Why Is My Hip Replacement Hurting After 5 Years?
Feeling hip replacement pain after a few years can worry those who had hip replacement surgery. At first, the surgery is meant to reduce pain and boost movement. But, some people might feel long-term hip replacement discomfort. This makes them wonder why and how to fix it. It’s key to understand the cause of this pain to find a good solution. There are many reasons for pain after 5 years, like wear and tear, or the prosthesis loosening. It’s vital for patients to talk to their doctor to find out why.
Understanding Hip Replacement Surgery and Expected Outcomes
Hip replacement surgery, also known as hip arthroplasty, is a procedure to replace a damaged or arthritic hip joint. It aims to reduce pain, improve function, and enhance life quality for those with severe hip damage or arthritis.
What Happens During Hip Replacement Surgery
An orthopaedic surgeon makes an incision to access the hip joint during surgery. The damaged parts are then removed and replaced with artificial ones, usually made of metal, ceramic, or durable plastic. These prosthetics are designed to mimic the natural hip joint, ensuring smooth and pain-free movement.
For more detailed information on the surgical process, patients can visit specialized orthopaedic centres that provide detailed guides on hip replacement procedures.
Typical Recovery Timeline and Patient Expectations
The recovery time for hip replacement surgery varies, but most see significant improvements in the first few months. Patients typically start with hospitalization and then rehabilitation, which includes physical therapy to regain strength and mobility. Full recovery can take several months, with most patients returning to their normal activities within 3 to 6 months.
It’s important to manage expectations realistically. While the surgery can greatly improve life quality, it’s a major operation that requires patience during recovery.
- Immediate Post-Surgery: Pain management and initial rehabilitation
- Short-Term (0-3 months): Gradual return to daily activities
- Medium-Term (3-6 months): Continued improvement in strength and mobility
- Long-Term (6 months+): Full recovery and return to most activities
Average Lifespan of Modern Hip Implants
Modern hip implants are designed to be durable and long-lasting. They typically last between 15 to 20 years. Factors like the type of implant, patient activity levels, and overall health can influence this.
Advances in technology and materials have improved implant longevity. Some newer models are expected to last even longer. Regular follow-ups with an orthopaedic specialist are key to monitor the implant’s condition and address any issues early.
Is Pain After Five Years Normal or a Cause for Concern?
Pain after hip replacement surgery is common, but it’s important to know if it’s normal or a sign of a problem. Hip replacement aims to reduce pain and improve movement. But, how long the implant lasts and how well the body adapts can vary.
Distinguishing Between Normal Discomfort and Problematic Pain
Some pain is okay during recovery, but long-term pain might mean there’s an issue. Normal discomfort is usually mild and linked to how active you are or specific movements. On the other hand, problematic pain is more intense, doesn’t go away, and might be with swelling or feeling unstable.
Here’s how to tell normal pain from the kind that needs attention:
- Pain that gets worse over time
- Pain that makes daily tasks hard
- Pain with swelling, redness, or warmth around the hip
- Pain that’s sharp or severe, not just a dull ache
Characteristics of Pain That Warrant Medical Evaluation
Some pain signs need a doctor’s check-up. These include:
- Pain that lasts and doesn’t get better with rest
- Pain that makes you feel unstable or like your hip is giving way
- Pain with fever, chills, or other signs of infection
- Pain that’s so bad it stops you from doing daily things or keeps you awake

It’s key to understand your pain to know what to do next. If you’re feeling any of these symptoms, talk to your orthopaedic surgeon. They can check if there’s a problem.
Common Causes of Hip Replacement Pain Years After Surgery
Hip replacement pain can happen years after surgery. It’s important to know why this happens. This knowledge helps patients find relief from their pain.
Aseptic Loosening of the Prosthetic Components
Aseptic loosening means the hip replacement parts can move too much. This happens without any infection. It’s often due to how well the parts fit or how much stress they face.
Key factors contributing to aseptic loosening include:
- Poor initial fixation of the implant
- Mechanical stress and micromotion
- Osteolysis, or bone resorption, around the implant
Progressive Wear and Tear of Implant Materials
Hip replacement parts wear out over time. Modern implants are made to last, but they can degrade. The rate of wear depends on several factors.
