The Nature of Viral Infections
Viral infections pose a significant threat to global health, impacting millions. When a virus invades a host’s body, it starts to multiply, leading to various symptoms. This invasion disrupts normal bodily functions. The severity of viral infections can range from mild, like the common cold, to severe, such as HIV/AIDS. Grasping the causes, symptoms, and treatment options is essential. It helps in managing and preventing viral infections from spreading.
Learning about viral infections is vital for safeguarding our health and that of others. This knowledge is fundamental in crafting effective prevention and treatment plans. Understanding viral infections is key to creating effective treatments and prevention methods. These infections are caused by viruses, which differ from bacteria and other pathogens in structure, replication, and host interaction.
What Defines a Viral Infection
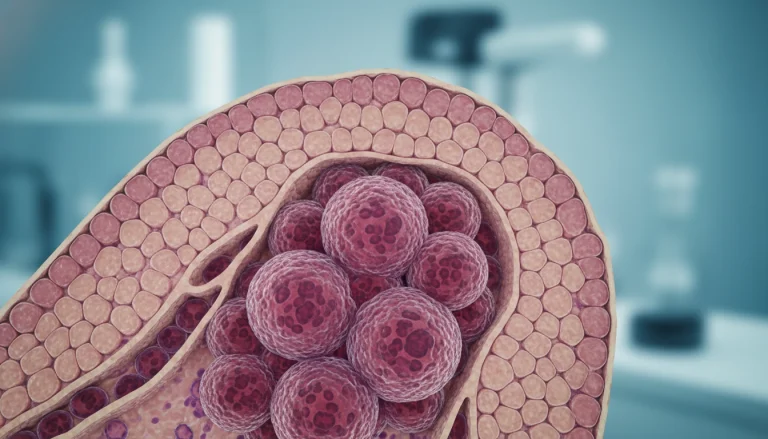
A viral infection happens when a virus invades a host cell, using its machinery to replicate. Viruses, being obligate parasites, cannot reproduce outside a host cell. They have genetic material, either DNA or RNA, wrapped in a protein coat called a capsid. Some viruses also have an outer lipid envelope.
The virus’s replication cycle includes several steps. These include attaching to and penetrating the host cell, replicating the viral genome, synthesizing viral proteins, and assembling and releasing new virus particles. This process can damage or kill host cells, leading to disease symptoms.
How Viruses Differ from Bacteria and Other Pathogens
Viruses are distinct from bacteria, which are single-celled organisms that can reproduce independently. Bacteria can also cause infections but through different mechanisms than viruses. Unlike viruses, bacteria are not obligate parasites and can often be treated with antibiotics.
- Viruses require a host cell to replicate, whereas bacteria can reproduce independently.
- The structure of viruses is distinct, with genetic material enclosed in a protein coat, whereas bacteria have cell walls and can be classified based on their Gram staining properties.
- Treatment approaches differ; antiviral medications are used for viral infections, while antibiotics are used for bacterial infections.
Understanding these differences is vital for diagnosing and treating infections effectively. By recognizing viruses’ unique characteristics and how they differ from other pathogens, healthcare professionals can develop targeted therapeutic strategies.
The Science of Viral Infection
Exploring the science behind viral infections uncovers the intricacies of viral behavior and how they interact with host cells. These infections are a major cause of illness and death globally. It’s critical to grasp the mechanisms driving them.
Viral Structure and Components
Viruses consist of genetic material, either DNA or RNA, encased in a protein shell called a capsid. Some viruses also have an outer lipid envelope. The viral genome harbors genes that encode proteins vital for replication and survival.
- Genetic Material: DNA or RNA that carries genetic information.
- Capsid: A protein shell that protects the viral genome.
- Envelope: A lipid layer derived from the host cell membrane, present in some viruses.
Viral Replication Cycle
The viral replication cycle includes several phases: attachment to and penetration of the host cell, uncoating of the viral genome, replication of viral genetic material, assembly of new viral particles, and release from the host cell.
- Attachment and Penetration: The virus binds to and enters the host cell.
- Uncoating: The viral genome is released from the capsid.
- Replication: The viral genome is replicated using host cell machinery.
How Viruses Evade Immune Detection
Viruses employ various tactics to evade the host immune system. These include antigenic variation, suppression of interferon responses, and inhibition of apoptosis. Such strategies allow viruses to remain within the host, leading to prolonged infections.
- Antigenic Variation: Changing surface proteins to avoid immune recognition.
