Ventricular Tachycardia: What is Ventricular Tachycardia
Ventricular Tachycardia (VT) is a potentially life-threatening heart rhythm disorder. It is marked by a rapid heartbeat. This condition can be dangerous if not addressed promptly. VT occurs when the heart’s ventricles beat too quickly. This is often due to an underlying heart condition or damage. It disrupts the heart’s normal rhythm, posing serious health risks. Symptoms of VT include dizziness, shortness of breath, and chest pain. If left untreated, these symptoms can escalate into more severe complications. It’s critical to seek medical attention if experiencing any of these signs.
Treatment options for VT depend on the underlying cause. They may include medication, cardioversion, or implantable cardioverter-defibrillators (ICDs). Each method aims to restore a normal heart rhythm and prevent further complications. The heart’s rhythm is vital for its proper functioning. Ventricular Tachycardia disrupts this rhythm. It is a potentially life-threatening arrhythmia that starts in the ventricles, the heart’s lower chambers.
Definition and Basic Mechanism
VT is marked by a rapid heart rate, usually over 100 beats per minute. It involves three or more consecutive premature ventricular contractions. This can cause inadequate blood circulation and severe complications.
Normal Heart Rhythm vs. VT
A normal heart rhythm is kept by a precise electrical system. VT occurs when this system is disrupted, causing the ventricles to contract too quickly. This can stem from various factors, including structural heart diseases or electrical disturbances within the heart.
How It Differs from Other Arrhythmias
VT is unique due to its origin in the ventricles and its severe impact on blood circulation. This makes it different from other arrhythmias.
Comparison with Supraventricular Tachycardia
Supraventricular Tachycardia (SVT) starts above the ventricles, in the atria or the atrioventricular node. Unlike VT, SVT typically does not pose the same risk for severe complications or cardiac arrest. It’s important to understand the differences between VT and SVT for accurate diagnosis and treatment.
Types of Ventricular Tachycardia
Ventricular Tachycardia (VT) presents in several forms, each with unique characteristics. It’s vital for healthcare professionals to grasp these differences to accurately diagnose and treat VT.
Monomorphic Ventricular Tachycardia
Monomorphic VT is marked by a consistent QRS complex on the electrocardiogram (ECG). This indicates a single source or circuit for the arrhythmia.
Characteristics and ECG Patterns
The ECG of monomorphic VT displays uniform ventricular activation. Key traits include:
- A consistent QRS morphology
- Typically, a rate between 100 and 250 beats per minute
- Often linked to structural heart disease
Polymorphic Ventricular Tachycardia
Polymorphic VT is recognized by its changing QRS complex on the ECG. This suggests multiple sources or a shifting reentrant circuit.
Distinguishing Features
Polymorphic VT’s key features are:
- Variable QRS complex morphology
- Often linked to acute ischemia or electrolyte imbalances
- Can evolve into ventricular fibrillation
Torsades de Pointes
Torsades de Pointes is a polymorphic VT variant. It’s characterized by a “twisting” of the QRS complexes around the isoelectric line on the ECG.
Unique Presentation and Risks
Torsades de Pointes is usually tied to a prolonged QT interval. It can be triggered by various factors, including certain medications and electrolyte disturbances. The risks include:
- Syncope or sudden cardiac death
- Often necessitates urgent treatment to address the underlying cause
- May require specific interventions like magnesium sulfate administration
Common Causes of Ventricular Tachycardia
Understanding the causes of VT is key to effective treatment. Ventricular Tachycardia can stem from various conditions. Identifying the root cause is essential for management.
Structural Heart Disease
Structural heart diseases significantly contribute to VT. These conditions alter the heart’s anatomy, potentially disrupting its electrical activity.
