Testicular Cancer: What is Testicular Cancer
Testicular cancer is a rare form of cancer that impacts the testicles, a vital part of the male reproductive system. It’s essential to grasp this condition to ensure early detection and effective treatment. This detailed guide delves into testicular cancer, covering its risk factors, symptoms, diagnosis, and treatment choices. By learning about it, individuals can better understand the diagnosis and treatment process. This knowledge is key to improving outcomes.
Early detection is critical for successfully treating testicular cancer. This guide aims to educate and reassure those affected. It provides a clear understanding of what to expect and how to manage the condition. Testicular cancer is a rare form of cancer that starts in the testicles. It’s the most common cancer in men aged 15 to 35. Understanding this cancer is key to its management.
Definition and Basic Concepts
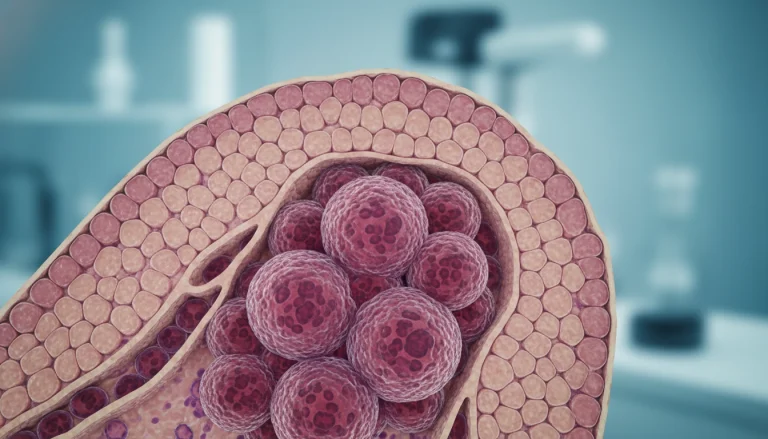
It happens when cells in the testicles grow out of control. The testicles produce sperm and testosterone. While the exact cause is unknown, certain factors can increase a man’s risk.
Types of Testicular Cancer
There are two main types: seminomas and non-seminomas. Each type has unique characteristics and treatment responses.
Seminomas
Seminomas grow slowly and are often treated with radiation. They appear uniform and are less aggressive than non-seminomas.
Non-Seminomas
Non-seminomas are aggressive and diverse, including subtypes like embryonal carcinoma. They grow faster and are more likely to spread.
Prevalence and Statistics in the United States
Testicular cancer is rare, making up 1% of male cancers. The American Cancer Society estimates 9,300 new cases annually. It’s most common in men 15 to 35, but early detection significantly increases cure rates.
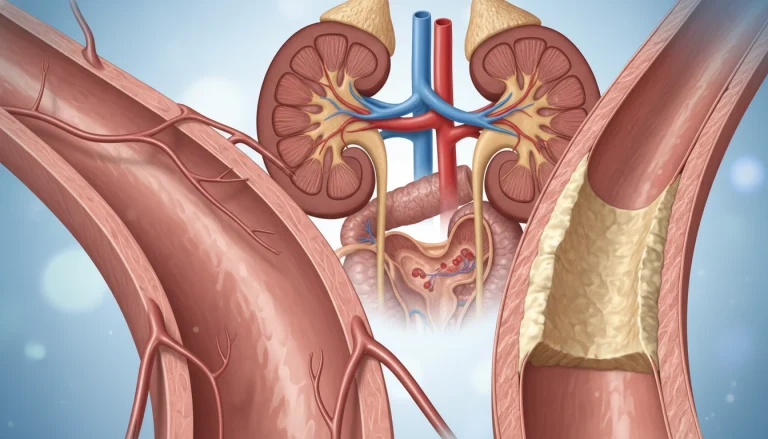
Anatomy and Physiology of the Testicles
To grasp testicular cancer, we must first understand the testicles’ normal anatomy and physiology. These oval-shaped organs are vital for male reproduction, producing sperm and hormones like testosterone. They are located in the scrotum, a sac that protects them and maintains the ideal temperature for sperm production.
Normal Testicular Function
The testicles are oval-shaped organs located inside the scrotum, a sac of skin and muscle that provides them with protection and the optimal temperature for sperm production. Normal testicular function involves the production of sperm through a process called spermatogenesis, which occurs within the seminiferous tubules of the testes.
They also produce hormones essential for male development and fertility. Testosterone, the primary male sex hormone, is produced by the Leydig cells in the testicles. It plays a key role in the development of male reproductive organs, secondary sexual characteristics, and the maintenance of libido.