- Immune Suppression: Interfering with the host’s immune response pathways.
Common Types of Viral Infections
It’s vital to grasp the various types of viral infections to craft effective treatments and prevention plans. These infections can impact different body systems, resulting in a multitude of diseases. By categorizing these infections, we gain insight into their health implications.
Respiratory Viral Infections
Respiratory viral infections target the respiratory system, causing symptoms from mild to severe. These infections are often highly contagious, spreading quickly.
Influenza and Common Cold
Influenza and the common cold are prevalent respiratory viral infections. Influenza can be severe, affecting vulnerable populations, while the common cold is typically mild but contagious.
COVID-19 and Other Coronaviruses
COVID-19, caused by SARS-CoV-2, has triggered a global pandemic. Other coronaviruses can cause mild to severe respiratory illness. This highlights the need to understand and manage coronavirus infections.
Gastrointestinal Viral Infections
Gastrointestinal viral infections impact the digestive system, leading to symptoms like diarrhea, vomiting, and abdominal pain. These infections are contagious and often spread through contaminated food or water.
Skin-Related Viral Infections
Skin-related viral infections can manifest as rashes and lesions. Viruses like herpes simplex cause recurring infections. Others, like varicella-zoster virus, lead to chickenpox and shingles.
Systemic Viral Infections
Systemic viral infections affect multiple organ systems, spreading throughout the body. These infections can be severe and require immediate medical attention.
HIV and AIDS
HIV infection can progress to AIDS if untreated. HIV weakens the immune system, making it harder to fight off infections and diseases.
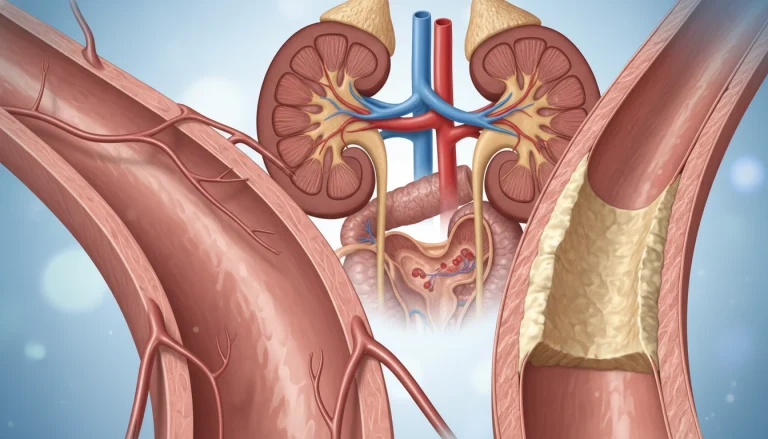
Viral Hepatitis
Viral hepatitis is inflammation of the liver caused by hepatitis viruses. Different types of hepatitis viruses exist, with varying transmission modes and acute or chronic infection risks.
How Viral Infections Spread
Viral infections spread through various routes, each with its own characteristics and risks. It’s vital to grasp these transmission methods to develop effective prevention and control strategies.
Airborne Transmission
Airborne transmission happens when viruses are released into the air through coughing, sneezing, or talking. These viruses are then inhaled by others. Examples include influenza and measles. To lower airborne transmission risks, wearing masks and maintaining social distancing are key.
- Influenza virus
- Measles virus
- Varicella-zoster virus
Direct Contact Transmission
Direct contact transmission involves physical contact with an infected person, like touching or shaking hands. Viruses like HIV and herpes simplex virus can spread this way. Good hygiene, such as frequent handwashing, is essential to prevent direct contact transmission.
- HIV
- Herpes simplex virus
- Human papillomavirus (HPV)
Foodborne and Waterborne Transmission
Foodborne and waterborne transmission happens when viruses are ingested through contaminated food or water. Norovirus and hepatitis A virus are examples. Proper food handling and water treatment can reduce these risks.
- Norovirus
- Hepatitis A virus
- Rotavirus
Vector-Borne Viral Transmission
Vector-borne transmission involves viruses spread through vectors like mosquitoes and ticks. Diseases like dengue fever and Zika virus are transmitted this way. Controlling vector populations and avoiding bites can prevent virus spread.
For more information on living with COVID-19, visit Acibadem International for guidelines and tips.
Recognizing Viral Infection Symptoms
Identifying symptoms of viral infections is essential for effective management and treatment. These infections can manifest differently, depending on the virus type and affected body part.