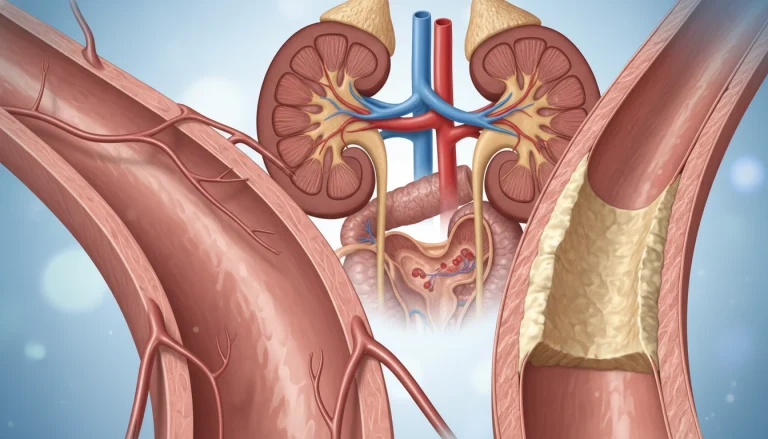
Coronary Artery Disease
Coronary artery disease is a major cause of VT. Narrowing or blockage of coronary arteries can lead to myocardial ischemia. This creates an environment conducive to arrhythmias.
- Reduced blood flow to the heart muscle
- Ischemia-induced electrical instability
- Increased risk of VT episodes
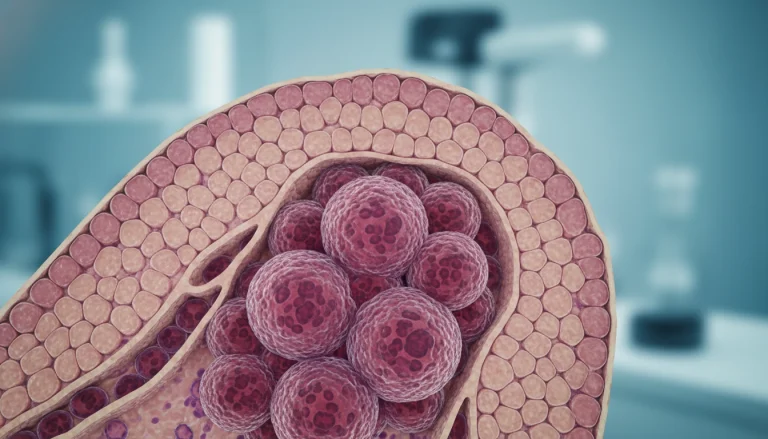
Myocardial Infarction and Scarring
Myocardial infarction, or heart attack, can lead to scarring in the heart muscle. This scarring disrupts the heart’s electrical pathways, potentially causing VT.
Post-Infarction VT
VT occurring after a myocardial infarction is a serious complication. The scarring from the infarct creates a substrate for reentrant arrhythmias.
- Scar tissue formation
- Electrical remodeling
- Increased susceptibility to VT
Cardiomyopathy
Cardiomyopathy refers to diseases of the heart muscle, which can lead to VT. Different types of cardiomyopathy have distinct effects on the heart’s structure and function.
Dilated, Hypertrophic, and Arrhythmogenic Types
Various forms of cardiomyopathy can contribute to VT, including dilated, hypertrophic, and arrhythmogenic right ventricular cardiomyopathy (ARVC).
- Dilated cardiomyopathy: Reduced heart function and increased risk of arrhythmias
- Hypertrophic cardiomyopathy: Thickened heart muscle and VT risk
- Arrhythmogenic right ventricular cardiomyopathy: Fatty replacement of heart muscle and high VT risk
Medication-Induced VT
Certain medications can induce VT, either as a direct effect or by interacting with other drugs.
Common Culprits and Mechanisms
Some medications increase VT risk, including certain antiarrhythmics, antibiotics, and antipsychotics. The mechanisms involve prolongation of the QT interval or direct effects on cardiac ion channels.
Risk Factors for Developing Ventricular Tachycardia
Understanding the risk factors for Ventricular Tachycardia is key to early detection and prevention. Several factors contribute to the likelihood of developing this condition. These include genetic predispositions, lifestyle choices, and pre-existing heart conditions.
Genetic Predisposition
Genetic factors significantly influence the risk of developing Ventricular Tachycardia. Those with a family history of heart conditions are more likely to experience VT.
Inherited Arrhythmia Syndromes
Inherited arrhythmia syndromes, like Long QT Syndrome and Brugada Syndrome, greatly increase VT risk. These conditions are often genetic and can be identified through specific diagnostic tests.
Lifestyle Factors
Lifestyle choices also impact VT risk. Factors such as diet, exercise, and substance use can affect heart health.