How Cancer Develops in Testicular Tissue
Testicular cancer typically originates in the germ cells, which are the cells responsible for producing sperm. The exact cause of testicular cancer is not fully understood, but it is believed to begin with a genetic mutation in a germ cell. This mutation leads to uncontrolled cell growth and tumor formation.
There are several types of testicular cancer, with seminoma and non-seminoma being the most common. Seminomas are cancers that arise from the germ cells and tend to grow more slowly. Non-seminomas are more aggressive and can include several subtypes, such as embryonal carcinoma and choriocarcinoma.
The Role of Testicles in Male Health
Beyond their role in reproduction, the testicles play a significant part in overall male health through the production of testosterone. This hormone influences a range of bodily functions, including bone density, muscle mass, and red blood cell production.
Understanding the normal function of the testicles and how cancer can develop in these organs is critical. It is essential for early detection and effective treatment of testicular cancer.
Risk Factors for Testicular Cancer
The exact cause of testicular cancer is not fully understood. Yet, several risk factors have been identified. These factors can increase a man’s chance of developing this disease. It’s vital to understand these risks to identify high-risk individuals early.
Age and Demographic Factors
Testicular cancer predominantly affects young and middle-aged men, typically between 15 and 35 years old. It can, though, occur at any age. White men are more likely to develop testicular cancer compared to men of other races.
Genetic Predisposition
Genetics significantly influence the risk of testicular cancer. Men with a family history of the disease are at higher risk. This suggests a genetic link.
Environmental Risk Factors
Exposure to certain environmental factors may increase testicular cancer risk. Yet, more research is needed to fully grasp their impact.
Medical Conditions Associated with Increased Risk
Certain medical conditions can elevate a man’s risk of testicular cancer. Two notable conditions are discussed below.
Cryptorchidism (Undescended Testicle)
Cryptorchidism, or undescended testicle, occurs when one or both testicles fail to descend into the scrotum. Men with a history of cryptorchidism face a higher risk of testicular cancer. 
Family History
A family history of testicular cancer is another significant risk factor. Men with a father or brother who has had testicular cancer are at increased risk. This suggests a possible genetic component to the disease.
Signs and Symptoms of Testicular Cancer
Recognizing the signs and symptoms of testicular cancer is vital for early detection and effective treatment. This cancer often presents through specific changes in the testicles or surrounding areas.
Early Warning Signs
Early signs of testicular cancer include a painless lump or swelling in the testicle. You might also feel a sense of heaviness in the scrotum or a dull ache in the lower abdomen or groin. It’s important for men to watch for any changes in their testicles. Early detection can significantly improve treatment outcomes.
- A lump or swelling in the testicle
- Pain or discomfort in the testicle or scrotum
- A feeling of heaviness in the scrotum
Advanced Symptoms
As testicular cancer progresses, symptoms become more pronounced. Advanced symptoms include pain in the testicle or scrotum, indicating tumor growth. You might also notice a sudden collection of fluid in the scrotum or sudden pain.
Symptoms of Metastatic Disease
When testicular cancer metastasizes, symptoms can appear in other parts of the body. These may include back pain, shortness of breath, or swelling in the neck due to lymph node metastasis. Recognizing these symptoms is critical for understanding the disease’s extent.
When to Seek Medical Attention
Seeking medical attention is essential if you notice any unusual symptoms or changes in the testicles. Early evaluation by a healthcare professional can lead to timely diagnosis and treatment. Men should not hesitate to consult a doctor if they observe any persistent or unusual testicular changes.
Prompt medical evaluation is key to effectively addressing testicular cancer. By being aware of the signs and symptoms and seeking medical care when necessary, men can significantly improve their chances of successful treatment.
Testicular Self-Examination
Testicular self-examination is a simple yet effective method for detecting testicular cancer early. By incorporating this practice into their routine, men can significantly improve their chances of identifying any abnormalities at an early stage.
Importance of Regular Self-Exams
Regular testicular self-exams are critical for early cancer detection. This practice allows men to become familiar with their testicles’ normal appearance and feel. It makes it easier to notice any changes or abnormalities.
Early detection is key to effective treatment and improved survival rates. Men are encouraged to perform self-exams monthly, ideally after a warm shower or bath when the testicles are most relaxed.
Step-by-Step Guide to Self-Examination
To perform a testicular self-exam, follow these steps:
- Hold the scrotum in the palm of your hand and gently feel the testicle.
- Notice the epididymis, a cord-like structure at the back of the testicle, which is normal.
- Gently roll the testicle between your thumb and fingers to check for any lumps, swelling, or irregularities.
