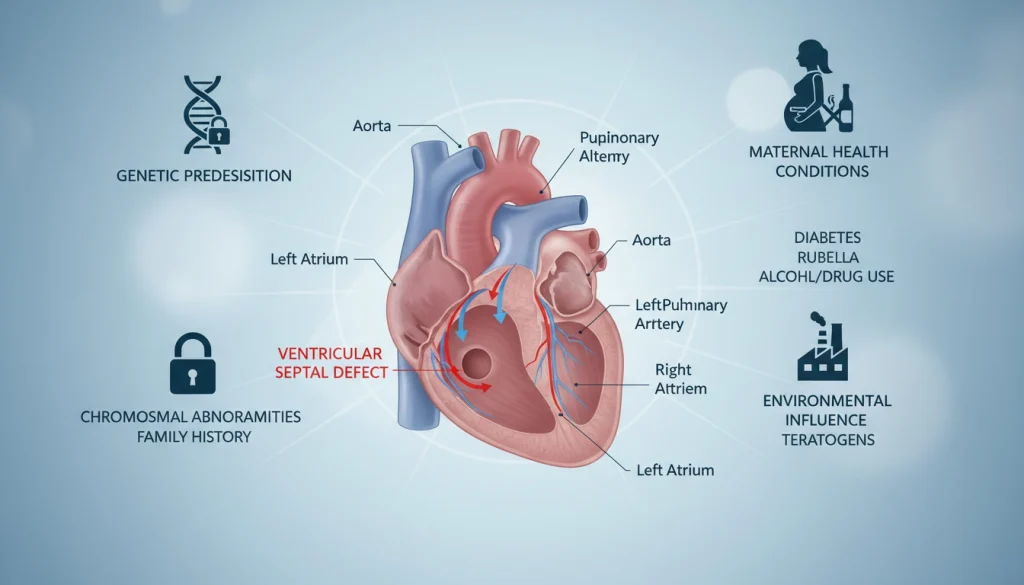
Associated Syndromes and Conditions
Certain syndromes and conditions increase VSD risk. These include chromosomal abnormalities and other congenital anomalies. Identifying these can aid in early diagnosis and management of VSD.
When VSD occurs with other syndromes or conditions, a holistic treatment plan is required. This approach considers the individual’s overall health.
Signs and Symptoms
Understanding the signs and symptoms of VSD is essential for early detection and management. These signs vary across age groups. Ventricular Septal Defect, a common congenital heart defect, presents differently among individuals. Awareness of its manifestations at different ages is necessary.
Symptoms in Infants
Infants with VSD may show symptoms like rapid breathing, poor feeding, and failure to gain weight. These symptoms occur because the defect allows blood to flow from the left to the right ventricle. This can lead to increased pulmonary blood flow and congestion.
In some cases, infants may also show signs of fatigue during feeding, sweating, or irritability. Early detection through physical examination and echocardiography is critical for managing these symptoms effectively.
Symptoms in Children
As children grow, the symptoms of VSD may evolve. Some children may remain asymptomatic, while others might experience recurrent respiratory infections or failure to thrive. Larger defects can lead to more pronounced symptoms, including shortness of breath during play or activity.
Children with VSD are also at risk for developing pulmonary hypertension if the defect is large and not adequately managed. Regular follow-up with a pediatric cardiologist is essential to monitor the defect’s size and impact.
Symptoms in Adults
Adults with undiagnosed or untreated VSD may present with symptoms such as shortness of breath, palpitations, or fatigue. Some adults may have lived with a small, asymptomatic defect their entire lives. Others may have undergone surgical repair in childhood.
In adults, complications such as pulmonary hypertension, heart failure, or arrhythmias can occur if the VSD is large and has caused significant hemodynamic changes over time. Monitoring and potentially treating these complications are critical aspects of managing VSD in adults.
Recognizing the signs and symptoms of VSD across different age groups is vital for timely diagnosis and appropriate management. Whether in infants, children, or adults, understanding these symptoms can lead to better outcomes.
When to Seek Medical Attention
For those with VSD, knowing when to seek medical help is critical. It’s essential to recognize the signs that signal a need for immediate care or routine evaluation.
Emergency Warning Signs
Certain symptoms demand immediate medical attention. These include difficulty breathing, chest pain, or severe fatigue. If you or your child shows any of these signs, seek emergency care without delay.
Routine Evaluation Indicators
Regular check-ups are key for monitoring VSD. Look out for changes in breathing patterns, poor weight gain in infants, or palpitations. Consulting a healthcare provider for these signs is vital for effective management of VSD.