Impact of Diet, Exercise, and Substance Use
A diet high in saturated fats and sodium can contribute to heart disease, increasing VT risk. Regular exercise is beneficial but excessive physical stress can be harmful. Substance use, including alcohol and certain drugs, can trigger arrhythmias.
Pre-existing Cardiac Conditions
Pre-existing heart conditions are a significant risk factor for VT. Conditions that affect the heart’s structure or function can predispose individuals to arrhythmias.
Heart Failure and Valvular Disease
Heart failure and valvular disease are among the cardiac conditions that increase VT risk. These conditions can lead to electrical disturbances in the heart, potentially resulting in VT.
Recognizing the Symptoms of Ventricular Tachycardia
Understanding the symptoms of ventricular tachycardia (VT) is vital for timely medical intervention. VT can manifest through various symptoms, some of which may be subtle, while others are more pronounced.
Common Symptoms
Patients experiencing VT often report palpitations, which are sensations of irregular or forceful heartbeats. These palpitations can be unsettling and are a key symptom to recognize.
Palpitations and Chest Discomfort
Alongside palpitations, individuals may experience chest discomfort or pain, which can be a sign of the heart working under strain. This discomfort may feel like pressure or tightness in the chest area.
Warning Signs of an Episode
Before a VT episode occurs, some individuals may experience prodromal symptoms, which serve as warning signs.
Prodromal Symptoms
These symptoms can include dizziness, lightheadedness, or a general feeling of being unwell. Recognizing these signs can help in seeking medical attention before the condition worsens.
When to Seek Emergency Care
It’s critical to know when to seek immediate medical help. Certain red flags indicate a need for emergency care.
Red Flags for Immediate Medical Attention
- Severe chest pain or discomfort
- Shortness of breath
- Fainting or near-fainting spells
- Rapid or irregular heartbeat that doesn’t resolve on its own
Being aware of these symptoms and warning signs can be lifesaving. Prompt medical intervention can significantly improve outcomes for individuals experiencing VT.
Diagnostic Approaches for Ventricular Tachycardia
Diagnosing ventricular tachycardia (VT) demands a thorough strategy that employs various diagnostic tools. Accurate VT diagnosis is essential for effective management and treatment.
Electrocardiogram (ECG)
The electrocardiogram (ECG) stands as a primary diagnostic tool for VT, providing immediate insights into the heart’s rhythm.
Characteristic Findings
ECG findings characteristic of VT include a wide QRS complex tachycardia, exceeding 120 ms, with a rate between 140 to 250 beats per minute.
- A series of three or more consecutive premature ventricular complexes.
- Wide QRS complexes indicating ventricular origin.
- AV dissociation, capture beats, or fusion beats may be observed.
Holter and Event Monitors
For patients with intermittent symptoms, Holter and event monitors are invaluable for capturing VT episodes.
Capturing Intermittent Episodes
Holter monitors record the heart’s rhythm over 24 to 48 hours. Event monitors can be worn for longer periods, detecting less frequent arrhythmic events.
- Holter monitors provide continuous recording.
- Event monitors are activated by the patient during symptoms.
- Both are useful for correlating symptoms with arrhythmic events.
Electrophysiology Studies
Electrophysiology studies (EPS) are invasive tests that directly assess the heart’s electrical system, diagnosing VT.
Procedure and Diagnostic Value
During an EPS, catheters are guided to the heart to record electrical activity and induce VT under controlled conditions, providing valuable diagnostic information.
Cardiac Imaging
Cardiac imaging techniques, including MRI, CT, and echocardiography, are vital in identifying structural heart disease that may underlie VT.
Role of MRI, CT, and Echocardiography
These imaging modalities assess cardiac function, detect scar tissue, and evaluate the heart’s anatomy.

In conclusion, diagnosing ventricular tachycardia requires a multi-faceted approach. This involves ECG, Holter and event monitors, electrophysiology studies, and cardiac imaging. Each tool offers unique information essential for accurate diagnosis and management of VT.
Medical Treatment Options for Ventricular Tachycardia
Managing VT requires knowledge of various medical treatments, including drugs and emergency interventions. The choice of treatment varies based on VT’s cause, patient health, and symptom severity.
Antiarrhythmic Medications
Antiarrhythmic drugs are key in treating VT. They stabilize the heart rhythm and prevent arrhythmias.