- Repeat the process for the other testicle.
What to Look For During Self-Exams
During a self-exam, men should look for any changes in the size, shape, or consistency of their testicles. Signs that may indicate a problem include:
- A lump or swelling on the testicle.
- Pain or discomfort in the testicle or scrotum.
- A feeling of heaviness in the scrotum.
Common Misconceptions About Testicular Abnormalities
One common misconception is that testicular cancer always causes pain. While pain can be a symptom, many cases are initially painless. Another misconception is that only men with a family history are at risk. While having a family history can increase risk, many men without a known family history can also develop testicular cancer.
By understanding these facts and performing regular self-exams, men can take proactive steps towards their health. They can potentially catch any issues early.
Diagnosis and Staging of Testicular Cancer
The journey to diagnose testicular cancer involves several steps. These include initial medical evaluations, diagnostic tests, and staging procedures. Accurate diagnosis and staging are key to finding the right treatment and understanding the prognosis.
Initial Medical Assessment
The first step is a detailed medical history and physical exam. The healthcare provider will ask about symptoms, risk factors, and past medical conditions. They will also perform a physical check of the testicles for any abnormalities.
Diagnostic Tests and Procedures
Several tests are used to confirm testicular cancer and determine its type and stage.
Ultrasound
An ultrasound is often the first imaging test for a testicular mass. It helps distinguish between solid tumors and other conditions like cysts or epididymitis.
Blood Tests for Tumor Markers
Blood tests measure tumor markers like alpha-fetoprotein (AFP), human chorionic gonadotropin (hCG), and lactate dehydrogenase (LDH). High levels of these markers suggest testicular cancer.
Imaging Studies
CT scans or MRI may follow to check if the cancer has spread to other areas of the body.

The TNM Staging System for Testicular Cancer
The TNM staging system classifies testicular cancer based on tumor size and spread. It considers the main tumor (T), nearby lymph nodes (N), and metastasis (M). This system aids in predicting outcomes and guiding treatment.
Understanding Your Diagnosis
Receiving a testicular cancer diagnosis can be daunting. It’s vital to talk with a healthcare provider about the diagnosis, stage, and treatment options. This understanding is essential for making informed decisions.
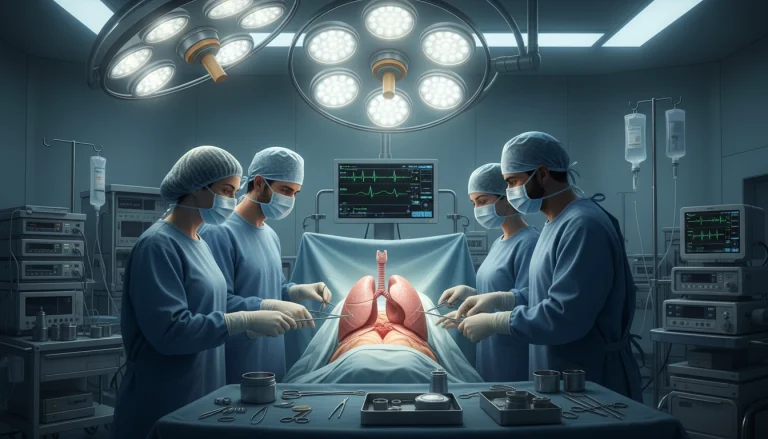
Treatment Options for Testicular Cancer
Patients facing testicular cancer have various treatment paths, each with its own merits and challenges. The choice hinges on the cancer’s type and stage, alongside the patient’s health status.
Surgical Approaches
Surgery stands as a cornerstone in treating testicular cancer. Several surgical methods are employed, each tailored to the patient’s needs.
Radical Inguinal Orchiectomy
A radical inguinal orchiectomy removes the affected testicle. It serves both as a diagnostic and therapeutic measure.
Retroperitoneal Lymph Node Dissection
Retroperitoneal lymph node dissection (RPLND) involves the removal of lymph nodes in the retroperitoneum. This area is a common site for testicular cancer metastasis.
Radiation Therapy
Radiation therapy employs high-energy rays to destroy cancer cells. It’s commonly used for seminoma, a testicular cancer type. It’s often applied post-surgery to eliminate residual cancer cells.
Chemotherapy Protocols
Chemotherapy uses drugs to target and kill cancer cells. It’s typically employed when cancer has spread beyond the testicles.
Stem Cell Transplantation
Stem cell transplantation involves high-dose chemotherapy followed by stem cell infusion. This helps the bone marrow recover.