Common Symptoms Across Different Viral Infections
Many viral infections share common symptoms. These include fever, fatigue, and a general feeling of being unwell. Inflammation in the affected area often leads to pain or discomfort.
Some infections cause rashes or skin lesions, while others lead to respiratory symptoms like coughing or sneezing. The symptoms’ presence and severity vary among different infections.
Respiratory Viral Infection Symptoms
Respiratory infections, such as the common cold or flu, often present with coughing, sneezing, sore throat, and a runny nose. In severe cases, they can cause pneumonia or bronchitis.
Gastrointestinal Viral Infection Symptoms
Gastrointestinal infections typically cause nausea, vomiting, diarrhea, and abdominal cramps. These symptoms can lead to dehydration if not managed properly.
Systemic Viral Infection Symptoms
Systemic infections, which spread through the bloodstream and affect multiple systems, can cause a wide range of symptoms. These include fever, headache, muscle aches, and in severe cases, organ failure.
Understanding these symptoms is key to diagnosing and treating viral infections. Early recognition can lead to better outcomes and reduced risk of complications.
The Body’s Response to Viral Infection
When a viral infection strikes, the body springs into action. It employs a complex strategy to fight off the virus. This effort is vital to control the infection and protect the body’s cells and tissues.
Innate Immune Response
The innate immune response is the body’s initial defense against viruses. It offers immediate protection through physical barriers like the skin and mucous membranes. It also activates natural killer cells and produces interferons. These actions help contain the virus in the early stages.
This response is non-specific, reacting to any pathogen, not just viruses. Its broad nature is essential to give the adaptive immune response time to kick in.
Adaptive Immune Response
The adaptive immune response is a more targeted defense that develops over time. It involves T cells and B cells, which recognize and remember specific viral antigens. T cells kill infected cells or regulate the immune response. B cells produce antibodies that neutralize the virus, preventing further infections.
This response not only clears the virus but also provides long-term immunity against future infections by the same virus.
Inflammation and Fever as Defense Mechanisms
Inflammation and fever are key defense mechanisms against viral infections. Inflammation, marked by redness, swelling, and pain, isolates the infected area and promotes healing. Fever, or elevated body temperature, can slow virus replication and boost the immune response.
These mechanisms are vital in the body’s battle against viruses. They work alongside the innate and adaptive immune responses to safeguard the body and restore health.
Diagnosing a Viral Infection
Diagnosing viral infections requires a blend of clinical assessment and lab tests. Accurate diagnosis is key to effective treatment and preventing infection spread.
Clinical Evaluation Methods
Clinical evaluation starts the process of diagnosing viral infections. Healthcare professionals evaluate symptoms, medical history, and conduct physical exams. This initial step helps decide if further lab tests are needed.
Laboratory Testing Options
Laboratory tests are vital for confirming viral infection diagnoses. They help pinpoint the specific virus, essential for targeted treatments.
PCR and Antigen Testing
PCR testing is highly sensitive, detecting viral genetic material. Antigen testing looks for specific viral proteins. Both are essential for diagnosing acute viral infections.
Antibody Testing
Antibody testing, or serology, detects antibodies against specific viruses in the blood. It’s useful for identifying past infections or immunity to certain viruses.
Differentiating Viral from Bacterial Infections
Distinguishing between viral and bacterial infections is critical for proper treatment. Lab tests, like cultures and molecular diagnostics, aid in this differentiation. Clinical evaluation also plays a significant role.
Knowing if an infection is viral or bacterial directs the use of antibiotics and other treatments. This approach helps prevent antibiotic resistance and ensures effective care.
Treatment Approaches for Viral Infections
The treatment of viral infections involves various strategies, including antiviral medications and supportive care. It’s vital to understand these methods for effective management of viral infections.
Antiviral Medications and How They Work
Antiviral medications are key in treating viral infections. They target specific stages of viral replication, preventing the virus from multiplying. For example, drugs like oseltamivir (Tamiflu) and zanamivir (Relenza) combat influenza by blocking the neuraminidase enzyme on the virus’s surface. Acyclovir treats herpes simplex virus by disrupting viral DNA synthesis.
Antiviral resistance is a major concern, as it can reduce medication effectiveness. So, these drugs are used carefully, sometimes in combination with other treatments.
Supportive Care Strategies
Supportive care is essential in treating viral infections, focusing on symptom relief and aiding the body’s recovery. This includes rest, hydration, and nutrition. For respiratory infections, humidifiers and saline nasal sprays can ease congestion.