Class I, III, and IV Agents
Class I drugs, like lidocaine, are used in acute settings. Class III agents, such as amiodarone, are effective for long-term management. Class IV agents, including verapamil, are used in specific cases.
- Lidocaine is effective for acute VT management.
- Amiodarone is used for long-term VT prevention.
- Verapamil can be considered for specific VT types.
Beta Blockers
Beta blockers are vital in VT management. They reduce heart rate and contraction force, lowering oxygen demand.
Mechanism and Efficacy
Beta blockers block epinephrine and norepinephrine effects on the heart, reducing arrhythmias. Their effectiveness in VT management is well-documented.
Calcium Channel Blockers
Calcium channel blockers are used in some VT cases, mainly when other treatments fail.
Indications and Limitations
These drugs are used when beta blockers are contraindicated or ineffective. Their use is limited by side effects and variable efficacy.
Emergency Medications
In acute VT episodes, emergency medications are critical. They include drugs that rapidly restore normal heart rhythm.
Acute Management Protocols
Acute management involves intravenous administration of drugs like lidocaine or amiodarone. Cardioversion or defibrillation may be necessary in severe cases.
- Administer oxygen and assess the patient’s airway, breathing, and circulation.
- Use cardiac monitoring to track the arrhythmia.
- Prepare for possible cardioversion or defibrillation.
Understanding these medical treatment options is essential for effective VT management and improved patient outcomes.
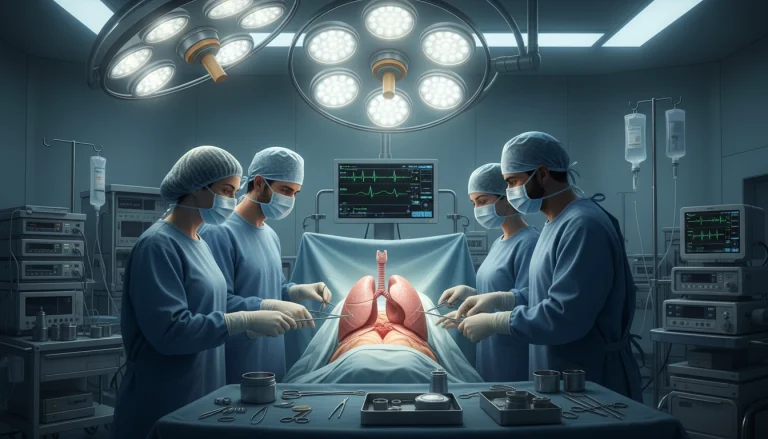
Interventional Procedures and Surgeries
For those with Ventricular Tachycardia, interventional procedures and surgeries are key treatment options. These methods are vital for managing VT and boosting patients’ quality of life.
Catheter Ablation
Catheter ablation is a minimally invasive method to treat VT by destroying abnormal heart electrical pathways. Ablation procedures have evolved, achieving high success rates for specific VT types.
Technique and Success Rates
The process uses catheters to map the heart’s electrical activity and pinpoint the arrhythmia source. Success rates vary based on the heart condition and VT type.
- Success rates are higher for patients with monomorphic VT.
- Some patients may need multiple procedures.
- Rare complications include bleeding or cardiac perforation.
Implantable Cardioverter Defibrillator (ICD)
An ICD is a device implanted under the skin to monitor the heart’s rhythm. It delivers an electric shock to restore a normal heartbeat during VT. ICDs are highly effective in preventing sudden cardiac death.
Device Selection and Programming
The choice and programming of an ICD depend on the patient’s condition, including VT type and heart disease. Proper programming is essential for the device’s effectiveness.
- Device type is chosen based on patient needs and anatomy.
- Programming is tailored to detect and treat VT appropriately.
- Regular follow-up is necessary to adjust settings as needed.
Surgical Ventricular Reconstruction
Surgical ventricular reconstruction is a more invasive procedure aimed at removing scar tissue causing VT. It’s typically considered for patients with significant scarring due to heart attacks.
Candidates and Outcomes
Candidates for this surgery often have a history of heart failure or significant scarring. Outcomes vary, but the goal is to reduce VT episodes and improve heart function.
- Improvement in VT episodes is possible.
- Surgery is often combined with other treatments like ICD implantation.