Diagnosis of Ventricular Septal Defect (VSD)
Accurate diagnosis of VSD is critical and involves a multi-faceted approach. This includes physical examination and imaging studies. A thorough assessment combines clinical findings with advanced diagnostic techniques.
Physical Examination Findings
The first step in diagnosing VSD is a physical examination. It may reveal a harsh holosystolic murmur at the left lower sternal border. A thrill might also be detected in some instances.
Echocardiography and Imaging
Echocardiography is key in diagnosing VSD, providing detailed heart images. It helps identify defect location, size, and number. Cardiac MRI or CT scans may be used in specific cases.
Cardiac Catheterization
Cardiac catheterization is an invasive procedure for assessing VSD’s hemodynamic impact. It measures heart chamber pressures. It’s useful in complex cases or for planning interventions.
Other Diagnostic Tests
Additional tests like electrocardiogram (ECG) and chest X-ray are used. They evaluate cardiac function and look for heart failure signs or complications.
Diagnosing VSD is complex, relying on physical examination, imaging, and other tests. Accurate diagnosis is vital for choosing the right treatment.
Classification by Size and Hemodynamic Impact
Understanding the size of a VSD and its hemodynamic impact is key to choosing the right treatment. The classification of VSDs by size and hemodynamic effects guides clinicians. It helps predict symptoms, complications, and the need for intervention.
Small VSDs
Small VSDs are less than 25% of the aortic root’s diameter. They usually have a minimal hemodynamic impact. This often means they don’t cause significant symptoms.
Moderate VSDs
Moderate VSDs have a more significant hemodynamic effect. This can increase the heart’s workload. Symptoms may start to appear, requiring closer monitoring.
Large VSDs
Large VSDs significantly alter hemodynamics, causing substantial left-to-right shunting. This can lead to heart failure and pulmonary hypertension if untreated. 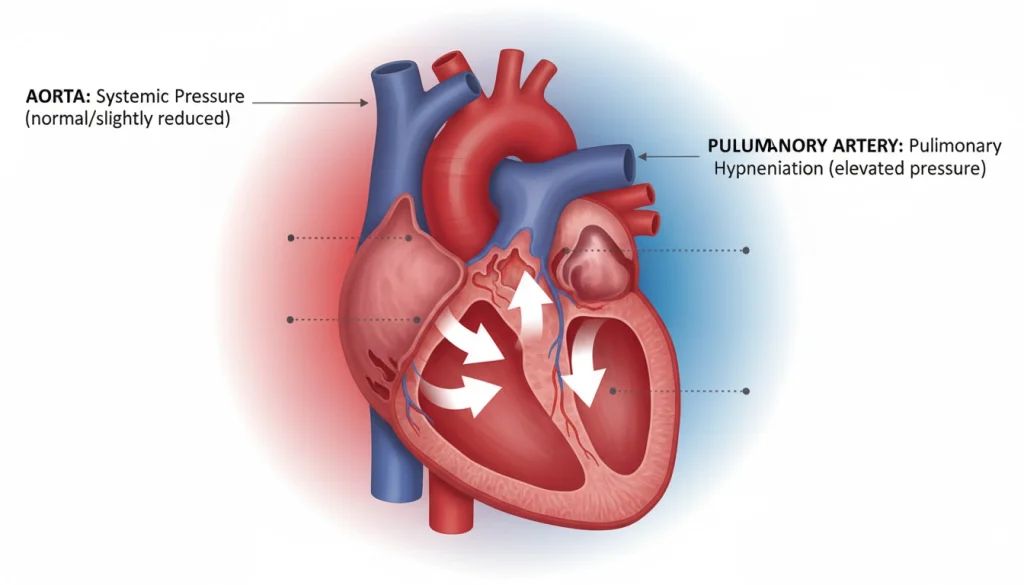
The size classification greatly influences treatment choices. Small defects might just need watchful waiting. But larger defects often require surgical or catheter-based interventions.
- Small VSDs: Watchful waiting
- Moderate VSDs: Monitoring and possible intervention
- Large VSDs: Surgical or catheter-based closure
Treatment Options for Infants and Children
Ventricular Septal Defect treatment in pediatric patients involves various medical and surgical approaches. The choice of treatment depends on several factors. These include the size of the defect, the presence of symptoms, and the child’s overall health.
Watchful Waiting Approach
For small VSDs without significant symptoms, a watchful waiting approach is sometimes adopted. This method involves regular monitoring with echocardiograms. It assesses the defect’s size and the heart’s function.
Medication Management
Medication is key in managing symptoms of VSD, such as heart failure. Diuretics help reduce fluid buildup. Other medications may improve heart function.
Surgical Closure Techniques
Surgical closure is often recommended for larger defects or those causing significant symptoms. This involves open-heart surgery. It can close the defect directly or use a patch.