In severe cases, hospitalization may be needed for intravenous fluids, oxygen therapy, or other supportive treatments. These strategies are customized based on the infection’s symptoms and severity.
Over-the-Counter Remedies and Their Effectiveness
Over-the-counter (OTC) remedies are important for managing viral infection symptoms. For instance, OTC pain relievers like acetaminophen (Tylenol) and ibuprofen (Advil, Motrin) can lower fever and ease headaches and body aches.
Cough medicines and decongestants help with respiratory symptoms. But, it’s critical to use these remedies wisely and adhere to recommended dosages to avoid side effects.
Combining antiviral medications, supportive care, and OTC remedies can effectively manage viral infections and lower the risk of complications.
Preventing Viral Infections
Preventing viral infections is key to public health. It demands a broad approach. By applying effective prevention methods, people can lower their risk of getting viral infections.
Vaccination and Immunization
Vaccination is a top method to stop viral infections. Vaccines introduce a small, harmless virus piece or a weakened virus to the body. This triggers the immune system to create antibodies. These antibodies then fight the virus, giving immunity against future infections.
Immunization not only shields the individual but also boosts herd immunity. Herd immunity is vital for stopping viral infections in communities. With enough people immunized, outbreaks are less likely. This protects those who can’t get vaccines for health reasons.
Personal Hygiene Practices
Good personal hygiene is key to stopping viral infections. Washing hands often with soap and water, or using hand sanitizers when soap is not available, is essential. Also, avoid touching your face. Covering your mouth and nose with a tissue or elbow when coughing or sneezing stops viral particles from spreading.

Social Distancing and Isolation Measures
Social distancing and isolation are critical during viral outbreaks. Keeping a safe distance from others lowers the risk of contact with an infected person. Isolating those who are sick also stops the virus from spreading to others.
Environmental Controls and Disinfection
Environmental controls and disinfection are vital in preventing viral infections. Regularly cleaning high-touch surfaces and areas, like doorknobs and countertops, reduces virus presence. Good ventilation and clean air quality also help stop airborne viruses.
By using vaccination, hygiene, social distancing, and environmental controls, we can prevent viral infections. This keeps both individuals and communities healthy.
Viral Infection in Special Populations
It’s vital to grasp how viral infections impact special populations to craft effective treatments and prevention plans. These groups, due to age, health, or other factors, face a heightened risk of severe viral infection effects.
Children and Viral Infections
Children are highly susceptible to viral infections because their immune systems are in development. Respiratory viruses like RSV and influenza are common in this age group. Those with weakened immune systems, such as those with chronic illnesses or undergoing chemotherapy, are at a higher risk of severe illness.
Vaccination is key in shielding children from serious viral infections. Parents and caregivers must adhere to recommended vaccination schedules. This ensures children are safeguarded against vaccine-preventable diseases.
Elderly and Immunocompromised Patients
The elderly and immunocompromised individuals are at a heightened risk for severe viral infections. As people age, their immune systems naturally weaken, making them more susceptible to infections. Those with compromised immune systems, due to disease or treatment, also face increased risks.
Preventive measures such as vaccination and avoiding exposure to infection sources are critical for these populations. Healthcare providers often recommend annual influenza vaccinations and pneumococcal vaccinations to protect against serious infections.
Pregnant Women and Viral Infections
Pregnant women are considered a special population regarding viral infections. Pregnancy can alter the immune system, making women more susceptible to certain viral infections. Infections like influenza and COVID-19 can pose significant risks to both the mother and the fetus.
Pregnant women should take precautions to avoid infection. This includes practicing good hygiene, avoiding close contact with individuals who are sick, and following healthcare provider recommendations regarding vaccinations and antiviral treatments.
Complications of Untreated Viral Infections
Untreated viral infections can cause various complications with lasting effects. These issues can greatly reduce an individual’s quality of life. In severe cases, they can even be life-threatening.
Short-term Complications
Short-term complications from viral infections can occur during or shortly after the infection. These may include secondary bacterial infections, like pneumonia after influenza. They can also worsen existing health conditions, such as asthma or heart disease. In some cases, viral infections can cause acute conditions like myocarditis or encephalitis, which need immediate medical care.
The severity of these complications varies widely. It depends on factors like age, overall health, and the specific virus involved.
Long-term Health Effects
Some viral infections can have long-term health effects, even after the initial infection has resolved. For instance, certain viruses are linked to chronic conditions like hepatitis B and C. These can lead to liver cirrhosis or liver cancer over time. Other viruses may cause neurological conditions or persistent fatigue syndrome.