- Recovery time can be significant, requiring careful post-operative care.
Emergency Management of Ventricular Tachycardia
When ventricular tachycardia strikes, a swift and effective emergency response is essential. This potentially life-threatening arrhythmia demands immediate medical attention.
First Response Protocols
The initial steps in managing VT involve a thorough assessment of the patient’s condition. If the patient is unresponsive or showing severe symptoms, the first action is to call emergency services.
CPR and Defibrillation
Initiating CPR is necessary if the patient is unresponsive and not breathing. For patients in VT with no pulse, defibrillation is critical. An automated external defibrillator (AED) can greatly enhance survival chances by restoring a normal heart rhythm.

Hospital Emergency Procedures
Upon hospital arrival, patients with VT undergo treatment according to established emergency protocols. These protocols aim to stabilize the patient and address the arrhythmia’s underlying cause.
Stabilization and Acute Interventions
Stabilization may involve administering antiarrhythmic medications, cardioversion, or other interventions to restore a stable heart rhythm. Continuous monitoring is vital to quickly spot any changes in the patient’s condition.
Post-Emergency Care
Post-emergency care focuses on monitoring the patient for complications and preventing future episodes.
Monitoring and Follow-up
Ongoing monitoring includes regular check-ups and potentially further diagnostic testing to identify underlying conditions. Follow-up care is essential for optimizing long-term outcomes.
Living with Ventricular Tachycardia
Dealing with ventricular tachycardia can be tough, but the right approach makes it manageable. Understanding its effects on daily life is key. Making lifestyle changes helps mitigate its impact.
Lifestyle Modifications
Healthy choices are vital for managing VT. This includes a balanced diet, regular exercise, and stress control.
Diet, Exercise, and Stress Management
Eating heart-healthy foods like fruits, veggies, and whole grains is beneficial. Regular exercise, as advised by a doctor, boosts heart health. Stress-reducing activities like meditation or yoga help manage VT’s psychological effects.
Activity Restrictions and Recommendations
Ventricular tachycardia may limit some activities, but many can stay active. Knowing what activities are safe is important.
Work, Sports, and Daily Activities
Most with VT can work, adjusting to job demands as needed. For high-intensity sports, getting a doctor’s advice on safe levels is critical.
Psychological Impact
VT’s diagnosis can lead to anxiety and depression. Acknowledging these feelings is the first step to managing them.
Coping Strategies and Support Resources
Strategies like cognitive-behavioral therapy, support groups, and counseling offer emotional support. They help manage VT’s psychological aspects.
Complications and Long-term Prognosis
Understanding VT’s complications and long-term prognosis is key to effective management. VT can lead to severe, potentially life-threatening outcomes if not managed properly.
Potential Complications
VT is linked to several complications, including heart failure, cardiac arrest, and sudden cardiac death. The risk of these complications varies based on the underlying heart condition and VT episode frequency.
Sudden Cardiac Death Risk
Sudden cardiac death is a major concern for those with VT, more so for those with heart disease or previous cardiac events. The risk is higher in patients with conditions like coronary artery disease or cardiomyopathy.
Factors Affecting Prognosis
The prognosis for VT patients depends on several factors. These include the VT cause, presence of other heart conditions, and treatment effectiveness.
Predictors of Outcomes
Outcomes in VT are predicted by the left ventricular ejection fraction (LVEF), heart failure presence, and VT episode frequency and duration. Patients with lower LVEF or heart failure generally have poorer prognoses.
Survival Rates and Quality of Life
Survival rates for VT patients vary widely based on cause and other health conditions. Effective management can significantly improve survival rates and quality of life.
Long-term Management Success
Successful long-term VT management involves medication, lifestyle changes, and sometimes interventional procedures. Regular follow-ups with healthcare providers are essential to adjust treatments and monitor for complications.
Healthcare providers can develop effective management plans by understanding VT complications and prognosis factors. This improves outcomes for VT patients.
Prevention Strategies for Ventricular Tachycardia
To prevent ventricular tachycardia, a multi-faceted approach is necessary. This includes lifestyle changes and strict adherence to medication. By focusing on heart health and managing underlying conditions, individuals can lower their risk of VT.