Clinical Trials and Emerging Treatments
Clinical trials test new treatments or existing ones in new ways. Participating in a trial offers access to cutting-edge therapies not yet widely available.
Treating testicular cancer is complex, requiring a team effort. Patients should consult with their healthcare provider to choose the most suitable treatment.
Prognosis and Survival Rates
Patients with testicular cancer often look for information on their prognosis and survival rates. Knowing the chances of successful treatment and what affects prognosis helps individuals deal with their diagnosis.
Survival Statistics by Stage
Survival rates for testicular cancer change a lot based on the stage at diagnosis. Generally, the 5-year survival rate is high, mainly for those diagnosed early.
- Localized testicular cancer: 99% 5-year survival rate
- Regional testicular cancer: 96% 5-year survival rate
- Distant testicular cancer: 73% 5-year survival rate
Factors Affecting Prognosis
Several factors impact the prognosis for testicular cancer. These include the type and stage of cancer, and the patient’s overall health. For example, seminoma tends to have a better prognosis than non-seminoma.
Long-term Outlook
The long-term outlook for testicular cancer survivors is generally positive. Most men are cured of their disease. Yet, long-term follow-up is vital to watch for late effects of treatment and any recurrence.
Recurrence Rates and Management
Understanding the risk of recurrence and how it’s managed is key for long-term survival. Regular follow-up appointments and self-examinations are essential for monitoring for recurrence.
Managing Side Effects of Treatment
Managing the side effects of testicular cancer treatment is vital for patients’ recovery and well-being. Treatments like surgery, radiation, and chemotherapy can lead to various side effects. These can significantly impact a patient’s quality of life.
Physical Side Effects
Physical side effects from testicular cancer treatment vary based on the treatment type. They can be divided into short-term and long-term effects.
Short-term Side Effects
- Fatigue
- Nausea and vomiting
- Hair loss
- Skin reactions
Long-term Side Effects
- Infertility
- Cardiovascular problems
- Secondary cancers
- Neuropathy

Emotional and Psychological Impact
Testicular cancer treatment also affects patients emotionally and psychologically. Anxiety, depression, and stress are common among those undergoing treatment.
Strategies for Coping with Side Effects
Several strategies can help patients manage treatment side effects. Maintaining a healthy lifestyle and practicing stress-reducing techniques are key. Seeking support from healthcare professionals, family, and friends is also essential.
Complementary Therapies
Complementary therapies, like acupuncture, massage, and meditation, are vital in managing side effects. They can help alleviate symptoms such as pain, nausea, and fatigue. This improves overall well-being.
Fertility Considerations and Preservation
Diagnosis with testicular cancer raises a critical concern for men: its impact on fertility. The disease and its treatments can severely affect a man’s ability to conceive. This makes fertility preservation a vital consideration for those facing this diagnosis.
Impact of Testicular Cancer on Fertility
Testicular cancer and its treatments, such as chemotherapy and radiation, can harm fertility. They can damage sperm or disrupt hormone production. It’s vital to understand these risks to make informed decisions about preserving fertility.
Sperm Banking and Preservation Options
Sperm banking, or cryopreservation, is a common method for preserving fertility. It involves freezing sperm for future use in assisted reproductive technologies. Men diagnosed with testicular cancer are advised to consider sperm banking before undergoing treatments that could harm their fertility.
Assisted Reproductive Technologies
For men who have banked sperm, assisted reproductive technologies (ART) like in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) offer pathways to parenthood. These technologies have seen significant advancements, providing hope for men facing fertility challenges due to testicular cancer.
Parenthood After Testicular Cancer
Many men treated for testicular cancer go on to become fathers. Advances in fertility preservation and ART have made parenthood more accessible. It’s essential for men to discuss their fertility concerns and options with their healthcare provider to make informed decisions about their future.
Living with Testicular Cancer
Living with testicular cancer is a complex journey. It involves medical treatments, personal challenges, and support systems. This journey impacts not just the patient but also their loved ones.
Psychological and Emotional Support
Receiving a testicular cancer diagnosis can be emotionally overwhelming. Patients often face anxiety, depression, and stress. It’s vital to seek psychological support to cope with these emotions.
- Counseling or therapy sessions offer a safe space to express feelings and concerns.
- Support groups, whether online or in-person, connect patients with others facing similar experiences.
- Mindfulness and relaxation techniques, like meditation or yoga, help manage stress and anxiety.
Impact on Relationships and Intimacy
Testicular cancer can strain relationships with family, friends, and romantic partners. Open communication is essential for maintaining healthy relationships during this challenging time.