These factors include how active the patient is, their weight, and the implant materials.
Late-Onset Periprosthetic Joint Infection
Periprosthetic joint infection (PJI) is a serious issue that can occur years after surgery. It’s rare but serious. Diagnosing and treating PJI is challenging.
Symptoms that may indicate PJI include:
- Persistent pain or swelling around the hip
- Redness or warmth around the surgical site
- Systemic symptoms like fever or malaise
Implant Dislocation and Instability Issues
Implant dislocation is another cause of pain. It happens when the prosthetic hip parts don’t fit right. This can lead to pain and discomfort.
Several factors can cause dislocation. These include:
- Wear and tear on the implant components
- Weakness or imbalance in the surrounding muscles
- Trauma or sudden injury to the hip
Prosthetic Component Wear and Material Degradation
Material degradation is a big worry for those with hip replacements. It can shorten the life of the implant. Wear and tear on prosthetic parts can cause problems, some needing more medical help.
Polyethylene Liner Deterioration Over Time
The polyethylene liner is key in many hip replacements. It acts as a soft cushion between the metal ball and the acetabular cup. But, over time, it can wear down due to friction, leading to:
- Osteolysis: Wear debris can cause inflammation, leading to bone loss around the implant.
- Increased risk of implant loosening: As the liner wears, the implant’s stability can be at risk.
Metal-on-Metal Bearing Surface Complications
Metal-on-metal hip replacements were once seen as durable. But, they’ve been linked to serious issues, including:
- Metallosis: Metal ions can get into the blood and tissues, causing damage and reactions.
- Pseudotumors: Soft tissue masses or cysts can form around the hip, causing pain and needing surgery.
It’s vital for patients with metal-on-metal implants to get regular checks for complications.
Ceramic Component Fractures and Squeaking
Ceramic parts are used in some hip replacements because they’re hard and wear-resistant. But, they come with risks:
- Fracture risk: Ceramic parts can break under stress, needing surgery to fix.
- Squeaking: Some with ceramic-on-ceramic hip replacements might hear squeaks or noises, causing worry.
Knowing about the risks of prosthetic wear and material degradation is key for hip replacement patients. Regular check-ups with an orthopaedic specialist are important for catching and managing these problems early.
Periprosthetic Infection as a Late Complication
Periprosthetic joint infection is a serious late complication of hip replacement. It happens when bacteria infect the tissue around the artificial hip. This infection is hard to diagnose and treat, often needing long-term antibiotics or surgery.
Recognising Symptoms of Deep Joint Infection
It’s important to spot the signs of deep joint infection early. Look out for ongoing pain, swelling, redness, and warmth in the hip. You might also feel feverish, have chills, or just not feel right. A sinus tract or wound drainage can also be a sign of a serious infection.
Key symptoms to watch for:
- Persistent pain or discomfort
- Swelling or redness around the hip
- Fever or chills
- Wound drainage or sinus tract formation
How Bacterial Infections Develop Years Post-Surgery
Bacterial infections can appear years after hip surgery. They can spread through the blood from another infection, or during surgery. They can also spread from nearby tissues.
Knowing how these infections start helps in preventing them. People with weak immune systems or chronic infections are at higher risk.
Patient Risk Factors for Delayed Infection
Some factors make patients more likely to get periprosthetic joint infection years later. These include:
- Rheumatoid arthritis or other inflammatory conditions
- Diabetes or other metabolic disorders
- Obesity or malnutrition
- Previous infections or compromised immune status
Knowing these risk factors helps doctors keep a closer eye on high-risk patients. They can then take steps to prevent late complications.
Implant Loosening and Osteolysis
It’s important to know why implants might loosen or cause osteolysis. These issues can affect how long an implant lasts and its success. Proper aftercare is key.
Understanding Aseptic Loosening Mechanisms
Aseptic loosening means the implant moves without infection. It can happen for many reasons, like too much stress or poor bone attachment. The main reason is when the bone and implant don’t bond well, causing the implant to move.
Things like bone quality and how active you are can play a part. So does how the surgery is done and the type of implant. Knowing these helps lower the risk of loosening.