Catheter-Based Procedures
Catheter-based procedures offer a less invasive option for some children. They involve using a catheter to deliver a device that closes the defect.
The decision on which treatment option to pursue is made on a case-by-case basis. A team of healthcare professionals works together. They determine the best course of action for each child’s unique needs.
Treatment Options for Adults
Managing Ventricular Septal Defect (VSD) in adults involves a detailed strategy. This includes both surgical and non-surgical methods. The treatment plan for adults with VSD varies. It depends on the defect’s size, symptoms, and the patient’s health.
Adult-Specific Considerations
Several factors are considered when treating adults with VSD. These include symptoms, defect size and location, and overall health. Adults with VSD may face complications like pulmonary hypertension or heart failure. These factors significantly influence the treatment approach.
Surgical Approaches in Adults
Surgical closure is an option for adults with significant symptoms or complications. The decision to operate is based on a detailed evaluation. This includes imaging studies and cardiac function assessment. Modern surgical techniques offer effective solutions with fewer complications.
Non-Surgical Management Strategies
Not all adults with VSD need surgery. Some can be managed without it. This includes monitoring symptoms and managing complications like arrhythmias or heart failure. Medications can help alleviate symptoms and improve quality of life.
In conclusion, treating VSD in adults requires a personalized approach. Each patient’s unique needs and circumstances are considered. Understanding the available treatments helps adults with VSD make informed decisions about their care.
Potential Complications and Long-Term Risks
A VSD can lead to serious heart problems over time. Without proper treatment, those with VSD face various long-term health risks.
Pulmonary Hypertension
Pulmonary hypertension is a severe complication of VSD. It happens when blood pressure in the pulmonary arteries increases. This can cause right heart failure.
Heart Failure
Heart failure is another risk for VSD patients. The heart works harder due to the defect. This can cause fatigue, shortness of breath, and swelling in the legs and feet.
Arrhythmias
Arrhythmias, or irregular heartbeats, can affect VSD patients. These can vary from mild to severe and may need medical treatment.
Endocarditis and Infection Risk
Those with VSD are more likely to get endocarditis, an infection of the heart lining. Good oral hygiene and possibly antibiotics before certain procedures are recommended.
Some major complications of VSD include:
- Pulmonary hypertension
- Heart failure
- Arrhythmias
- Endocarditis
It’s vital to understand these complications to manage VSD well and improve long-term health outcomes.
Recovery and Post-Treatment Care
The path to full recovery after VSD treatment is complex, involving immediate care and long-term monitoring. Effective strategies are key to achieving the best health outcomes and improving life quality for those with VSD.
Immediate Post-Operative Care
Immediate care after surgery is vital for managing pain, watching for complications, and ensuring the patient’s safety. Important steps include:
- Close monitoring of vital signs and cardiac function
- Pain management through medication
- Prevention of infection through antibiotics
Patients usually stay in the ICU for a while before moving to a regular room.
Long-Term Follow-Up Protocol
Long-term follow-up is critical for checking treatment success and managing long-term issues. The follow-up plan may include:
- Regular echocardiograms to assess heart function
- Cardiac MRI or CT scans as needed
- Monitoring for signs of pulmonary hypertension or other complications

Following the follow-up plan is essential for maintaining good health and addressing any issues quickly.
Living with VSD
Understanding ventricular septal defect (VSD) is key to navigating daily life with the condition. Those with VSD must be aware of possible complications. They should take steps to manage their health proactively.
Lifestyle Considerations and Limitations
Adjustments in lifestyle are often necessary for VSD management. These might include:
- Monitoring their overall health and reporting any changes to their healthcare provider
- Avoiding contact sports or activities that could lead to injury
- Maintaining a healthy diet and weight to reduce the risk of complications
Adopting these changes can help individuals with VSD avoid complications. It also enhances their quality of life.
Physical Activity Guidelines
Physical activity is vital for a healthy lifestyle, but those with VSD must adhere to specific guidelines. The permissible level of activity varies based on the defect’s size, presence of other heart conditions, and overall health.
Low-to-moderate intensity activities are generally advised. It’s critical for individuals with VSD to consult their healthcare provider before engaging in any exercise program.
Pregnancy and Family Planning with VSD
Pregnancy poses unique challenges for women with VSD, often compounded by other heart conditions or large defects. Pre-pregnancy counseling is vital to discuss pregnancy risks and plan.
Women with VSD should closely collaborate with their healthcare provider. This is to monitor their condition during pregnancy and address any complications that may arise.