It’s important to understand the long-term effects of viral infections. This knowledge helps manage and mitigate these risks through proper medical care and lifestyle adjustments.
Post-Viral Syndromes
Post-viral syndromes are conditions that occur after a viral infection. They are characterized by persistent symptoms like fatigue, muscle pain, and cognitive difficulties. Examples include post-SARS syndrome and chronic fatigue syndrome. These can significantly affect an individual’s ability to function normally.
Research into post-viral syndromes is ongoing. The focus is on understanding their causes and developing effective treatments. This aims to improve the quality of life for those affected.
When to Seek Medical Attention for a Viral Infection
Viral infections demand prompt medical care, and knowing when to act is critical. While many can be managed with rest and hydration, some cases require immediate attention. Recognizing warning signs and red flags is essential for making informed health decisions.
Warning Signs and Red Flags
Several symptoms suggest a viral infection is worsening. These include:
- High fever lasting more than 3-4 days
- Difficulty breathing or shortness of breath
- Severe headache or stiff neck
- Confusion or disorientation
- Severe fatigue or weakness
Experiencing any of these symptoms calls for a healthcare professional’s evaluation.
Emergency Symptoms Requiring Immediate Care
Some symptoms are so severe they demand immediate medical care. These include:
- Chest pain or pressure
- Severe difficulty breathing
- Seizures or convulsions
- Severe abdominal pain
- Vomiting blood or bloody stools
If you or someone you know is experiencing these symptoms, immediate emergency medical care is essential.
Virtual vs. In-Person Medical Consultations
Today, both virtual and in-person consultations are available. For non-emergency cases, virtual consultations can be a convenient option. Yet, for severe symptoms or when a physical exam is needed, in-person visits are better.
Key Takeaways for Managing Viral Infections
Managing viral infections effectively involves a multi-faceted approach. This includes prevention, timely diagnosis, and appropriate treatment. It’s essential to grasp the nature of viral infections and their spread mechanisms. This knowledge is vital for developing effective strategies against them.
Preventive measures are the first line of defense. Vaccination, personal hygiene, and social distancing are key. Early recognition of symptoms and prompt medical intervention are also critical. These actions can greatly influence the outcome of infections.
Combining public health measures with individual actions is the cornerstone of successful management. Staying informed about viral infections and following recommended guidelines are essential. This way, individuals can significantly contribute to controlling viral infections and reducing their impact.
Managing viral infections is a collective responsibility. It demands awareness, education, and cooperation. By understanding the key takeaways from this article, individuals can better handle the challenges posed by viral infections.
FAQ
Q: What is a viral infection?
A: A viral infection happens when a virus enters the body and starts to multiply. This causes symptoms and can lead to health problems.
Q: How are viral infections different from bacterial infections?
A: Viral infections are caused by viruses, which are different from bacteria. Viruses need a host cell to replicate. Bacteria, on the other hand, can reproduce on their own.
Q: What are the common symptoms of a viral infection?
A: Symptoms of viral infections include fever, fatigue, headache, and muscle aches. The specific symptoms depend on the virus and the body part affected.
Q: How are viral infections diagnosed?
A: Diagnosing viral infections involves clinical evaluation, medical history, and lab tests. Tests like PCR, antigen testing, and antibody testing are used.
Q: What are the treatment options for viral infections?
A: Treatment for viral infections includes antiviral medications and supportive care like rest and hydration. Over-the-counter remedies can also help alleviate symptoms. The treatment depends on the virus and infection severity.
Q: Can viral infections be prevented?
A: Yes, preventing viral infections is possible. Vaccination, good hygiene, social distancing, and environmental controls like disinfection are effective.
Q: Are there any complications associated with untreated viral infections?
A: Untreated viral infections can cause complications. These include short-term issues like pneumonia and long-term effects like chronic fatigue syndrome. Post-viral syndromes are also possible.
Q: When should I seek medical attention for a viral infection?
A: Seek medical attention for severe symptoms, difficulty breathing, or if you’re at high risk for complications. Emergency symptoms need immediate care.
Q: How do antiviral medications work?
A: Antiviral medications target specific viral lifecycle stages. They inhibit replication or boost the immune response to the virus.
Q: Can viral infections affect certain populations more severely?
A: Yes, certain groups like children, the elderly, and those with weakened immune systems are more at risk. Pregnant women are also vulnerable due to their developing immune systems.