Osteolysis and Progressive Bone Loss
Osteolysis is when bone around the implant wears away. This often happens because of debris from the implant. This bone loss can make the implant unstable, possibly needing a new surgery.
Debris from the implant and the body’s reaction to it cause osteolysis. Choosing the right implant materials and design is important to reduce wear and osteolysis risk.

Clinical Signs That Your Implant May Be Loose
Spotting signs of implant loosening early is vital. Look out for hip or groin pain, feeling unstable, or the implant moving. Also, if you find it harder to move or feel more pain when doing things, it might be a sign.
Scans like X-rays or CT scans can show if the implant is loose. Seeing an orthopaedic specialist regularly is important. They can check the implant and fix any problems quickly.
Why Is My Hip Replacement Hurting After 5 Years: Mechanical Complications
It’s important to understand the mechanical issues that can cause hip replacement pain. These problems come from how the prosthetic parts work with the bone and soft tissue around them.
Femoroacetabular Impingement Between Components
Femoroacetabular impingement (FAI) happens when the femoral head and acetabular cup rub against each other. This can cause pain and make it hard to move. The rubbing can also wear down the parts, leading to bigger problems if not fixed.
Leg Length Discrepancy and Biomechanical Effects
Leg length differences can happen after hip replacement surgery. This can mess up how you walk and put strain on your back and other joints. Using shoe lifts or surgery might be needed to fix the leg length and ease pain.
Muscle Weakness and Soft Tissue Irritation
Weak muscles and irritated soft tissues are common after hip replacement. Weak hip muscles can make your gait abnormal and put more stress on the joint. Physical therapy can help strengthen the muscles and reduce irritation, making you feel better and move easier.
Non-Implant Related Sources of Hip Pain
After hip replacement surgery, patients might feel hip pain from different reasons. These reasons are not because of the implant itself. Knowing these causes helps manage pain better and improves life quality.
Osteoarthritis in Adjacent Joints
Osteoarthritis can happen in joints near the replaced hip. It causes pain and stiffness. This happens because the joint cartilage wears out over time.
- Symptoms: Pain, stiffness, and limited mobility in the affected joint.
- Management: Treatment options include physical therapy, pain relief medications, and lifestyle modifications.
Trochanteric Bursitis and Tendon Inflammation
Trochanteric bursitis is inflammation near the hip joint. It causes pain on the outer hip. Tendon inflammation also leads to hip pain.
Causes:
- Overuse or repetitive strain on the hip tendons.
- Trauma or injury to the hip area.
Lumbar Spine Conditions Causing Referred Pain
Lumbar spine issues, like herniated discs or spinal stenosis, can cause hip pain. This pain is felt in areas other than the actual problem.
Common Lumbar Spine Conditions:
- Herniated discs.
- Spinal stenosis.
- Degenerative disc disease.
Pelvic and Sacroiliac Joint Dysfunction
Dysfunction in the pelvic or sacroiliac joints can also cause hip pain. These joints support the spine and help with movement.
- Symptoms: Pain in the lower back, hip, or buttock area.
- Treatment: May include physical therapy, joint injections, or other interventions aimed at reducing pain and improving joint function.
Patients with hip pain after hip replacement should talk to their healthcare provider. They need to find out the cause and get the right treatment.
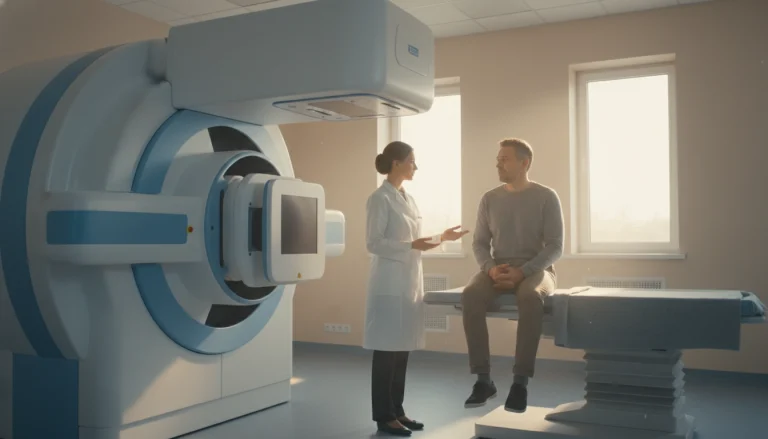
Diagnostic Procedures and Clinical Evaluations
To find the cause of hip replacement pain after five years, a detailed approach is needed. A thorough check is key to pinpoint the pain’s source and choose the right treatment.