Differences Between Pediatric and Adult VSDs
Understanding the differences between pediatric and adult VSDs is key for effective diagnosis and treatment. The basic defect is the same, but implications and management strategies vary significantly between these age groups.
Natural History and Progression
The natural history of VSDs differs between pediatric and adult populations. In children, small defects may close on their own, while larger ones often need intervention. Adults, on the other hand, may have had their VSDs treated earlier, but some remain undiagnosed until adulthood. This can lead to complications like pulmonary hypertension.
- Spontaneous closure is more common in children.
- Adults may present with complications like pulmonary hypertension.
- The size of the defect influences the likelihood of spontaneous closure.
Treatment Approach Variations
Treatment approaches for VSDs vary between pediatric and adult populations. This reflects differences in their clinical presentation and underlying health. In children, treatment may include watchful waiting, medication, or surgery. Adults often require more complex management, including surgical or catheter-based closure, and consideration of associated conditions.
- Pediatric treatment often involves watchful waiting or medication.
- Adults may require more invasive procedures, such as surgical closure.
- Associated conditions in adults can complicate treatment.
Recent Advances in VSD Management
New developments in surgical and interventional procedures are transforming VSD treatment. These advancements are leading to better patient outcomes and a broader range of management options for Ventricular Septal Defects.
Innovative Surgical and Interventional Techniques
Minimally invasive surgery and hybrid procedures are becoming more common for VSD treatment. These methods offer several advantages, including shorter recovery times and less patient trauma.
Interventional cardiology has also made significant strides. Devices like occluders and plugs are now used to close VSDs without open-heart surgery.
Research Developments and Future Directions
Research is ongoing to develop new technologies and techniques for VSD management. This includes the creation of biodegradable devices and tissue engineering approaches.
The future of VSD management likely involves a more personalized approach. Treatments will be tailored to each patient’s unique needs and anatomy.
Navigating Life After VSD Diagnosis: Hope and Resilience
Receiving a Ventricular Septal Defect (VSD) diagnosis can drastically change one’s life, bringing uncertainty and worry about the future. Yet, thanks to modern medical advancements and treatment options, those with VSD can live full and meaningful lives.
Life post-VSD diagnosis is a journey of hope and resilience. It demands a deep understanding of the condition, strict adherence to treatment plans, and making lifestyle changes. These steps help prevent complications and enhance overall well-being.
Hope is key in managing life with VSD. It motivates individuals to stay optimistic, seek support from family and healthcare teams, and stick to their treatment plans. Resilience, on the other hand, helps cope with VSD’s challenges, like managing symptoms, undergoing surgeries, and adjusting to new realities.
By embracing hope and resilience, those with VSD can overcome hurdles and flourish. It’s vital to stay informed, seek support, and be proactive in managing the condition. With the right attitude and support, a brighter future awaits those with VSD.
FAQ
Q: What is a Ventricular Septal Defect (VSD)?
A: A Ventricular Septal Defect (VSD) is a congenital heart condition. It features an opening in the septum between the heart’s two ventricles. This opening allows blood to flow from one ventricle to the other.
Q: How common are VSDs?
A: VSDs are among the most common congenital heart defects. They occur in about 2-5 per 1000 live births.
Q: What are the symptoms of VSD?
A: Symptoms of VSD vary based on the defect’s size and the individual’s age. Infants may experience shortness of breath, fatigue, and poor feeding. Adults might have shortness of breath, fatigue, and palpitations.
Q: How is VSD diagnosed?
A: VSD diagnosis involves a physical examination, echocardiography, and other imaging tests. These include chest X-rays and cardiac catheterization.
Q: What are the treatment options for VSD?
A: Treatment for VSD depends on the defect’s size and the individual’s health. Options include watchful waiting, medication, surgical closure, or catheter-based procedures.
Q: Can VSD be treated in adults?
A: Yes, VSD can be treated in adults. The treatment approach may differ from that for children. It may involve surgical or non-surgical management strategies.
Q: What are the possible complications of VSD?
A: Possible complications of VSD include pulmonary hypertension, heart failure, arrhythmias, and endocarditis. These are among the risks.
Q: How can individuals with VSD manage their condition?
A: Individuals with VSD can manage their condition by following a healthy lifestyle. This includes regular exercise and a balanced diet. They should also work closely with their healthcare provider to monitor their condition and address any concerns.
Q: Can individuals with VSD participate in physical activity?
A: Individuals with VSD can participate in physical activity. They should follow guidelines provided by their healthcare provider. This ensures safe and healthy exercise habits.
Q: What are the considerations for pregnancy and family planning with VSD?
A: Women with VSD should discuss their condition with their healthcare provider when planning pregnancy. VSD can increase the risk of complications during pregnancy and childbirth.