Heart-Healthy Lifestyle
Adopting a heart-healthy lifestyle is key to preventing VT. It involves following nutrition and physical activity guidelines that promote cardiovascular health.
Nutrition and Physical Activity Guidelines
Eating a balanced diet, rich in fruits, vegetables, whole grains, and lean proteins, is essential. Regular physical activity, such as walking, cycling, or swimming, should be aimed for at least 150 minutes per week.
- Focus on consuming foods low in saturated fats, cholesterol, and sodium.
- Stay hydrated by drinking plenty of water.
- Limit alcohol intake to reduce heart stress.
Managing Underlying Conditions
Effectively managing underlying heart conditions is critical in VT prevention. This involves controlling heart disease risk factors through lifestyle adjustments and medical treatment.
Controlling Heart Disease Risk Factors
Monitoring and managing conditions such as hypertension, diabetes, and high cholesterol are vital. Working closely with healthcare providers to adjust treatment plans as needed is also important.
- Regularly check blood pressure and blood glucose levels.
- Adhere to prescribed medications for managing heart disease risk factors.
- Make lifestyle changes as recommended by healthcare providers.
Medication Compliance
Adhering to prescribed medication regimens is critical for VT prevention. Understanding the importance of medication compliance can help individuals stay on track with their treatment plans.
Importance of Adherence to Treatment Plans
Following the prescribed treatment plan helps in managing heart health and reducing the risk of VT episodes. It’s essential to understand the role of each medication and the consequences of non-adherence.

By integrating these prevention strategies into daily life, individuals can significantly reduce their risk of ventricular tachycardia and improve their overall heart health.
Future Directions in Ventricular Tachycardia Management
The management of Ventricular Tachycardia (VT) is undergoing significant changes. Ongoing research and technological advancements are set to enhance patient outcomes. The focus is on developing more effective and personalized treatment strategies.
New treatments, including novel antiarrhythmic medications and improved catheter ablation techniques, are being explored. Wearable cardioverter-defibrillators and remote monitoring systems are also gaining importance in VT care. These advancements aim to improve VT management.
Research into the genetic and molecular mechanisms of VT is vital. This research will uncover new therapeutic targets and enhance risk stratification for VT patients. As VT management evolves, patient outcomes are expected to improve, reducing complications and improving quality of life.
The future of VT management hinges on ongoing innovation and collaboration. Healthcare professionals, researchers, and industry leaders must work together. This collaboration will lead to more effective treatments and better care for VT patients.
FAQ
Q: What is Ventricular Tachycardia?
A: Ventricular Tachycardia is a heart rhythm disorder. It starts in the ventricles, causing the heart to beat too fast.
Q: What are the symptoms of Ventricular Tachycardia?
A: Symptoms include palpitations, chest discomfort, and dizziness. You might also feel lightheaded or have shortness of breath. In severe cases, it can cause loss of consciousness or cardiac arrest.
Q: How is Ventricular Tachycardia diagnosed?
A: Diagnosis involves an electrocardiogram (ECG) to check the heart’s rhythm. Other tests like Holter monitoring, event monitoring, and electrophysiology studies are also used.
Q: What are the treatment options for Ventricular Tachycardia?
A: Treatments include medications like antiarrhythmics and beta blockers. Calcium channel blockers are also used. Procedures like catheter ablation and implanting a cardioverter-defibrillator (ICD) are options too.
Q: Can Ventricular Tachycardia be prevented?
A: Preventing VT is not always possible. But, a heart-healthy lifestyle and managing heart conditions can reduce the risk. Sticking to medication regimens also helps.
Q: What is the prognosis for someone with Ventricular Tachycardia?
A: The prognosis varies based on the cause, heart disease, and treatment success. With proper care, many people with VT can live active lives.
Q: How does Ventricular Tachycardia affect daily life?
A: VT can require lifestyle adjustments, like avoiding certain activities and managing stress. With the right management and support, its impact can be minimized.
Q: What are the risks associated with Ventricular Tachycardia?
A: VT increases the risk of sudden cardiac death, heart failure, and other complications. Quick medical attention and proper treatment can reduce these risks.
Q: Can lifestyle changes help manage Ventricular Tachycardia?
A: Yes, making healthy lifestyle choices can help manage VT. A balanced diet, regular exercise, stress management, and avoiding triggers are key.