Comprehensive Physical Examination Techniques
A detailed physical check is the first step in diagnosing hip pain. It looks at how the patient walks, moves, and what triggers pain. Specific tests, like the hip flexion test and the log roll test, help find pain sources. The doctor also checks for swelling, redness, or warmth, signs of infection or inflammation.
Radiological Imaging: X-rays, CT Scans, and MRI
Imaging is key in finding hip pain causes. X-rays are often the first choice, showing if parts are loose, worn, or broken. CT scans give more detailed views, useful for checking bone and implant connections. MRI, despite challenges with metal implants, helps with soft tissue issues.
Laboratory Blood Tests for Inflammatory Markers
Blood tests are vital for spotting infection or inflammation signs. CRP and ESR tests are common to find inflammatory markers, hinting at joint infection. High levels mean more tests are needed.
Hip Aspiration and Synovial Fluid Analysis
When infection is suspected, hip aspiration and fluid analysis are essential. This involves taking fluid from the hip joint for lab tests. The fluid is checked for infection signs and cultured to find bacteria.
Treatment Approaches for Long-Term Hip Replacement Pain
Managing long-term hip replacement pain requires looking at different treatment options. The right choice depends on the pain’s cause, the patient’s health, and their wishes.
Conservative Non-Surgical Management Options
For many, starting with non-surgical treatments is best. This includes lifestyle changes like losing weight, doing gentle exercises, and avoiding painful activities.
- Physical therapy to improve joint mobility and strength
- Using assistive devices like canes or walkers to reduce stress on the hip
- Making adjustments to daily activities to minimise discomfort
Pharmaceutical Pain Management Strategies
If non-surgical methods don’t work, medicines might be needed. This could be nonsteroidal anti-inflammatory drugs (NSAIDs), painkillers, or corticosteroid injections to cut down inflammation and pain.
Physical Therapy and Targeted Rehabilitation
Physical therapy is key in keeping the hip working well and easing pain. A customised rehab plan can boost movement, muscle strength, and overall mobility.

Revision Hip Replacement Surgery Considerations
If pain is caused by a problem like implant loosening or wear, revision hip replacement surgery might be needed. This choice is made after checking other options first.
Choosing to have revision surgery is a big decision. It’s important to weigh the benefits and risks. Patients should talk about their options with their orthopaedic surgeon.
Preventative Measures and Long-Term Hip Care
Looking after your hip after surgery is key to its success. It’s not just about the first few weeks. Taking care of your hip long-term can make it last longer and work better.
Maintaining Optimal Body Weight for Joint Health
Keeping a healthy weight is important for your hip. Too much weight can wear out your new hip faster. Eating well and staying active can help you keep a good weight.
Eating right and avoiding too much weight helps your hip stay healthy. It also means less stress on your new hip.
Appropriate Exercise Programmes and Activity Modifications
Doing the right exercises is key for keeping your hip healthy. Swimming, cycling, and brisk walking are good. They keep your heart healthy without putting too much strain on your hip.
- Swimming: A low-impact exercise that promotes flexibility and strength without stressing the hip joint.
- Cycling: Enhances cardiovascular fitness and leg strength.
- Brisk Walking: Improves cardiovascular health and maintains mobility.
It’s also important to avoid activities that could harm your new hip. Stay away from high-impact sports and heavy lifting.
Importance of Regular Orthopaedic Follow-Up
Seeing your orthopaedic specialist regularly is very important. It helps keep an eye on your hip and catch any problems early. This way, you can fix things before they get worse.
Regular check-ups let doctors check how your hip is doing. They can make any needed changes or give advice for keeping your hip healthy.