Intimacy may be affected, but facing cancer together can also strengthen relationships.
Support Groups and Resources
Support groups and resources are vital in the cancer journey. They offer a sense of community and provide valuable information.
Returning to Work and Normal Activities
Returning to work and resuming normal activities is a significant step in recovery. It’s important to listen to your body and not rush back too quickly.
- Discuss your return to work plan with your healthcare provider.
- Consider a gradual return to work, starting with part-time hours or modified duties.
- Communicate your needs and any necessary accommodations to your employer.
Financial Considerations and Insurance
The cost of cancer treatment can be substantial. Understanding your insurance coverage and exploring financial assistance options is critical.
- Review your insurance policy to understand what is covered and what is not.
- Look into financial assistance programs offered by cancer organizations.
- Discuss financial concerns with your healthcare team to find solutions.
Living with testicular cancer requires a holistic approach. This includes medical treatment, emotional support, and practical considerations. By utilizing available resources and support systems, patients can better navigate this challenging journey.
Prevention and Risk Reduction
While testicular cancer can’t be fully prevented, knowing the risks and making healthy choices can help spot it early. Awareness and education are vital in preventing and reducing the risk of testicular cancer.
Preventive Measures
Though there’s no guaranteed way to prevent testicular cancer, some steps can help in early detection. Regular self-exams are key to spotting any unusual changes in the testicles.
- Perform monthly self-exams to check for any unusual changes.
- Be aware of the risk factors, including family history and previous testicular cancer.
- Understand that certain medical conditions, such as undescended testes, increase the risk.
Healthy Lifestyle Choices
Healthy lifestyle choices can boost overall health and might lower the risk of testicular cancer.
- Maintain a balanced diet rich in fruits, vegetables, and whole grains.
- Exercise regularly to promote overall health and well-being.
- Avoid smoking and limit alcohol consumption.
Awareness and Education
Awareness and education are critical for early detection and management of testicular cancer. Learning about signs, symptoms, and risk factors can lead to timely medical interventions.
Advocating for Men’s Health
Advocacy for men’s health, including testicular cancer, is key for awareness and research support. Encouraging open discussions about men’s health can help reduce stigma and promote early detection.
The Future of Testicular Cancer Care
The field of testicular cancer care is rapidly evolving, thanks to breakthroughs in medical research and technology. Looking ahead, there’s a focus on creating treatments that are more precise and effective. These treatments aim to reduce side effects while boosting patient outcomes.
Researchers are now exploring new biomarkers for testicular cancer. This could mean earlier detection and more tailored treatment plans. The introduction of immunotherapy and precision medicine also shows great promise. These approaches could significantly improve survival rates and the quality of life for testicular cancer patients.
The future of cancer care, including testicular cancer, will likely be more integrated. It will draw on genetics, genomics, and data analytics to personalize treatments. As research progresses, we can look forward to better diagnostic tools and more effective treatments. This will greatly enhance the care and support for those dealing with testicular cancer.
FAQ
Q: What is testicular cancer?
A: Testicular cancer is a form of cancer that occurs in the testicles. These are key parts of the male reproductive system.
Q: What are the risk factors for testicular cancer?
A: Several factors increase the risk of testicular cancer. These include age, family history, and genetic predisposition. Certain medical conditions, like cryptorchidism, also play a role.
Q: What are the symptoms of testicular cancer?
A: Symptoms of testicular cancer include a noticeable lump or swelling in the testicle. Pain or discomfort in the testicle or scrotum is also common. A feeling of heaviness in the scrotum is another symptom.
Q: How is testicular cancer diagnosed?
A: Diagnosing testicular cancer involves a physical exam and ultrasound. Blood tests for tumor markers and imaging studies are also used.
Q: What are the treatment options for testicular cancer?
A: Treatment for testicular cancer varies based on the cancer’s stage and type. Options include surgery, radiation therapy, chemotherapy, and stem cell transplantation.
Q: Can testicular cancer be cured?
A: Yes, testicular cancer is highly treatable. The cure rate is generally high, provided it’s caught early.
Q: How can I reduce my risk of testicular cancer?
A: While preventing testicular cancer is not possible, a healthy lifestyle can help. Being aware of risk factors and doing regular testicular self-exams aid in early detection.
Q: What is the impact of testicular cancer on fertility?
A: Testicular cancer and its treatment can impact fertility. Yet, options like sperm banking and assisted reproductive technologies can help preserve fertility.
Q: Are there support resources available for testicular cancer patients?
A: Yes, numerous support groups, resources, and organizations exist. They offer emotional, psychological, and practical support to testicular cancer patients.