Early Recognition of Warning Signs
Knowing the signs of trouble with your hip is important. If you have pain, swelling, or feel unstable, tell your doctor right away.
- Monitor for persistent pain that doesn’t improve with rest.
- Watch for signs of swelling or redness around the hip.
- Report any feeling of instability or dislocation.
Spotting and acting on these signs early can really help. It can make a big difference in how well your hip works.
When to Contact Your Orthopaedic Surgeon Urgently
People with a hip replacement need to know when to call their orthopaedic surgeon. This is to get help quickly.
Red Flag Symptoms Requiring Immediate Assessment
Some symptoms mean you should see a doctor right away. These include:
- Severe pain that doesn’t go away with rest or medicine
- Swelling or redness around the hip that gets worse or is very bad
- Instability or feeling like your hip might break
- Fever or chills, which could mean an infection
- Difficulty walking or putting weight on the affected leg

Emergency Situations and Acute Complications
Some hip replacement patients face serious problems that need quick help. These include:
- Fractures or dislocations of the hip
- Signs of deep vein thrombosis (DVT), like leg swelling or pain
- Neurovascular issues, shown by numbness, tingling, or coldness in the leg
Preparing Information for Your Medical Consultation
Before you call your orthopaedic surgeon, have this info ready:
- Tell them about your symptoms, when they started, and what makes them better or worse
- Share any recent changes in your health or medicines
- Bring any test or imaging results from before
Knowing the red flag symptoms and when to get urgent help is key. This way, hip replacement patients can get the care they need fast.
Conclusion
Hip replacement pain after 5 years can worry those who have had the surgery. It’s important to know why this pain happens. Factors like wear on prosthetics, infections, and mechanical issues can cause it.
Dealing with hip replacement pain needs a full plan. This includes tests, doctor checks, and treatments. Working with an orthopaedic surgeon is key to finding and fixing the pain’s cause. For pain from other conditions, like facet joint syndrome, https://acibademinternational.com/facet-joint-syndrome/ is a good place to start.
Knowing why hip replacement pain happens helps manage it better. Regular doctor visits and a healthy lifestyle are important. This way, people can feel better and live better lives.
FAQ
Q: Why is my hip replacement hurting after 5 years?
A: Hip replacement pain after 5 years can be due to several reasons. These include aseptic loosening, wear and tear, infection, or mechanical issues. It’s important to see an orthopaedic surgeon to find out why.
Q: Is it normal to experience some discomfort after hip replacement surgery?
A: Yes, some discomfort is normal when you’re recovering. But, if you’re experiencing persistent or severe pain after 5 years, it’s not usual. You should look into it further.
Q: What are the common causes of hip replacement pain years after surgery?
A: Common causes include aseptic loosening and wear and tear of implant materials. Other causes are late-onset periprosthetic joint infection and issues with implant dislocation or instability.
Q: How is hip replacement pain diagnosed?
A: Diagnosis involves a thorough physical examination and radiological imaging like X-rays, CT scans, or MRI. Blood tests for inflammatory markers and hip aspiration and synovial fluid analysis may also be done.
Q: What are the treatment options for long-term hip replacement pain?
A: Treatment options include non-surgical management and pain management strategies. Physical therapy and targeted rehabilitation are also considered. In some cases, revision hip replacement surgery may be necessary.
Q: Can I prevent hip replacement pain after 5 years?
A: While some factors are unavoidable, you can reduce the risk. Maintaining a healthy weight, exercising correctly, and attending regular follow-up appointments with your orthopaedic surgeon can help.
Q: When should I contact my orthopaedic surgeon urgently?
A: If you have sudden severe pain, swelling, or instability, contact your orthopaedic surgeon urgently. Also, if you have concerns about your hip replacement, don’t hesitate to reach out.
Q: What are the signs of a problem with my hip replacement?
A: Signs include increasing pain, swelling, instability, or a feeling of looseness in the hip. If you notice any of these symptoms, seek medical attention.
Q: How can I manage my hip replacement pain?
A: Management strategies include pain relief medication, physical therapy, and lifestyle changes. Your orthopaedic surgeon can advise on the best approach for your situation.